Is Transoesophageal Echocardiography Necessary for the Percutaneous Management of Lutembacher Syndrome: A Case Report
Vamsi Krishna Kamana1, Ranjan Shetty2, Anand Muthu Krishnan3, Ravella Keerthika Chowdary4, Umesh Pai Malpe5
1 Fellow, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Professor, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Intern, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Resident, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Assistant Professor, Department of CVT, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:Dr. Vamsi Krishna kamana, Fellow, Department of Cardiology, KMC, Manipal, Udupi- 576104, Karnataka, India.
E-mail: drvamsikrishna2k@gmail.com
Lutembacher syndrome is defined as a combination of congenital Atrial Septal Defect (ASD) with an acquired Mitral Stenosis (MS). There are various challenges involved in the percutaneous management of Lutembacher syndrome. Here, we present a case that had a very small Left Atrium (LA) and Left Ventricle (LV) cavities with an anteriorly placed ASD. We used Transoesophageal echocardiography (TEE) to take a separate interatrial septal puncture and complete the Balloon Mitral Valvotomy (BMV) procedure. Finally both the defects in interatrial septum were closed with the help of a large device.
Atrial septal defect, Balloon mitral valvotomy, Inoue balloon, Interatrial septal puncture
Case Report
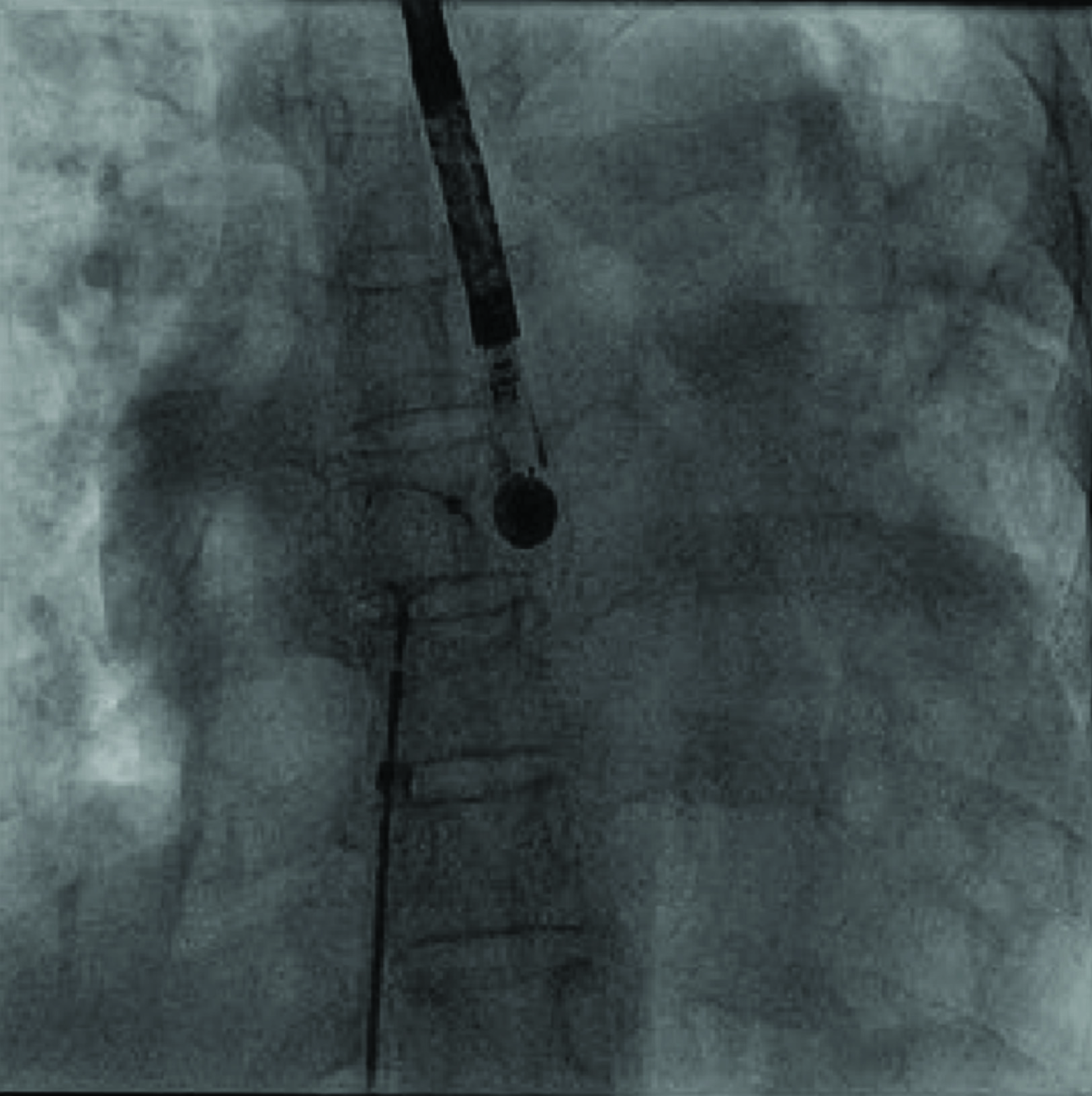
A 36-year-old female with a history of dyspnea on exertion (NYHA Class II) for past 6 months presented with exacerbation since 4 days (New York Heart Association - NYHA Class III-IV). She also had a history of orthopnea and paroxysmal nocturnal dyspnoea. There was no history of accompanying chest pain, cough, palpitations, fever, or any other symptoms of upper respiratory infections. She was a known case of Rheumatic heart disease on Penicillin prophylaxis and Rheumatic arthritis. On brief physical examination at our hospital, she was afebrile with normal volume regular pulse of 80beats/min and blood pressure 110/70mm of Hg, with respiratory rate of 20breaths/min. There was no pallor or any signs of pedal oedema. On cardiac examination, the apex is right ventricular type and was situated in the left 5th inter coastal space at mid clavicular line, parasternal heave was present, there was a palpable P2, ejection systolic murmur grade 4/6 was heard in the left clavicular area and so was a loud P2. Respiratory system examination revealed bilaterally diffuse rhonchi. Abdominal examination revealed no hepatomegaly. Electrocardiogram (ECG) showed sinus tachycardia with prominent P waves, incomplete right bundle branch block and right axis deviation. A 2D Echocardiography showed severe mitral stenosis with mild mitral regurgitation and mitral valve area 1.12-1.2 cm2. A large 24mm Ostium Secondum Atrial Septal Defect (OS ASD) with a left to right shunt [Table/Fig-1] was present. The right atrium /right ventricle were dilated with mild tricuspid regurgitation and good LV function. This confirmed the diagnosis of Lutembacher Syndrome. Initially Balloon Mitral Valvotomy (BMV) was tried with a 26mm inoue balloon, which failed to cross the Mitral Valve (MV). We felt the failure is due to the small left atrium, which is causing difficult manipulations in left atrium cavity. Trans Oesophageal Echocardiography (TEE) was used all throughout the procedure for interatrial septal puncture to complete BMV and also to guide device closure [Table/Fig-2]. BMV was done on 28/12/15 [Table/Fig-3]. ASD device closure was done with a 30mm COCOON on 28/12/15 [Table/Fig-4]. Post-operatively the patient was managed with diuretic Furesemide. There was no evidence of a clot or pericardial effusion. Her medications were optimized and she was informed about her medical condition and the prognosis and was discharged. She was asked to report immediately in case of any chest discomfort, breathlessness, giddiness. A follow-up 40 days showed good general condition and no symptoms.
Image showing the native OS ASD located antero-superiorly
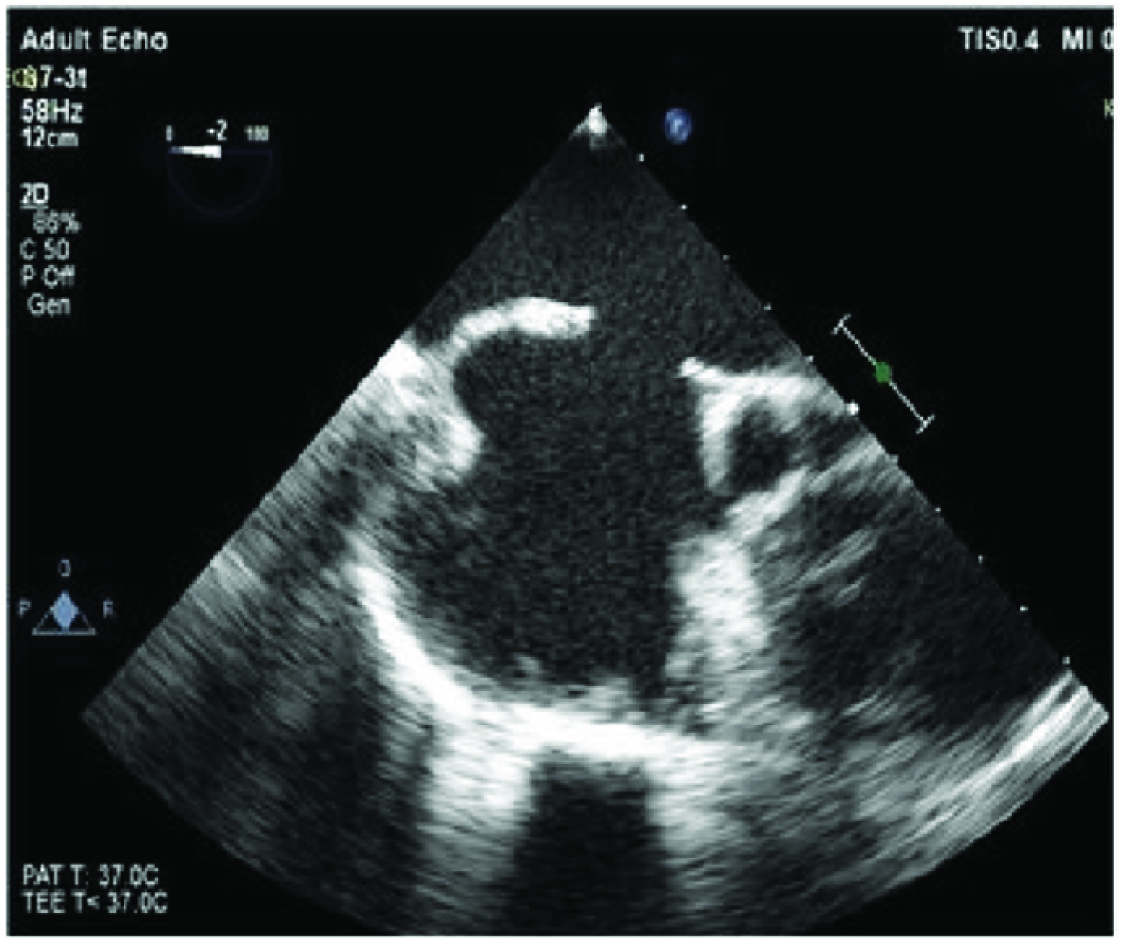
Image showing the TEE assisted septal puncture posteriorly
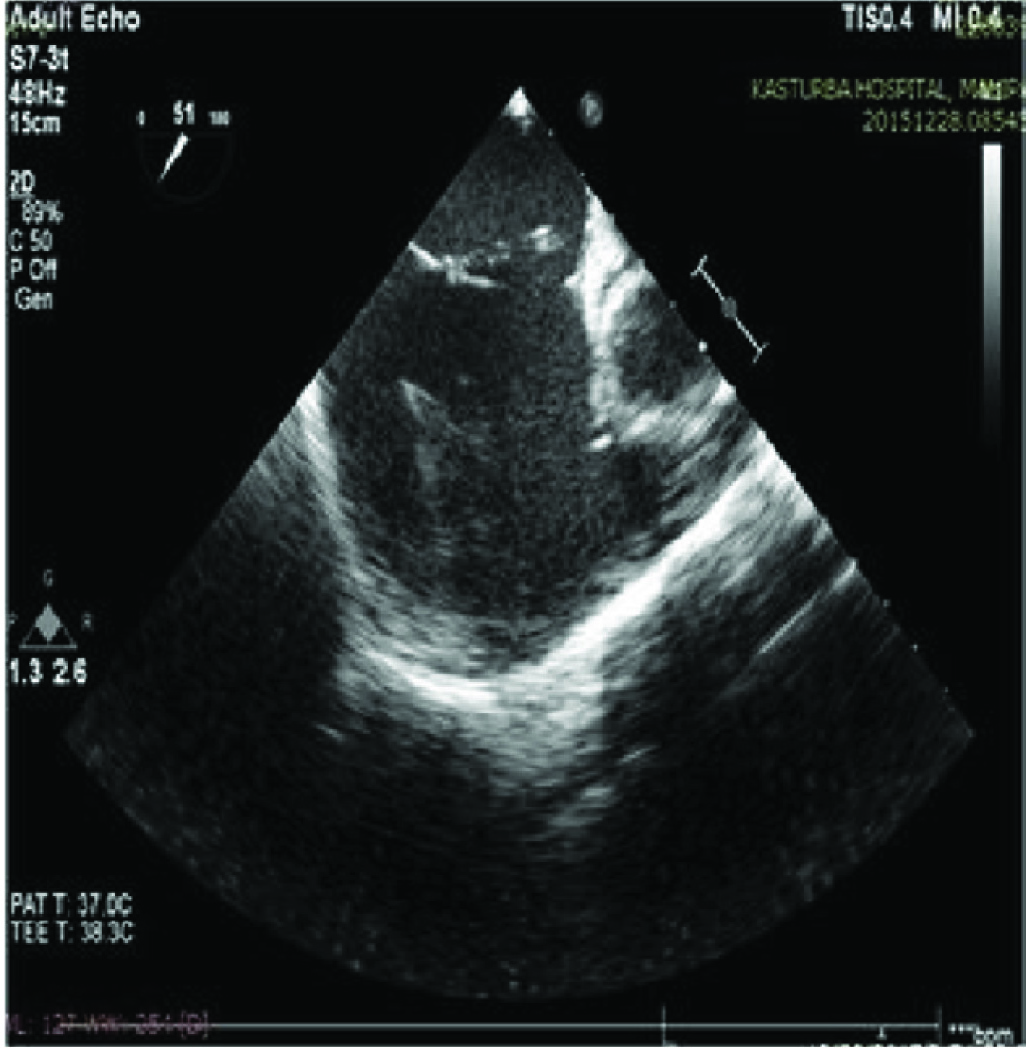
Image showing BMV done with 26mm Inoue balloon with TEE guidance.
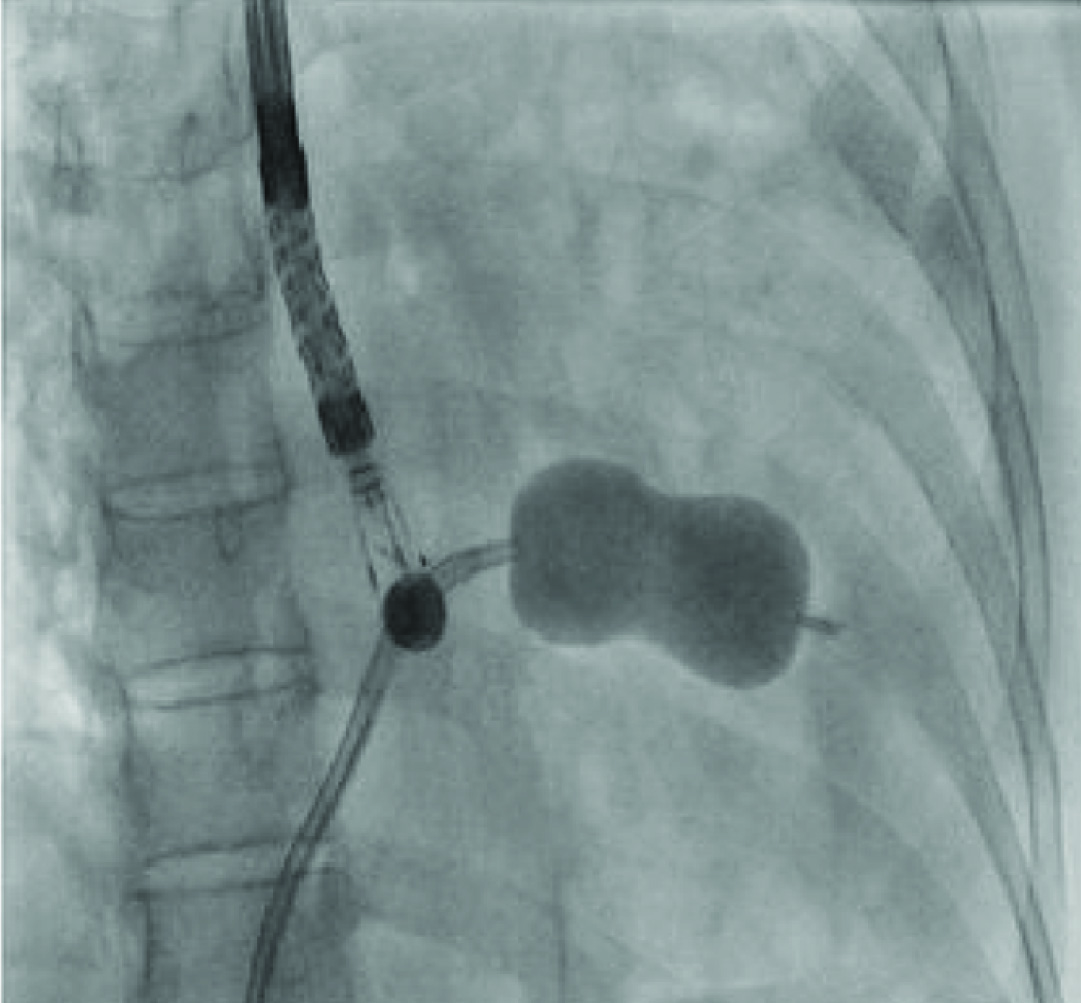
Image showing ASD close with a 30mm Cocoon ASD Septal Occluder with TEE support.
Discussion
Lutembacher’s syndrome is a combination of congenital Atrial Septal Defect (ASD) with acquired Mitral Stenosis (MS) [1]. Lutembacher syndrome has predisposition for women as MS and ASD are more frequently observed in women. Approximately 4% cases of MS are seen in patients with ASD, whereas 0.6-0.7% of ASD cases is seen in patients with MS [2]. The percutaneous management of lutembacher is challenging for each case to case. Because lutembacher is characterized anatomically by small sized left atrium and mitral valve stenosis and the right atria is larger than left atria. This makes the inoue balloon manipulation difficult during BMV.
Percutaneous treatment in a patient with Lutembacher syndrome was first performed in 1992 by Ruiz [3]. The success rate for complete closure rate of ASD by the septal occluder device was found to be upto 93-97% [4]. The most important complication during the procedure is embolization of the septal occluder device [5]. In a study by Chen CR et al., the success rate of percutaneous intervention for BMV by the trans-septal inoue balloon technique was 99% [6]. The life threatening complication rate (death and stroke) was very low (0-0.5%) and the risk of developing severe complications like (3-4 degree MR, cardiac tamponade, thromboembolism) was found to be lower with inoue balloon technique when compared to the other procedures of BMV [7].
In patients with Lutembacher syndrome, the combined percutaneous treatment techniques BMV and device closure, have reported to reduce the mortality and morbidity risk associated with cardiac surgery and reduce the surgery- related length of hospital stay [8]. BMV may be performed in these patients when there is recurrence of severe mitral stenosis by using the retrograde non trans-septal approach. Here the transarterial technique approach is done by passing from the left ventricle into the left atrium and BMV is completed [9]. Here, this case highlights the importance of TEE in assisting septal puncture at a posteroinferior location, despite the native anatomical defect located anterosuperiorly and also TEE during the anatomical closure of the ASD. Despite limited literature, our experience in this case shows that treatment done using the combined catheter technique with help of TEE can be performed safely and successfully without the need for open heart surgery.
Conclusion
Always plan the intervention on Lutembacher syndrome with a thorough echocardiographic imaging. TEE helps in difficult septal punctures. A small sized left atrium and left ventricle in cases of Lutembacher syndrome will cause difficulty while manipulating the inoue balloon across the mitral valve. There is difficulty in passing inoue balloon across the mitral valve in the presence of high and anteriorly located ASDs. A TEE guided separate inter-atrial septal puncture is the best solution for performing the BMV successfully. TEE guidance is also helpful in the closure of these difficult or large ASDs eg., anterior, superior defects.
[1]. Perloff JK, Atrial septal defectIn: The clinical recognition of congenital heart disease 1994 4th edPhiladelphiaW. B. Saunders:233-99. [Google Scholar]
[2]. Vasan RS, Shrivastava S, Kumar MV, Value and limitations of doppler echocardiographic determination of mitral valve area in Lutembacher syndromeJ Am Coll Cardiol 1992 20:1362-70. [Google Scholar]
[3]. Ruiz CE, Gamra H, Percutaneous closure of a secundum atrial septal defect and double balloon valvotomies of a severe mitral and aortic valve stenosis in a patient with Lutembacher’s syndrome and severe pulmonary hypertensionCathet Cardiovasc Diagn 1992 25:309-12. [Google Scholar]
[4]. Thanopoulos BD, Laskari CV, Tsaousis GS, Zarayelyan A, Closure of atrial septal defects with the amplatzer occlusion device: preliminary resultsJ Am Coll Cardiol 1998 31:1110-16. [Google Scholar]
[5]. Wilson NJ, Smith J, Prommete B, O’Donnell C, Transcatheter closure of secundum atrial septal defects with the Amplatzer septal occluder in adults and children -follow-up closure rates, degree of mitral regurgitation and evolution of arrhythmiasHeart Lung Circ 2008 17:318-24. [Google Scholar]
[6]. Chen CR, Cheng TO, Percutaneous balloon mitral valvuloplasty by the Inoue technique: a multicenter study of 4832 patients in ChinaAm Heart J 1995 129:1197-203. [Google Scholar]
[7]. Cheng TO, Holmes DR, Percutaneous balloon mitral valvuloplasty by the Inoue balloon technique: the procedure of choice for treatment of mitral stenosisAm J Cardiol 1998 81:624-28. [Google Scholar]
[8]. Cheng TO, Coexistent atrial septal defect and mitral stenosis (Lutembacher syndrome): An ideal combination for percutaneous treatmentCatheter Cardiovasc Interv 1999 48:205-06. [Google Scholar]
[9]. Stefanadis CI, Stratos CG, Lambrou SG, Bahl VK, Cokkinos DV, Voudris V, Retrograde nontransseptal balloon mitral valvuloplasty: immediate results and intermediate long-term outcome in 441 cases-a multicenter experienceJ Am Coll Cardiol 1998 32:1009-16. [Google Scholar]