Osteomyelitis in Pycnodysostosis – Report of 2 Clinical Cases
Rohit S.1, Praveen Reddy B.2, Sreedevi B.3, Sandeep Prakash4
1Reader, Department of Oral and Maxillofacial Surgery, Rajarajeswari Dental College and Hospital, Bangalore, India.
2Professor & Head, Department of Oral and Maxillofacial Surgery, Government Dental College, RIMS, Imphal, India.
3Reader, Department of Oral Medicine and Radiology, Hitkarini Dental College and Hospital, Jabalpur, India.
4Reader, Department of Oral and Maxillofacial Surgery, Triveni Institute of Dental Sciences, Bilaspur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rohit S., #1348, Sai Kuteera, TF-7, Chikkallasandra, Bangalore – 560061, India.
E-mail: rohit.srikanthan@gmail.com
Pycnodysostosis is a rare craniofacial syndrome characterized by dwarfism, cranial anomalies, diffuse osteosclerosis where multiple fracture of long bones and osteomyelitis of jaw are frequent complications. This clinical entity was first described in 1962 by Maroteaux and Lamy. This article presents two clinical cases of pycnodysostosis with their clinical and radiological characteristics.
Osteomyelitis, Pycnodysostosis, Pathological fracture
Case Report
We present two clinical cases of patients attending the Oral Surgery Unit, who presented clinical and radiographic characteristics typical of pycnodysostosis.
Case 1
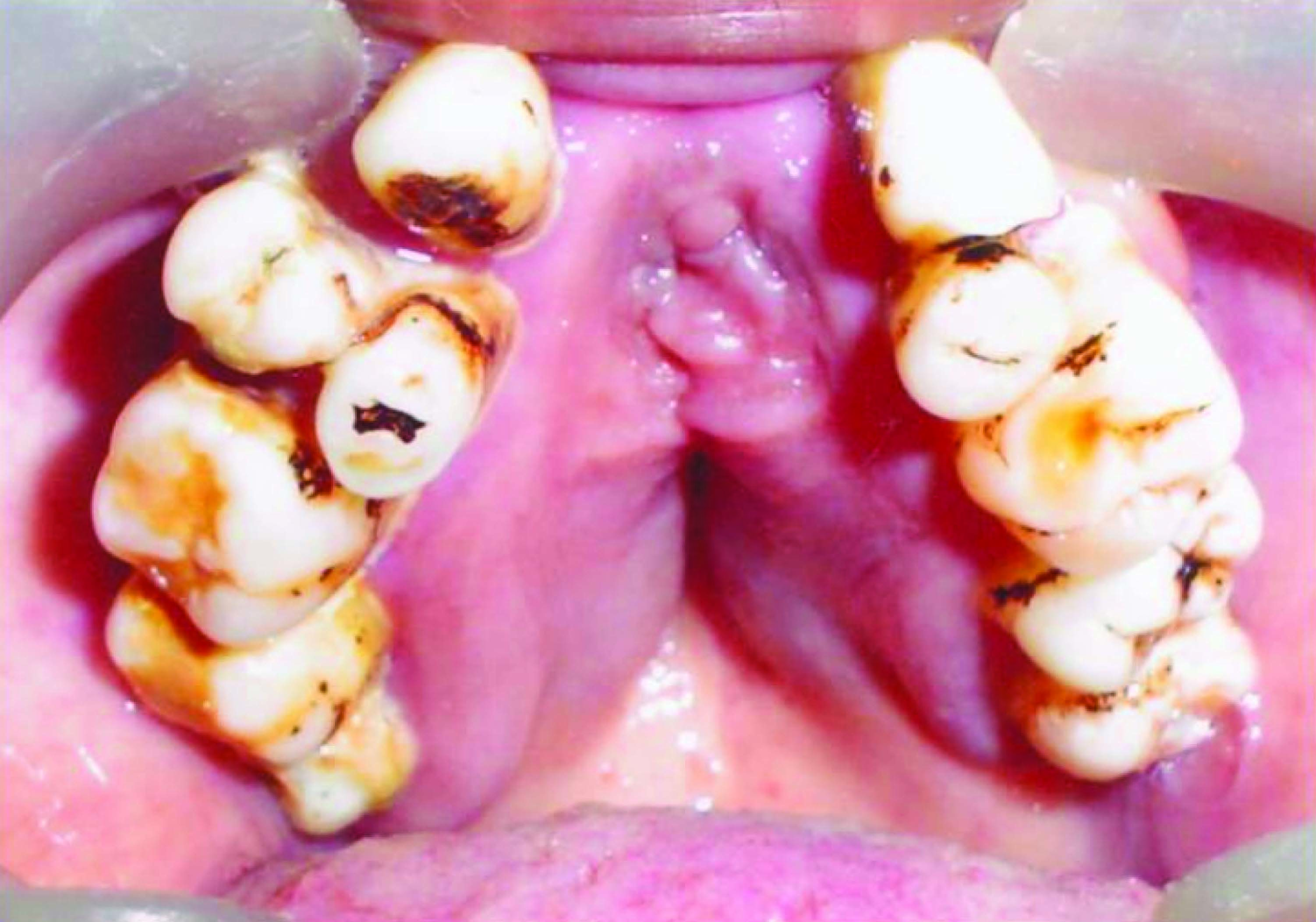
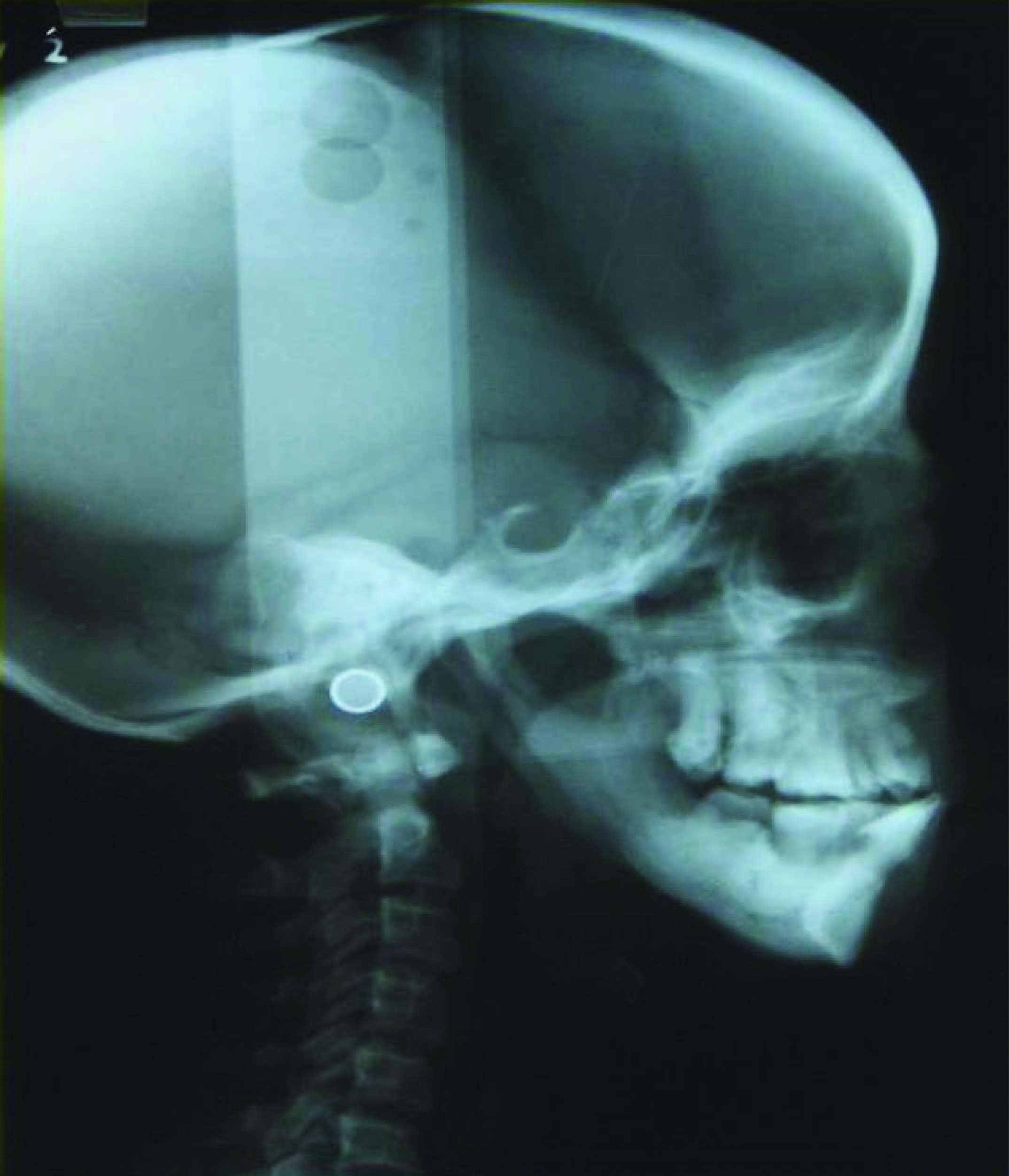
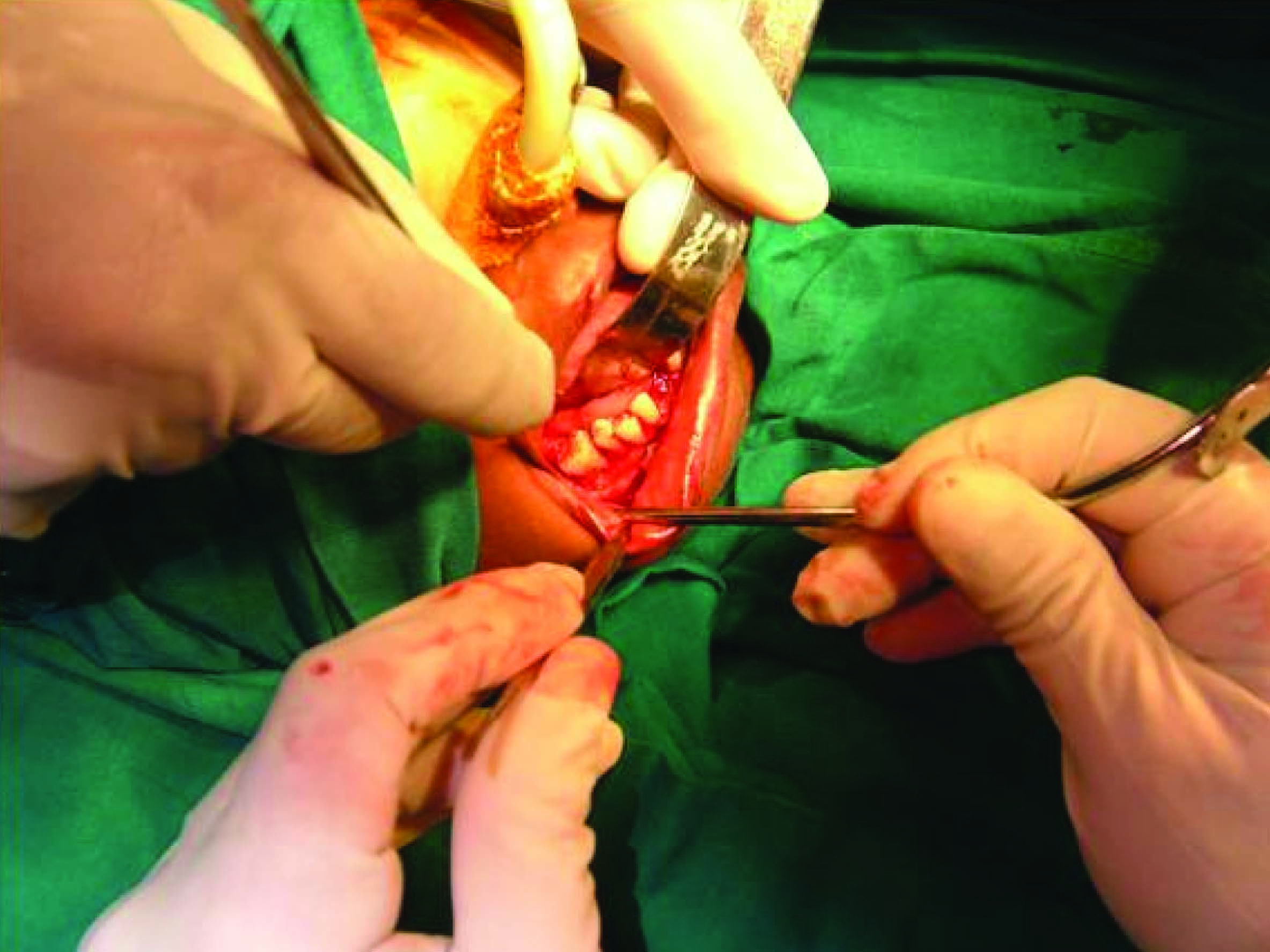
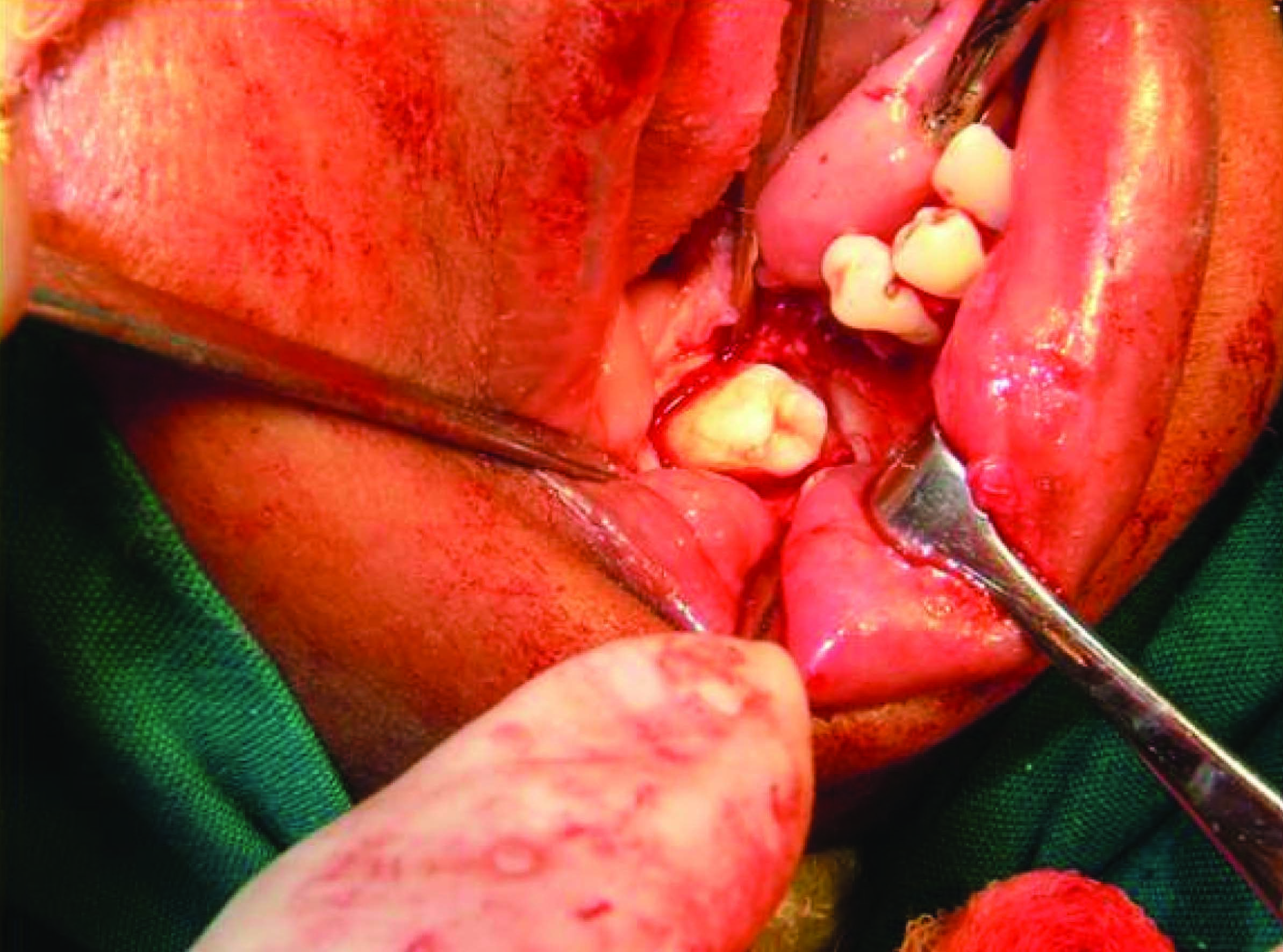
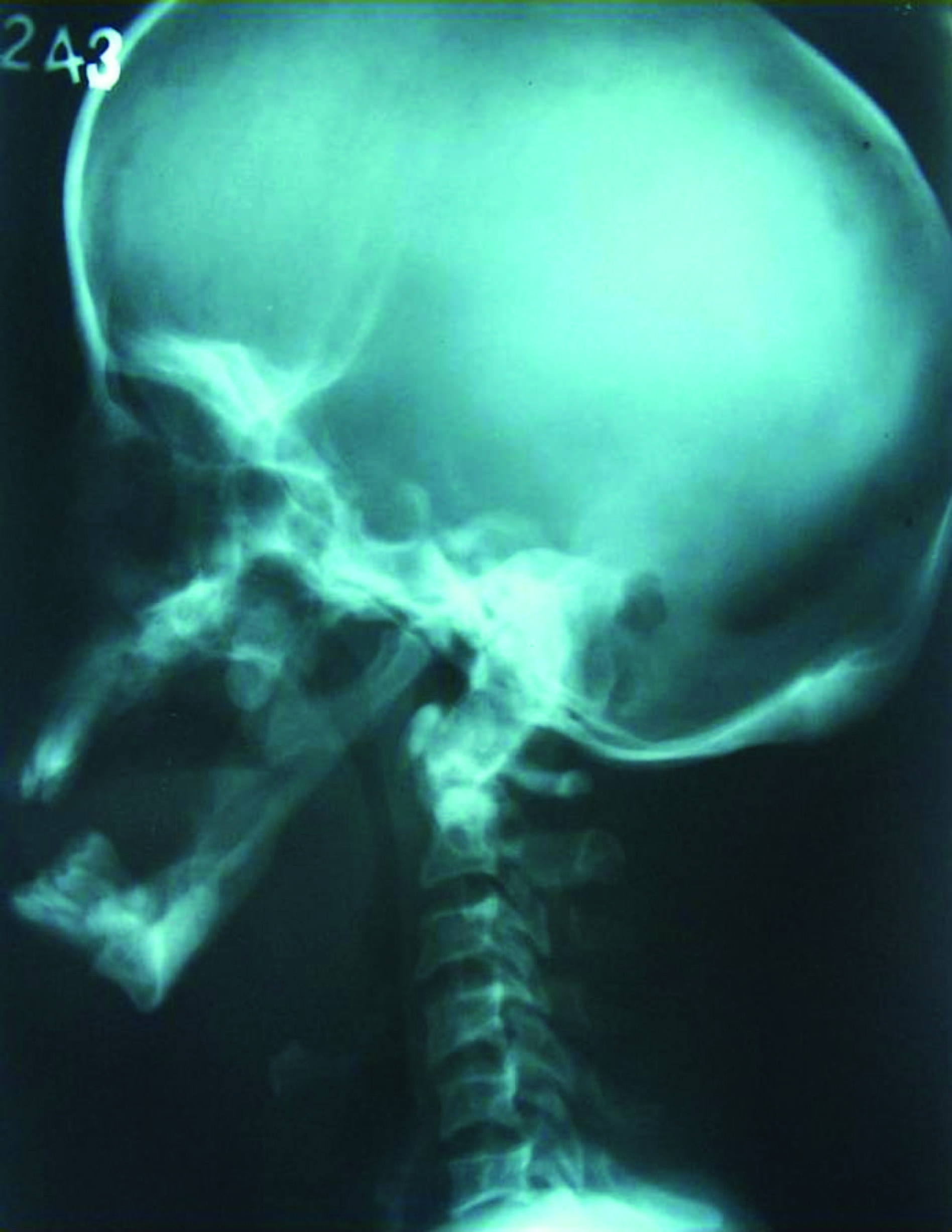
A 40-year-old female patient reported to our unit with a wound on right side of lower jaw since 6 months [Table/Fig-1]. Patient gives a history of swelling in the same region 6 months back followed by pus discharge. She was treated by a local doctor with Tab. Metronidazole for a week. She complains of frequent discharge from the same site in the last two months. Her family history reveals consanguineous marriage between her parents. Her brother and paternal aunt were also having a short stature. General examination revealed short stature, short stubby fingers & toes, webbing of 2nd & 3rd digit of toes [Table/Fig-2,3]. Patient’s height was 4 feet and 3 inches and weight was 47Kgs. Extraorally there was a draining sinus on the right lower border of the mandible. Extra oral examination revealed exopthalmous & slanting of eyes [Table/Fig-4]. Intraoral examination revealed partially edentulous dentition with missing 11, 12, 21, 22, 24, 32, 38, 43, 47 and 48, grooving of palate [Table/Fig-5], narrow maxillary and mandibular arches, vestibular tenderness irt 46 and Impacted 47. The orthopantomograph [Table/Fig-6] revealed thin mandible, obtuse angle of mandible, Osteomyelitis in relation to 46 and 47. The lateral skull view [Table/Fig-7] revealed typical hockey stick mandible. Based on history, clinical and radiological features, a diagnosis of Pycnodysostosis and chronic osteomyelitis in relation to 46 and 47 was made. Informed consent was taken from the patient prior to surgery. The treatment was planned for surgical removal of 46 and 47 and decortication [Table/Fig-8,9,10]. The patient was started on intravenous Amoxycillin 500mg and Metronidazole thrice daily preoperatively. The patient was taken for surgery under general anaesthesia. Surgical removal of 46 and 47 was done. Decortication of the buccal cortex in relation to 46 and 47 was performed. The surgical site was irrigated with Metronidazole and primary closure was done using 3-0 vicryl. Postoperatively patient was asked to continue oral amoxicillin and metronidazole for three weeks. Postoperatively healing was uneventful.
Case 2
A 36-year-old male patient reported to our unit with a discharge below the left eye since 2½ months [Table/Fig-11] and a hypomobile mandible. Patient gives a history of swelling on the left side of the face since three months followed by extraoral pus discharge since 21/2 months. General examination revealed short stature, short stubby fingers and toes. The extraoral examination revealed facial dysmorphia, limited mouth opening and pain at the point of fracture of mandible. The intraoral examination revealed partially edentulous dentition with missing 16, 17, 18, 24, 25, 26, 27, 32, 35, 36, 37, 38, 42, 47 and 48, malposed teeth, narrow maxillary and mandibular arches, grooving of palate and pus discharge in relation to 27 [Table/Fig-12,13] and chronic periodontitis. The orthopantomograph revealed obtuse angle of mandible and pathological fracture of the left ramus of the mandible. The mandibular condyles and coronoid apophyses were elongated [Table/Fig-14]. The lateral skull view [Table/Fig-15] revealed typical hockey stick appearance of mandible. Based on history, clinical and radiological features, a diagnosis of Pycnodysostosis with pathological fracture of left ramus of the mandible and chronic osteomyelitis in relation to 27 was made. Informed consent was taken from the patient prior to surgery. The patient was started on intravenous Amoxycillin 500mg and Metronidazole thrice daily preoperatively. The patient was taken for surgery under general anaesthesia. The treatment involved mandibular setting and osteosynthesis, extraction of 27 and curettage. Postoperatively patient was asked to continue oral amoxicillin and metronidazole for three weeks. Postoperatively healing was uneventful.
Discussion
Pychnodysostosis is a rare, recessive, autosomal disease belonging to the group of bone dysplasias. Parental consanguinity is considered as the main aetiology [1].
Pycnodysostosis is a rare sclerosing bone disorder in which osteomyelitis of jaws is a frequent complication. Treatment of osteomyelitis of jaws in pycnodysostosis is difficult and may lead to large resections [2]. Pycnodysostosis a variant of osteopetrosis, occurs only in dwarfs and is characterised by increased density of bone which may lead to increase susceptibility to fracture and inflammatory disease [3].
The sclerosing activity of pycnodysostosis is due to a genetic defect located on chromosome 1q21. This anomaly consists of 12 different mutations [4,5] that produce mutational changes in a lysosomal cystine protease, cathepsin K, the expression of which is reduced in the osteoclasts of these patients [4-7]. This protease is responsible for degrading collagen type 1, that constitutes 95% of the organic bone matrix. The diagnosis of pycnodysostosis has been reported in patients from the age of 9 mnth to adults of 77 y of age. Helfrich asserts that in diseases where the formation and function of the osteoclasts is reduced, as is the case with pycnodysostosis, dental eruption is affected [8]. There may be dental abnormalities, with hypoplasia of the enamel, obliterated pulp chambers and hypercementosis. Protrusion of the incisors with anterior open bite may be found, and dental crowding associated with extensive caries and periodontitis is frequent. These conditions cause the premature loss of dentition that may already be complete by the fourth decade of life [9].
Osteomyelitis and pathological fracture of jaw is commonly seen in patients with pycnodysostosis. The gradual elimination of medullary spaces that occurs with the normal ageing process, coupled with increased endosteal bone production is inherent with this disease. The risk of osteomyelitis is also increased because of the decrease in vascularity and subsequent compromise of the patient’s local immune defences. Lack of follow up care leaves the question of whether the management, or lack of it, was responsible for development of osteomyelitis. Close and long term follow up is required in these patients. Thorough clinical evaluation has to be done before arriving at a treatment plan. Tooth extraction in patients who suffer from pycnodysostosis demands certain special care, such as carrying out the surgery as atraumatically as possible and with proper asepsis, due to the risk of fracture, especially in the mandible [9]. In addition, the greater bone density increases the probability of developing post extraction osteomyelitis [3]. Extractions of teeth are to be taken up under strict antibiotic cover. Hyperbaric Oxygen Therapy can be given when necessary. Conservative management with Decortication and Saucerization would be the best choice of treatment. Prophylactic Resection should be considered when sclerotic areas are still present after sequestrectomy. Bone grafting in these patients may leave a weak donor site which may lead to pathological fracture. The differential diagnosis of pycnodysostosis is established with osteopetrosis, cleidocranial dysplasia and idiopathic acroosteolysis. In osteopetrosis the bone marrow may be absent; it is therefore frequent for hematopoietic alterations to appear. Signs of compression of the cranial nerves exist such as facial paralysis, deafness or pain. Cranial dysplasia may seem like pycnodysostosis for presentation of agenesis or clavicular aplasia, as well as alterations of the skeletal bone membranes, however, bone density is not increased. In idiopathic acroosteolysis, the appearance of the patients is typical, with hypotelorism, exophthalmos and an upturned nose. The angle of mandible is acute and increased bone density is not present [9].


Webbing of 2nd and 3rd digits

Exopthalmous and slanting of eyes

Orthopantomograph showing osteomyelitis irt 46 and 47

Lateral skull view showing hockey stick mandible
Intraoperative view showing extraction of 46
Intraoperative view showing surgical removal of 47 and decortication
1 week postoperative healing of surgical site

Extraoral pus discharge in left infraorbital region

Extraoral view showing features of pycnodysostosis

Grooving of palate and pus discharge irt 27

Orthopantomograph showing osteomyelitis irt 27 and pathological fracture of left ramus of mandible with elongated condyle and coronoid apophyses

Lateral skull view showing hockey stick mandible
Conclusion
Pycnodysostosis is associated with osteosclerosis. As the bone in these patients is very brittle, extraction of teeth should be done under strict asepsis and suitable cover of antibiotics as they are prone to develop osteomyelitis postoperatively. Conservative management of osteomyelitis with Decortication and Saucerization would be the best choice of treatment. Hence identification of this syndrome and a long term follow up protocol is essential to prevent such complications
[1]. RJ Bathi, VN Masur, Pycnodysostosis – A report of two cases with a brief review of literatureInt J Oral Maxillofac Surg 2000 29:439-42. [Google Scholar]
[2]. JP Van Merkesteyn, J Bras, JI Vermeeren, A van der Sar, LW Statius van Eps, Osteomyelitis of jaws in pycnodysostosisInt J Oral Maxillofac Surg 1987 16(5):615-19. [Google Scholar]
[3]. CO Iwu, Bilateral Osteomyelitis of mandible in pycnodysostosis - A case reportInt J Oral Maxillofac Surg 1991 20(2):71-72. [Google Scholar]
[4]. DA Pereira, LB Aytés, CG Escoda, Pycnodysostosis: A report of three clinical casesMed Oral Patol Oral Cir Bucal 2008 13(10):E633-35. [Google Scholar]
[5]. M Donnarumma, S Regis, B Tappino, C Rosano, S Assereto, F Corsolini, Molecular analysis and characterization of nine novel CTSK mutations in twelve patients affected by pycnodysostosisMutation in brief #961. Online. Hum Mutat 2007 28(5):524 [Google Scholar]
[6]. N Fratzl-Zelman, A Valenta, P Roschger, A Nader, BD Gelb, P Fratzl, Decreased bone turnover and deterioration of bone structure in two cases of pycnodysostosisJ Clin Endocrinol Metab 2004 89(4):1538-47. [Google Scholar]
[7]. AT Soliman, MA Ramadan, A Sherif, ES Aziz Bedair, MM Rizk, Pycnodysostosis: clinical, radiologic, and endocrine evaluation and linear growth after growth hormone therapyMetabolism 2001 50(8):905-11. [Google Scholar]
[8]. MH Helfrich, Osteoclast diseases and dental abnormalities Arch Oral Biol 2005 50(2):115-22. [Google Scholar]
[9]. S Landa, S Esteban, E Montes, J Santamaria, A Vitoria, JM Santolaya, Maxillofacial alterations in a family with pycnodysostosisMed Oral 2000 5(3):169-76. [Google Scholar]