Large Solitary Neurofibroma of Face in a Paediatric Patient
Kumar Nilesh1, Ramchandra G Naniwadekar2, Aaditee V Vande3
1 Associate Professor, Department of Oral and Maxillofacial Surgery, School of Dental Sciences, Karad, Maharashtra, India.
2 Professor, Department of Surgery, Krishna Institute of Medical Sciences, Karad, Maharashtra, India.
3 Postgraduate Student, Department of Prosthodontics, School of Dental Sciences, Karad, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kumar Nilesh, Associate Professor, Department of Oral and Maxillofacial Surgery, School of Dental Sciences, Krishna Hospital, Satara, Karad-415110, Maharashtra, India.
E-mail: drkumarnilesh@yahoo.com
Neurofibroma is a rare, benign, neurogenic tumour which may present as multiple lesions as a part of neurofibromatosis syndrome or as a solitary mass. This paper reports a case of large solitary neurofibroma of face in a young female patient. Clinical presentation, imaging characteristics and management of the pathology has been described in detail. The paper also reviews English literature for similar cases.
Maxillofacial, Neurofibromatosis, Neurogenic, Swelling, Tumour
Case Report
A 10-year-old female child was referred to the Department of Oral and Maxillofacial Surgery, Krishna Hospital, Karad, Maharashtra, India for evaluation and management of a painless soft tissue swelling over the left side of face. The parents reportedly first noticed the growth when the child was four-year-old and the swelling had gradually increased to its present size. Patient’s medical history was non contributory. There was no previous history of trauma. On examination, a sagging subcutaneous swelling was noted, extending from left commissure of mouth to the preauricular region. The lesion was about 4 X 7 cm in size and caused drooping of the left corner of the mouth. The overlying skin showed a localized area of hyper pigmentation [Table/Fig-1]. It was soft, non-tender and non-pulsatile. On palpation, the lobulated mass gave a so-called ‘bag of worm’ feeling. There was no neurological disturbance associated with the lesion. Facial nerve weakness and paresthesia over distribution of mental, infraorbital nerve were ruled out. The patient had no similar lesion or area of pigmentation elsewhere on the body.
Clinical presentation of the lesion.

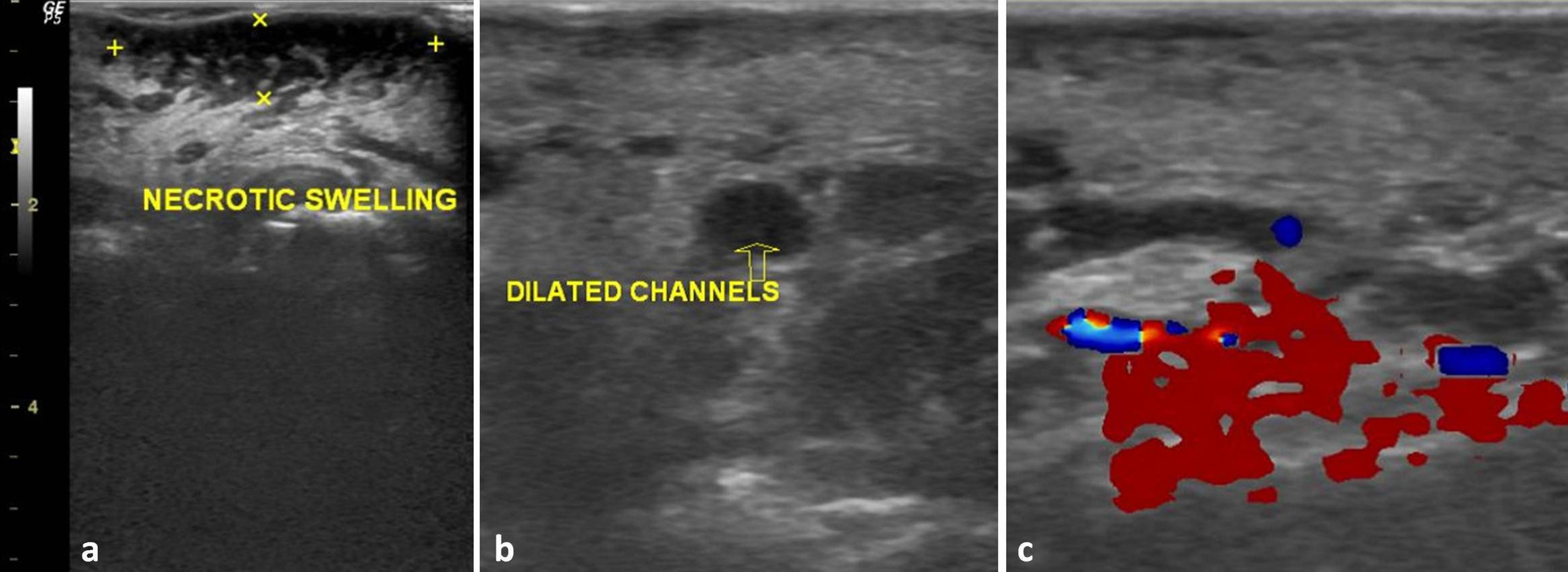
Ultrasonography (USG) of the lesion showed a hypoechoic mass in the subcutaneous plane of buccal space measuring about 7.6 cm cranio-caudally, resting over the buccinator, masseter and orbicularis-oris muscle. Well defined hypoechoic area was noted within the swelling, suggestive of necrotic foci. Multiple dilated channels were seen within the lesion with minimal vascularity on color doppler [Table/Fig-2].
(a) Ultrasonogram showing hypoechoic mass in the subcutaneous plane with necrotic foci; (b) Multiple dilated channels (arrow); (c) With minimal vascularity on color doppler.
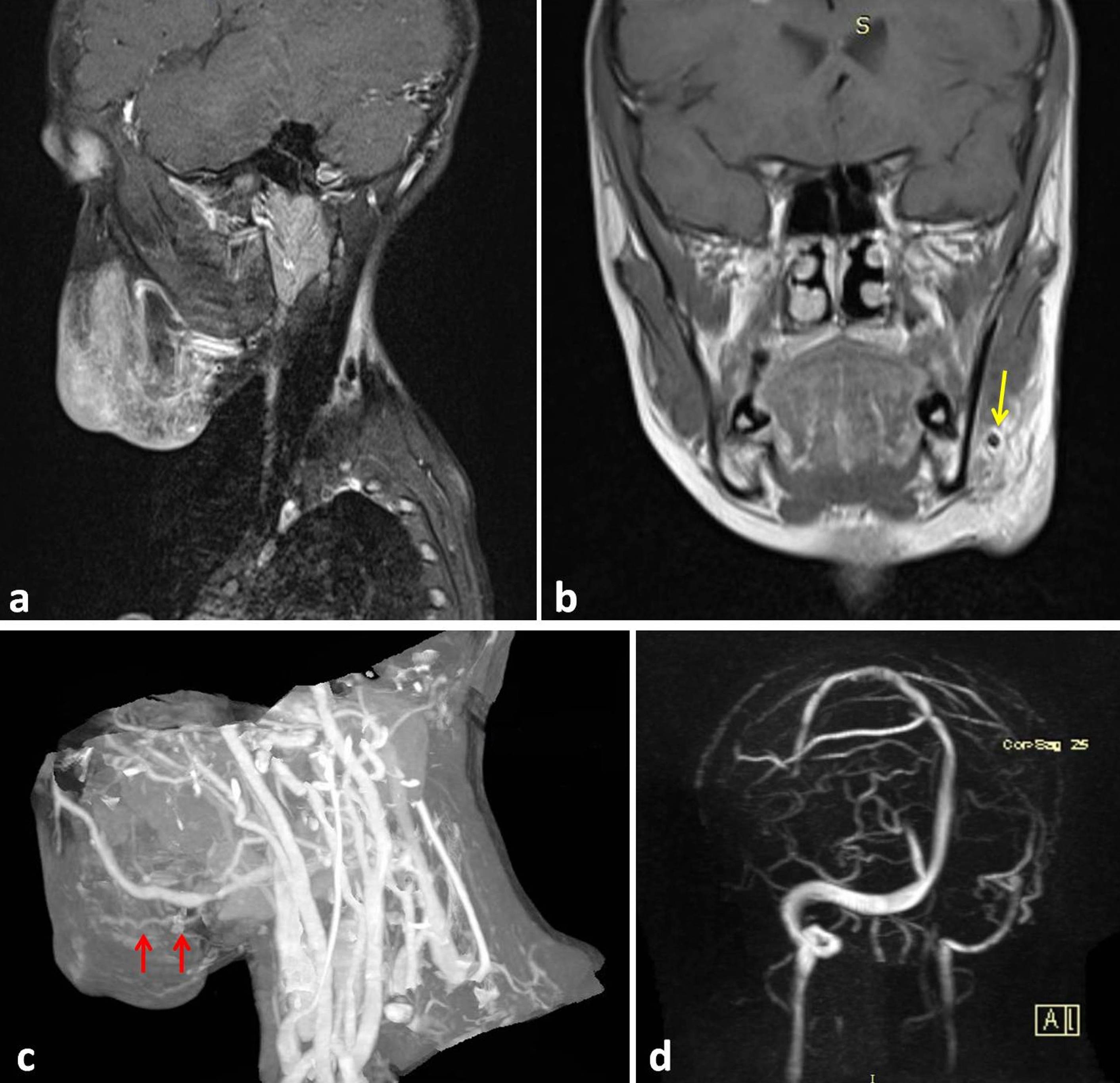
Magnetic Resonance Imaging (MRI) showed a well-defined enhancing lesion (on T2 images) involving the subcutaneous soft tissue plane with contour bulge on left side of the face. Lesion was seen encasing the facial vessels and its branches [Table/Fig-3a,b]. No haemorrhagic or calcification foci were seen within the lesion. Underlying mandible and maxillary bones showed normal morphology. Head and neck angiogram showed the subcutaneous mass being supplied by facial artery. Large, early draining, dilated torturous venous channels were noted within the lesion draining into the external jugular vein on the left side suggestive of shunting of capillary network. The left carotid artery system, including common carotid cervical segment, carotid bifurcation, external and internal carotid artery were normal [Table/Fig-3c,d].
MRI showing an enhancing lesion of left buccal space with contour bulge on skin of face (a); Prominent facial vessel (arrow) and its branches seen within the mass (b). Neck angiogram showing dilated torturous venous channels (arrow) draining into the external jugular vein on the left side (c); Carotid artery system which appear normal bilaterally (d).
The above radiological features were suggestive of non-encapsulated subcutaneous mass with slow flow vascular channels and the differential diagnosis included neurogenic tumour, haemangioma and lipoma. An incision biopsy, carried out under local anaesthesia revealed stratified squamous epithelium and connective tissue on microscopy. The underlying connective tissue showed proliferation of delicate spindle shaped cells with thin wavy nuclei intertwining with connective tissue fibrils [Table/Fig-4a,b]. The features were diagnostic of neurofibroma. Based on the clinical, radiological and microscopic finding a final diagnosis of solitary neurofibroma was established.
(a) Haematoxylin and eosin stained section of photomicrograph showing stratified squamous epithelium and underlying connective tissue (4X magnification); (b) With proliferation of delicate spindle shaped cells with thin wavy nuclei intertwining with connective tissue fibrils (10X magnification).

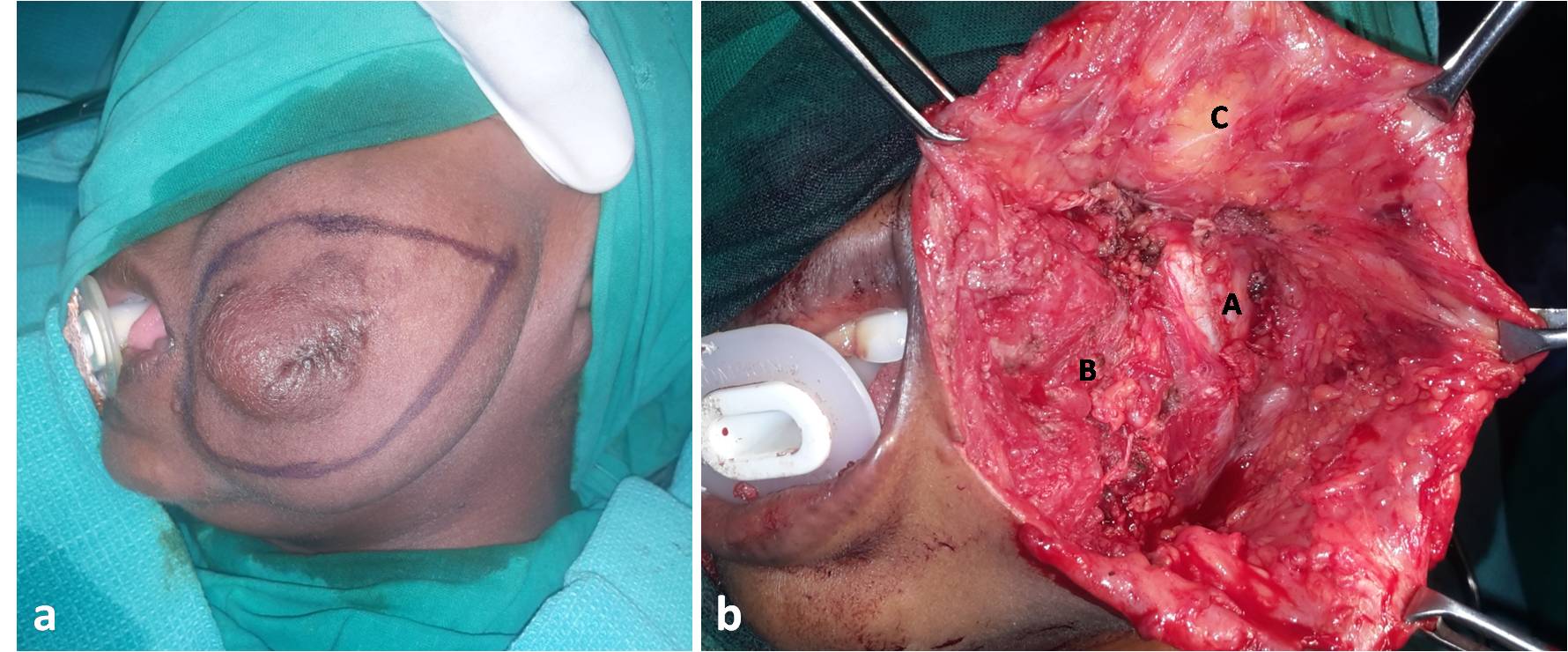
Complete excision of the lesion was planned and executed under general anaesthesia. Incision marking was made to completely excise the lesion and remove the loose extra skin [Table/Fig-5a]. On dissection the lesion was non-capsulated, vascular and without any distinct plane. The vessels encountered in the mass were carefully identified and ligated. The mass was carefully dissected and excised in-toto from the underlying muscle bed of masseter and buccinators muscles [Table/Fig-5b].
(a) Intraoperative photograph showing incision marking; (b) The surgical site after removal of lesion, showing lateral surface of masseter (A) and buccinator (B) Muscle and the raised skin flap (C).
The histopathological features of the excised specimen were consistent with the findings of incision biopsy, confirming diagnosis of neurofibroma. Postoperative period was uneventful and patient was kept on regular follow up. At one year recall the patient showed no clinical evidence of recurrence. The scar line was visible with some amount of contracture. The aesthetic outcome was acceptable at present to the parents and they agreed for scar revision surgery at later date [Table/Fig-6].
One year postoperative picture.

Discussion
Neurofibroma is a benign tumour of neural origin. It is common in head and neck region, accounting for 25% of all neurofibromas [1]. It usually presents as multiple lesions as a part of Neurofibromatosis (NF). Type 1 Neurofibromatosis (NF1) manifests at birth or early childhood and is characterized by multiple areas of hypo- or hyper-pigmented skin called as café-au-lait spots. Multiple subcutaneous lesions called plexiform neurofibromas consisting of proliferating bundles of nerve fibers is pathognomonic of NF1. Type 2 Neurofibromatosis (NF2) is associated with bilateral neurofibromas involving the vestibulocochlear nerve along with hearing and visual disturbances. Solitary Neurofibroma (sNF) is localized single lesion which occurs outside the settings of neurofibromatosis [2,3]. They invariably present as slow growing subcutaneous or submucosal mass. Pain or numbness may occur due to compression of involved nerve. The difference between lesion of sNF and neurofibromatosis is that, NF although unencapsulated has a distinct plane between the lesion and adjacent normal tissue, and the same was also noted in our case.
Although, the incidence of isolated neurofibroma not associated with neurofibromatosis is uncertain, in a review of 43 cases of head and neck neurofibroma, 22 (51.2%) presented as isolated lesion, involving tongue, buccal mucosa, palate, gingiva, maxillary bones, mandible, chin, neck, and salivary gland [4]. Search of English literature from PubMed database, using combination of terms; solitary, neurofibroma and face revealed 14 titles. The papers were further scrutinized and five case reports of neurofibroma of face, which were not part of neurofibromatosis, were identified. These papers were reviewed for demographic details, clinical presentation, duration, location, treatment provided and outcome [Table/Fig-7] [5-9]. Solitary neurofibroma involving face vary from small localized mass to large diffuse lesion occupying almost entire half of the face [5]. Most of the lesion present as painless swelling of varying duration. Large lesion causes significant facial disfigurement [5,8]. Parotid and preauricular area is the most commonly involved site. In the present case, the lesion was localized over the cheek producing a soft lobulated mass, giving ‘bag of worm’ feeling typical to neurofibroma. The functional and cosmetic impairment produced by the lesion in child patient puts them at high risk for psychological disturbances, warranting a surgical intervention for its management.
Review of solitary neurofibroma of face.
| Author | Year | Country | Age / Sex | Presentation | Duration | Location | Underlying bone Involvement | Treatment | Recurrence |
|---|
| Kobus K and Wójcicki P, [5] | 2009 | Poland | 15/M | Painless swelling with facial disfigurement | 4 years | Entire left face (extending over temporal-parietal region superiorly to lower border of mandible inferiorly) | Thickening and displacement of frontal, zygomatic and temporal bone | Surgical excision | Recurrence at six months follow up |
| He Y et al., [6] | 2011 | China | 8/M | Painless swelling | 1 month | Right cheek and infra-temporal fossa (extending from skull base to angle of mandible) | None | Surgical excision | No recurrence at one year follow up |
| Maheshwari V et al., [7] | 2011 | India | 40/M | Painless swelling | NA | Right parotid | None | Surgical excision | NA |
| Huang W and Chong WS, [8] | 2013 | Singapore | Middle aged/F | Painless swelling with facial disfigurement | 10 years | Right supraorbital and periauricular region | Periosteal reaction of underlying zygomatic bone | Conservative | NA |
| Rai A et al., [9] | 2015 | India | 36/M | Painless swelling | 1 year | Right parotid | None | Surgical excision | No recurrence at three months follow up |
F = Female, M = Male, NA = Data not available/described
Imaging is essential to study the nature and extent of the lesion before surgical excision. Ultrasonography, MRI angiography were used to evaluate the lesion in the present case. The lesion presented as defined, un-encapsulated, hypoechoic mass with multiple areas of necrotic foci and dilated channels with minimal vascularity on color doppler. It appeared homogenously hyperintense on T2WI image and isointense on T1WI image, with slow flow vascular channels. Solitary neurofibroma of face is localized to soft tissue and produces no bony changes, as also seen in the present case. However, reactive periosteal changes, bone thickening and displacement of underlying bone have been previously reported [5,8]. Angiogram of the presented lesion was seen encasing the facial vessels and its branches. Large, dilated and torturous venous channels were noted within the lesion. Lack of a defined capsule and multiple vascular channels, make the surgical dissection of the lesion tedious with increased risk of blood loss, especially in child patients. Location of the lesion in subcutaneous plane of mid-face also increases the risk of facial nerve injury and damage to underlying muscle bed (masseter and buccinators muscles). Simple surgical excision is treatment of choice for the pathology. The rate of recurrence is low when the tumour is completely excised. Malignant transformation of solitary neurofibroma is considerably low in contrast to neurofibroma associated with neurofibromatosis, which varies from 2–29% [10]. The present case showed satisfactory outcome at one year follow up with no signs of recurrence.
Conclusion
Neurofibroma although a rare neoplasm, can manifest as solitary mass in head and neck region. When localized over the face, it can cause significant disfigurement leading to psychological and emotional disturbance in young patient. Detailed imaging of the lesion helps to know the exact location and extent of the mass, which is often unencapsulated and infiltrates the surrounding tissues. Angiography helps to identify the vessels within the mass, which is often vascular with slow flow characteristics. Surgical excision is treatment of choice. The prognosis is good when the lesion is completely removed, with low recurrence rate.
F = Female, M = Male, NA = Data not available/described
[1]. Wright BA, Jackson D, Neural tumours of the oral cavity. A review of the spectrum of benign and malignant oral tumours of the oral cavity and jawsOral Surg Oral Med Oral Pathol 1980 49:509-22. [Google Scholar]
[2]. Cherrick HM, Eversole LR, Benign neural sheath neoplasm of the oral cavity. Report of thirty-seven casesOral Surg Oral Med Oral Pathol 1971 32:900-09. [Google Scholar]
[3]. Bruce KW, Solitary neurofibroma (neurilemmoma, Schwannoma) of the oral cavityOral Surg Oral Med Oral Pathol 1954 7:1150-59. [Google Scholar]
[4]. Marocchio LS, Oliveira DT, Pereira MC, Soares CT, Fleury RN, Sporadic and multiple neurofibromas in the head and neck region: A retrospective study of 33 yearsClin Oral Investig 2007 11(2):165-69. [Google Scholar]
[5]. Kobus K, Wójcicki P, Gigant facial neurofibromaPolish Journal of Surgery 2009 81(1):53-57. [Google Scholar]
[6]. He Y, Wang J, Zhang Z, Yang H, Fu H, Solitary neurofibroma arising from the infratemporal fossa in a childJournal of Paediatric Surgery 2011 46(7):E13-16. [Google Scholar]
[7]. Maheshwari V, Varshney M, Alam K, Khan R, Jain A, Gaur K, Khan AH, Neurofibroma of parotidBMJ Case Rep 2011 10:1136 [Google Scholar]
[8]. Huang W, Chong WS, Facial plexiform neurofibroma: Is it truly just skin deep?BMJ Case Rep 2013 2013 pii: bcr2013200716 [Google Scholar]
[9]. Arpita Rai A, Kumar A, Neurofibroma of facial nerve presenting as parotid massJ Maxillofac Oral Surg 2015 14(Suppl 1):465-68. [Google Scholar]
[10]. Neville BW, Damm DD, Allen CM, Bouquot JE, Oral and maxillofacial pathology 2002 2nd edPhiladelphiaElsevier:457-61. [Google Scholar]