Surgical Management of a Separated Endodontic Instrument using Second Generation Platelet Concentrate and Hydroxyapatite
SL Satheesh1, Shefali Jain2, Atul Chandra Bhuyan3, Lekshmy S Devi4
1 Senior Lecturer, Department of Endodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
2 Private Practitioner, Department of Endodontics, Dental Panache, Gurgaon, Haryana, India.
3 Professor and Head, Department of Conservative Dentistry and Endodontics, Regional Dental College, Guwahati, Assam, India.
4 Professor, Department of Endodontics, Sri Sankara Dental College, Thiruvananthapuram, Kerela, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shefali Jain, B 1101 The Citizen Sector 51, Gurgaon, Haryana, India.
E-mail: drshefalijain21@gmail.com
Fractured endodontic instrument is an unfortunate endodontic mishap which may obstruct thorough cleaning and shaping of the root canals with potential impact on the endodontic prognosis and treatment outcome. When the fractured segment lies apical to canal curvature, overzealous removal of tooth structure is required to gain access to the separated segment which in turn increases the likelihood of root fracture. In infected cases, the stage at which instrument separation occurs is crucial as root canal disinfection is jeopardized. This case report describes the surgical retrieval of a fractured endodontic file from the mesiobuccal canal of mandibular first molar by limited resection of mesial root. Second generation platelet concentrate called Platelet Rich Fibrin (PRF) and nanocrystalline hydroxyapatite and β-tricalcium phosphate bone graft was placed to fill the surgical defect as the combination enhances the regenerative effect of PRF by exerting an osteoconductive effect in the bony defect area. The clinical and radiographic examination after eighteen months revealed complete periapical healing.
Bone graft, Instrument fracture, Instrument retrieval, Periapical surgery, Platelet rich fibrin
Case Report
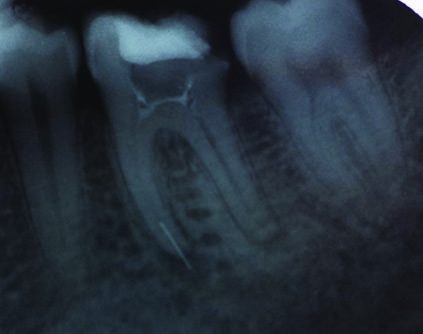
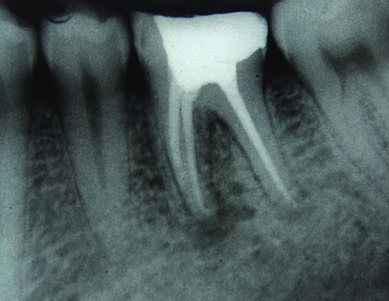
A 32-year-old male patient with a chief complaint of dull aching pain in relation to his mandibular left first molar tooth (# 19) was referred to Department of Endodontics for retreatment. Brief history revealed that the patient had undergone incomplete root canal treatment two weeks before but symptoms persisted. On clinical examination, the first molar had a faulty restoration and was symptomatic with tenderness on percussion. Intraoral radiograph showed a fractured file segment extruding beyond the periapex in the mesial canal with radiolucency evident at the mesial and distal root apices [Table/Fig-1]. The diagnosis was endodontic treatment failure with symptomatic apical periodontitis and retreatment of the molar tooth was planned.
Left mandibular first molar with persistent periradicular infection of the mesial root;
Working length radiograph after bypassing the fractured segment.
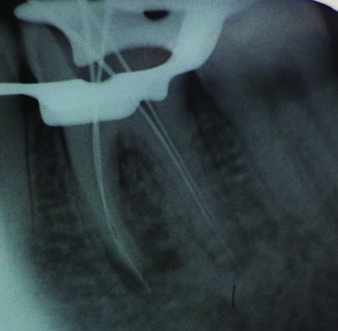
Orthograde retreatment of the first molar was commenced with an attempt to bypass the file in the mesiobuccal canal. After coronal flaring, Protaper rotary NiTi instruments (DENTSPLY Tulsa Dental Specialties) along with RC Prep (Premier Dental Products, USA) were used to prepare the coronal and middle portion of the mesiobuccal canal. Fractured file in the apical third of the mesiobuccal canal was bypassed using precurved stainless steel K file ISO number 10 (Dentsply-Maillefer, Ballaigues, Switzerland). Working length was determined using electronic apex locator (Root ZX, J Morita, USA) and confirmed using radiograph [Table/Fig-2].
The canals were then negotiated to the radiographic terminus with small precurved stainless steel hand files to an apical size of 25 followed by Protaper rotary files sequentially from S1 to F2 to working length. A 5.25% sodium hypochlorite (Novo dental products pvt., ltd, India) was used to irrigate the canals during canal preparation. Similarly cleaning and shaping was completed for mesiolingual and distal canals which were enlarged till F2 and F3 respectively. After canal preparation, a calcium hydroxide based intracanal medicament (RC Cal, Prime dental products pvt ltd, India) was placed and temporized with Cavit (3M ESPE Dental, India) for one week. However, on follow up after one week, the tooth was still symptomatic. Treatment plan was changed to periapical surgery to retrieve the fractured file from mesiobuccal canal because it was deemed likely that further attempts to remove the file could perforate or significantly weaken the mesial root. Patient was recalled after one week.
After a week, when the acute symptoms had resolved, canals were irrigated with 5.25% sodium hypochlorite (Novo dental products pvt. ltd, India) with final rinse of 17% EDTA (Canalarge, Ammdent, Chandigarh, India). After copious saline irrigation, the canals were dried with paper points. Master cone radiograph [Table/Fig-3] was taken and the root canals were obturated with corresponding protaper guttapercha cones and AH plus sealer (Dentsply, maillefer, USA) [Table/Fig-4]. Access preparation was restored with amalgam restoration.
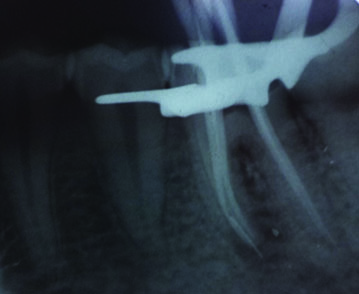
Post obturation radiograph.
Following obturation, periapical surgery was initiated. Complete intraoral disinfection was done with betadine rinse before surgery. After administration of local anaesthesia (1:80000 adrenaline, Lignox, Warren pharmaceuticals pvt., ltd, India), intrasulcular incision was given extending from distal aspect of premolar to mesial aspect of second molar with subsequent divergent release incisions. A full thickness mucoperiosteal flap was reflected on the buccal aspect.
Buccal window of approximately 6 mm diameter was created by osteotomy to locate the mesial root end [Table/Fig-5].
Bony window created in the buccal cortex;

Surgically retrieved fractured endodontic instrument.

Since mesiobuccal and mesiolingual canal had separate portals of exit, decision was made to do a limited root resection of the mesial root. Apex of mesial root along with the extruded instrument could be well visualised. The portion of mesial root involving the mesiobuccal canal extending approximately 8mm from the periapex coronally was planned to remove. A cut was made perpendicular to the long axis of the root from the buccal aspect through the gutta-percha in the mesiobuccal canal till sound dentin was reached. A deep cut was made using a round bur with copious irrigation using sterile saline, parallel to the long axis, nearly located in the centre of mesial root through the mesial and distal aspect. The cut segment along with the fractured file was retrieved [Table/Fig-6] and all pathological tissue was thoroughly debrided with curettage.
A 2-3 mm deep root end cavity was prepared using ultrasonic tips and subsequently filled with Mineral Trioxide Aggregate (MTA Angelus® Gray, Angelus, Lodrina, Parana, Brazil). The osseous defect was filled with PRF produced by using Choukron’s Technique [1] and a synthetic nanocrystalline hydroxyapatite and β tricalcium phosphate bone graft (SYBOGRAF™-Plus). PRF protects the surgical site, promotes soft tissue healing and when used in combination with hydroxyapatite, an osteoconductive material, it will enhance bone regeneration [2]. Mucoperiosteal flap was approximated with multiple interrupted sutures [Table/Fig-7].
Final suturing after placement of PRF and bonegraft crystals (SYB-OGRAF™ –Plus);

Immediate postoperative radiograph after retrieval of fractured instrument from mesiobuccal canal;
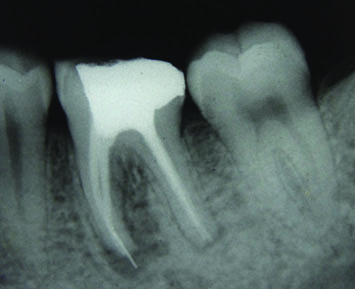
Radiograph at 18 months demonstrates complete healing of the periapical lesion with formation of normal periodontal ligament space around the apex.
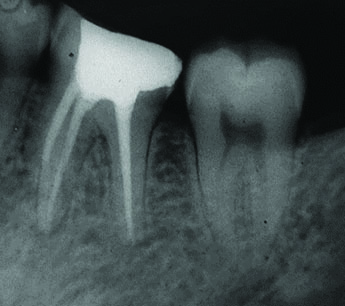
An immediate postoperative radiograph was taken to confirm complete retrieval of the fractured segment [Table/Fig-8].
Antibiotics (Amoxycillin and clavulanate potassium 625 mg) and Non-Steroidal Analgesics (Diclofenac) were prescribed along with 0.2% chlorhexidine digluconate mouthwash for five days post surgery. On recall after surgery days, patient was asymptomatic and sutures were removed.
Postoperatively clinical and radiographic examinations were done in six months interval for a period of eighteen months. The radiograph demonstrated complete healing of the periapical radiolucency with no clinical signs or symptoms [Table/Fig-9].
Discussion
Instrument fracture prevents optimal cleaning and shaping of the root canals thereby compromising the final outcome because of pulp remnants and bacteria persisting in the canals [3]. In this case report, RVG was used for precise location of the fractured segment similar to the case report of Gandevivala A et al., for retrieval using a surgical approach [4]. Other newer modalities of retrieval of a fractured instrument reported include atraumatic extraction and removal of the fractured instrument extraorally followed by replantation [5].
Cone beam computed tomography helps in accurate visualization of anatomic structures and precise planning of the surgical procedure. With the advancements in 3D imaging technologies and digital impressions, virtual surgical templates can be created and printed using 3D printers. Guided modern endodontic periapical surgery and guided endodontics for management of pulpal calcifications have been reported [6,7].
A combination of PRF and bone graft was placed to fill the bone defect to accelerate the healing process by acting as a scaffold as done by Jayalakshmi KB et al., [8]. PRF, a second generation platelet rich concentrate, has diversified applications in dentistry such as extraction socket preservation, reconstruction of osseous defect, sinus lift procedures, alveolar ridge augmentation etc. The fibrin network present in PRF enhances cellular migration and angiogenesis. The multiple growth factors (PGDF, TGF and IGF) in PRF are released slowly resulting in a continual healing process as the leukocytes and cytokines present regulates any infectious/ inflammatory process in bone graft materials [9,10].
Conclusion
In this case report, surgical removal of the foreign body and use of stem cell rich PRF with bone graft ensured successful resolution of symptoms and periapical healing by enhancing body’s natural wound healing mechanism.
[1]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet-rich fibrin (PRF): a secondgeneration platelet concentratePart I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:e37-44. [Google Scholar]
[2]. Pradeep AR, Rao NS, Agarwal E, Bajaj P, Kumari M, Naik SB, Comparative evaluation of autologous platelet rich fibrin and platelet-rich plasma in the treatment of 3-wall intrabony defects in chronic periodontitis: a randomized controlled clinical trialJ Periodontol 2012 83:1499-507. [Google Scholar]
[3]. Suter B, Lussi A, Sequeira P, Probability of removing fractured instruments from root canalsInt Endod J 2005 38(2):112-23. [Google Scholar]
[4]. Gandevivala A, Parekh B, Poplai G, Sayed A, Surgical removal of fractured endodontic instrument in the periapex of mandibular first molarJ Int Oral Health 2014 6(4):85-88. [Google Scholar]
[5]. Shenoy A, Mandava P, Bolla N, Vemuri S, A novel technique for removal of broken instrument from root canal in mandibular second molarIndian J Dent Res 2014 25:107-10. [Google Scholar]
[6]. Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C, Guided modern endodontic surgery: a novel approach for guided osteotomy and root resectionJ Endod 2017 43(3):496-501. [Google Scholar]
[7]. Krastl G, Zehnder MS, Connert T, Weiger R, Kuhl S, Guided Endodontics: A novel treatment approach for teeth with pulp canal calcifiication and apical pathologyDental Traumatology 2016 32:240-46. [Google Scholar]
[8]. Jayalakshmi KB, Agarwal S, Singh MP, Vishwanath BT, Krishna A, Agrawal R, Platelet-rich fibrin with beta-tricalcium phosphate-a noval approach for bone augmentation in chronic periapical lesion: a case reportCase Rep Dent 2012 2012:902858 [Google Scholar]
[9]. Kökdere NN, Baykul T, Findik Y, The use of platelet-rich fibrin (PRF) and PRF- mixed particulated autogenous bone graft in the treatment of bone defects: An experimental and histomorphometrical studyDent Res J (Isfahan) 2015 12(5):418-24. [Google Scholar]
[10]. Naik B, Karunakar P, Jayadev M, Marshal VR, Role of platelet rich fibrin in wound healing: a critical reviewJ Conserv Dent 2013 16:284-93. [Google Scholar]