Tumours of the nervous system constitute 1%-2% tumours in adults (About 2,57,000 cases per year world-wide); the incidence does not vary markedly between regions or population [1]. The predominant Central Nervous System (CNS) tumour types in adults are metastasis, glial neoplasms and meningioma [2]. The worldwide incidence of brain tumours has been reported to be around 3.9 /one lac/year in males and 3.0 /one lac/year in females [1]. The South Central Asia region including India has an incidence of 1.5 and 0.7/one lac/year in males and females respectively [1,3]. Previous studies have shown an overall increase in brain tumours [1,2,4]. There has been a documented increase in the number of CNS tumours in both males and females in India [4]. The recent trends from developed countries show a decline in low grade tumours and an increase in higher grade tumours. Some studies have suggested an increased incidence of CNS neoplasms associated with certain occupations, dietary factors and exposure to chemicals, but most of these reports have not been confirmed and causative agents have not been identified [1,3].
The majority of tumours of CNS are meningiomas and gliomas; the most common WHO grade IV tumour being glioblastoma Not Otherwise Specified (NOS). Due to improved diagnostic and treatment modalities available; particularly in the developing countries, an increased incidence of glial tumours (by 1%-2% per year) has been observed [2]. Several factors impede the systematic study of epidemiology of CNS tumours. These include the distinct clinico-pathological entities grouped under this general heading and their different aetiological factors, difficulty in obtaining diagnostic material for intracerebral and intraspinal lesions and the fact that even low grade lesions may have dramatic consequences for the patients. The scarcity of reliable data collection and financial constraints are challenges faced by developing countries. The large population load also adds to the tumour burden. Specifically till date, there is no published database on the profile of brain tumours in South Indian population. The present study is an attempt to identify the age groups, gender distribution, topography and different histological types of brain tumours in the population attending our hospital.
Materials and Methods
We did a retrospective analysis of the data on brain tumours obtained from the hospital cancer registry and histopathology reports in the department of pathology during the seven year study period (2009-2015). Purposive sampling of cases was done and the study subjects included all cases of brain tumours received in the department. Non neoplastic and inflammatory lesions of the brain were excluded. We retrieved the slides of these cases and reviewed them. Immunohistochemistry in required cases were done. Strict confidentiality of patient information was maintained while handling the data sets. Those cases with incomplete data were excluded from the study. This study was approved by the Institutional Review Board (IEC No.56/16).
All the CNS tumours were divided into the following categories: glial tumours, meningeal tumours, germ cell and embryonal tumours, tumours of sellar region, neuroepithielial and choroid plexus tumours, haemangioblastoma, tumours of the cranial and paraspinal nerves, lymphomas and haematopoietic neoplasms and metastatic tumours. In addition to histology, molecular parameters were also included in the 2016 WHO classification of CNS tumours. Since the molecular testing and cytogenetic studies were not available in our institution the diagnosis was reclassified as tumours NOS.
Statistical Analysis
Age and gender distribution, clinical presentation, site of tumour and histopathologic patterns with grade were noted and the data was analysed with SPSS software.
Results
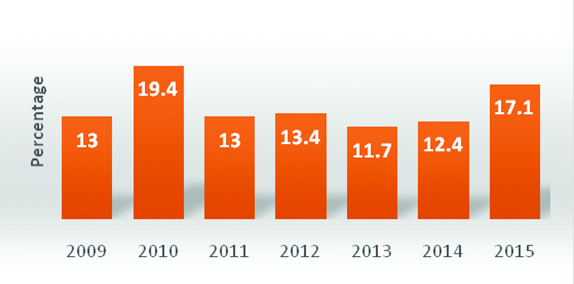
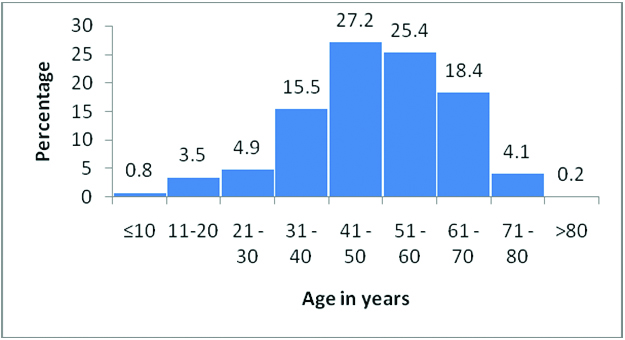
A total of 510 cases of CNS tumours were analysed over a period of seven years. These included 405 cases of primary brain tumours, 70 cases of spinal tumours and 35 cases of metastasis to brain. The year wise distribution of cases showed an increase in number of cases in 2010 and 2015 [Table/Fig-1]. In our study the predominant age group affected was between 40-60 years (58.1%) [Table/Fig-2]. There were only 18 cases of paediatric brain tumours (age<18 years) in our study. The median age group of different histological subtypes of brain tumours in this study was compared with those from international (CBTRUS) data and national (NIMHANS) data [Table/Fig-3] [5,6].
Year-wise distribution of CNS tumour cases.
Age-wise distribution of CNS tumour cases.
Histology and median age (in years) CBTRUS data (2006-2010) and NIMHANS data (2010-2014) compared with the present study.
| DIAGNOSIS | Median age NIMHANS data (2010-2014) | Median age CBTRUS data (2006-2010) | Median age of present study (2009-2015) |
|---|
| Meningioma | 45 | 65 | 52 |
| Glioblastoma NOS | 50 | 64 | 55.5 |
| Diffuse astrocytoma NOS | 37 | 48 | 40 |
| Anaplastic astrocytoma NOS | 36 | 53 | 48 |
| Oligodendroglioma NOS | 40 | 43 | 52 |
| Mixed gliomas | 36 | 42 | 49 |
| Ependymal tumours | 18 | 45 | 49 |
| Peripheral nerve tumours | 40 | 55 | 48 |
| Pituitary adenoma | 42 | 51 | 47 |
| Craniopharyngioma | 22 | 42 | 47.5 |
| Lymphoma | 50 | 65 | 60 |
Brain tumours were more common in females compared to males and showed M:F ratio of 0.9:1. Distribution of CNS tumours in males and females is shown in [Table/Fig-4]. Among females the most common diagnosis was meningioma (44.4%) and in males it was astrocytic tumours (30.6%) [Table/Fig-4]. Spinal tumours showed a slight male predominance (14.9% of tumours in males and 12.7% in females).
Distribution of brain tumours in relation to gender.
| Diagnosis | Sex | Total |
|---|
| Male | Female |
|---|
| n | % | N | % | N | % |
|---|
| Meningioma | 58 | 24.0 | 119 | 44.4 | 177 | 34.7 |
| Astrocytic tumours | 74 | 30.6 | 54 | 20.1 | 128 | 25.1 |
| Oligodendroglial tumours | 1 | 0.4 | 1 | 0.4 | 2 | 0.4 |
| Mixed gliomas | 6 | 2.5 | 6 | 2.2 | 12 | 2.4 |
| Ependymal tumours | 4 | 1.7 | 3 | 1.1 | 7 | 1.4 |
| Choroid plexus carcinoma | 1 | 0.4 | 0 | 0.0 | 1 | 0.2 |
| Peripheral nerve tumours | 36 | 14.9 | 35 | 13.1 | 71 | 13.9 |
| Lymphoma | 1 | 0.4 | 4 | 1.5 | 5 | 1.0 |
| Metastasis | 26 | 10.7 | 9 | 3.4 | 35 | 6.9 |
| Neuroglial tumours | 2 | 0.8 | 4 | 1.5 | 6 | 1.2 |
| Sellar tumours | 13 | 5.4 | 17 | 6.3 | 30 | 5.9 |
| Mesenchymal tumours | 6 | 2.5 | 8 | 3.0 | 14 | 2.7 |
| Germinoma | 0 | 0.0 | 1 | 0.4 | 1 | 0.2 |
| Embryonal tumours | 1 | 0.4 | 1 | 0.4 | 2 | 0.4 |
| Epidermal cyst | 2 | 0.8 | 3 | 1.1 | 5 | 1.0 |
| Haemangioblastoma | 10 | 4.1 | 3 | 1.1 | 13 | 2.5 |
| Chordoma | 1 | 0.4 | 0 | 0.0 | 1 | 0.2 |
| Total | 242 | 100.0 | 268 | 100.0 | 510 | 100.0 |
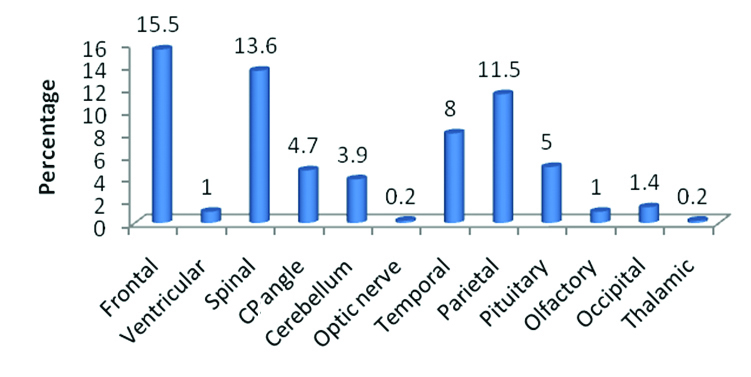
Among the brain tumours the most common site involved was the frontal lobe of cerebrum followed by parietal and temporal lobes [Table/Fig-5]. Many of the tumours involved more than one lobe of brain. The least affected was occipital lobe.
Site-wise distribution of CNS tumour cases.
The most common histological diagnosis in the current study was meningioma. A total of 177 cases (34.6%) were diagnosed followed by astrocytic tumours (25.2%) and peripheral nerve sheath tumours (13.8%) [Table/Fig-6].
Distribution of different histopathological entities.
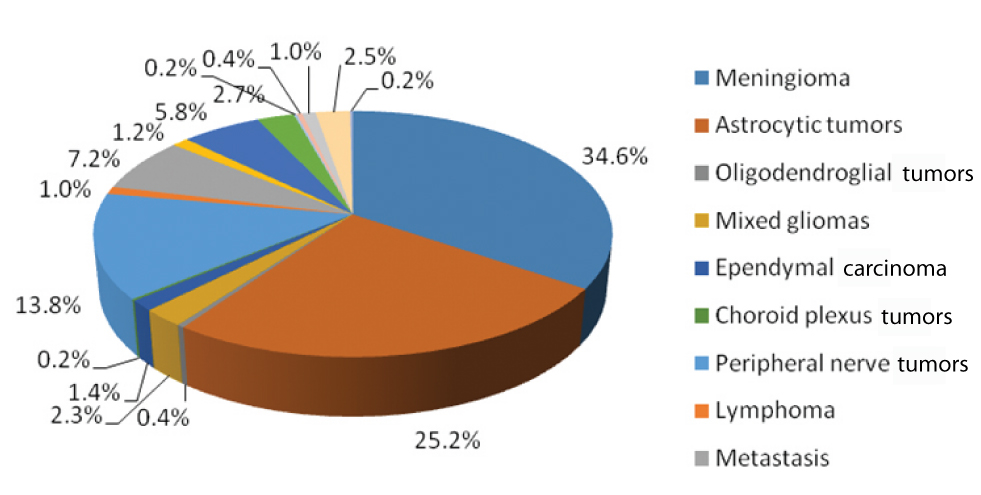
Meningiomas showed female predominance and the median age affected was 52 years. Incidence of meningioma, more or less remained the same after 40 years. The most common sites were dura overlying frontal and parietal lobes of cerebrum. The most common histological subtype was transitional meningioma followed by meningothelial type. There were 156 cases (87.5%) of grade I meningioma, 17 cases (9.6%) of grade II and five cases (2.9%) of grade III meningiomas noted. Among the spinal meningiomas the most common histological subtype was psammomatous meningioma.
Astrocytic tumours were the second most common histological type in our analysis (128 cases). There was a male predominance (74/128 cases) and WHO grade IV tumour-glioblastoma NOS showed a median age of 55.5 years. Most common site involved was the temporo parietal lobe of cerebrum. None of the cases involved the occipital lobe. Among the glial tumours, glioblastoma NOS- grade IV was the most common histological subtype (58.5%) followed by diffuse astrocytoma NOS, grade II (26.9%).
The third common histological diagnosis was peripheral nerve sheath tumours of which 85.9% (61/71 cases) were schwannomas. The most common site was cerebello pontine angle. Median age group affected was 48 years.
Among the 30 sellar tumours studied 23/30 (76.7%) cases of pituitary adenoma, six cases of craniopharyngioma and a single case of pituicytoma were observed. The most common tumour involving the cerebellum was haemangioblastoma (50%) followed by metastasis (20%) and astrocytoma (15%).
Discussion
The seven year data of our hospital based study was analysed and no marked variation in the distribution of CNS tumours over these years were observed. The predominant age group affected was between 40-60 years which was comparable with most other worldwide studies [6,7]. The median age group of different histological subtypes of brain tumours in this study was intermediate between those from international (CBTRUS) data and national (NIMHANS) data [5,6] [Table/Fig-3]. The median age group of meningioma was 52 years in our study compared to 45 years in NIMHANS and 65 years of CBTRUS. High grade (WHO grade III and IV) tumours like glioblastoma NOS also showed a similar pattern, median age of 55.5 years in our study and 50 years in NIMHANS and 64 years in CBTRUS respectively. The late occurrence as compared to national data could be due to the better health care facilities and higher literacy rate in our part of the country. M:F ratio of 0.9:1 was observed in our study which was consistent with those studies which included meningeal tumours also [7,8]. Glial tumours (the most common category being astrocytic tumours) and metastasis were observed more frequently in male patients, while tumours of the meninges exhibited a female predominance in our data. Frontal lobe was the most common site of brain tumours in our study. Trabelsi S et al., Zahir ST et al., and Krishnatreya M et al., also observed frontal lobe as the commonest site of brain tumours [7-9].
Meningioma was the most common diagnosis in our study and it occurred mostly in females. This is in concordance with most of the worldwide studies where meningioma was also included among the CNS tumours [6,10-12]. All the different histological types of meningioma were identified. The most common histological subtype was transitional meningioma followed by meningothelial meningioma. The second common histological diagnosis was astrocytic tumours, which showed a male predominance and this is in par with observations by Jaiswal J et al., Ghanghoria S et al., and Jazayeri SB et al., [6,10,11]. The most common astrocytic tumour type was glioblastoma NOS, which occurred at the median age of 55.5 years. Rare histological variants of glioblastoma like small cell glioblastoma, giant cell glioblastoma and glioblastoma with pleomorphic xanthoastrocytoma like areas were noted. Comparison of data on brain tumours in adults with other recent studies has been presented in [Table/Fig-7] [6,9-12].
Comparison of data on brain tumours in adults with other recent studies [6,9-12].
| Variables | Present study | Jaiswal J et al., [6] | Krishnatreya M et al., [9]* | Ghanghoria S et al., [10] | Jazayeri SB et al., [11] | Chen L et al., [12] |
|---|
| Type of study | Hospital based study | Hospital based study | Hospital based study | Hospital based study | National cancer registry based study | Hospital based study |
| Number of cases | 510 | 4295 | 231 | 65 | 10,802 | 34,640 |
| M:F ratio | 0.9:1 | 1.3:1 | 2.3:1 | 1: 0.86 | 1.48:1 | 0.9:1 |
| Most common age group | 40-60 years | 30-40 years | 20-60 years | 30-50 years | 30-60 years | 30-60 years |
| Most common site | Frontal-80 (15.5%) | NA | Frontal- 103 (44.6%) | NA | NA | NA |
| Histological diagnosis | Meningioma (34.7%), Astrocytic tumours,(25.1%) | Meningiomas (23.2%), Glioblastomas (15.5%),Nerve sheath tumours (12.7%) | Diffuse astrocytoma (37.2%), Glioblastoma (21.2%) | Meningioma (41.54%), Astrocytoma (24.61%) | Meningioma (27.8%), Astrocytoma (15.2%), Glioblastoma (13.8%) | Meningioma (33.6%), Schwannoma (14.2%), Astrocytic tumours (11.4%) |
Krishnatreya M et al.,(2014) excluded tumours arising from the meninges
In adults we came across most of the tumour types mentioned in the WHO classification and the distribution was also similar to those observed worldwide. The latest WHO classification of CNS tumours (2016) uses histology and molecular parameters to define tumour entities with an aim to enhance objectivity. They have redefined the existing tumours based on molecular pathology and added newer genetically defined entities [13]. Immunohistochemical surrogates (IDH immunohistochemistry and other markers) for molecular changes are under evaluation which may be easier and more accessible in our setting [13].
Conclusion
Population based studies are more effective as they shed light on the actual tumour incidence in the population under study as compared to hospital based data. For developing countries, due to the financial constraints a comprehensive database is a dream yet to achieve. In this context these types of studies give a glimpse of the varied distribution of brain tumours in our population. Over all the histological pattern of primary CNS tumours in our cohort paralleled with national as well as the international data. Better socioeconomic and educational level in our part of the country possibly explains the variation in age and grade of tumours diagnosed.
Limitation
The limitations of study included hospital bias, as the sample population includes only those who underwent surgery in our institution. The study conducted was a single-centre retrospective analysis and hence the data is not representative of the national epidemiology of CNS tumours. Another factor that needs to be considered is, our hospital being a government institution caters mainly the lower socioeconomic class in the society, limiting the number of cases included.
*Krishnatreya M et al.,(2014) excluded tumours arising from the meninges