Intestinal anastomosis is a common procedure both in elective and emergency surgeries and hence, it is imperative for both practicing surgeons and residents to be familiar with and to master the art of safe bowel anastomosis. The technique of anastomosis depends upon the site of anastomosis, condition of the bowel and the underlying disease aetiology, and also the general condition of the patient [1]. Individual surgical skill and preference is another important decisive factor. Many techniques have evolved but, the hand sewn suturing technique remains the mainstay for intestinal anastomosis because of availability and affordability of suture material and familiarity with the procedure.
Historically, two-layer anastomosis has been the conventional method for most surgical situations. But, it is tedious, time-consuming and there is potential risk of anastomotic stricture formation. Recently, single layer continuous anastomosis using monofilament suture has been adopted by many surgeons due to reports describing its cost-effectiveness, less time consumption and no increase in rates of leakage as compared to double-layer method [2].
However, despite large amount of work done on both single and double layered methods, it is still unclear which method is better in terms of safety and efficacy. A recent Cochrane database review compared effectiveness of single layer versus double layer gastrointestinal anastomosis [3]. It suggested further trials aimed to reduce the limitations of the review since the conclusion was derived from smaller number of patients recruited in relatively moderate quality trials. Therefore, the present study was designed to compare the efficacy, safety and cost effectiveness of single layer continuous extra-mucosal intestinal anastomosis versus double layer method.
Materials and Methods
A single-centre prospective, double-blind, randomized controlled comparative study was conducted in the Department of General Surgery, SCB Medical College and Hospital, Cuttack, Odisha, India during September, 2013 to September, 2015.
Patients requiring intestinal resection and anastomosis, were assessed for eligibility following admission to the ward. Patients enrolled were subjected to physical examination, routine blood investigations and imaging (ultrasonography or computed tomography of abdomen) as appropriate. Adult patients aged 18-65 years of either sex were considered eligible. Only haemodynamically stable patients with no peritoneal contamination and with a haemoglobin level of > 8 gm/dL were included. Both emergency and elective procedures with jejuno-jejunal, jejuno-ileal and ilieo-ileal anastomosis; ileo-colic and colo-colic anastomoses; and stoma closure were taken up for the study. Patients undergoing gastric, duodenal and rectal anastomosis, or proximal diversion were not included. Cases in which delayed recovery was expected i.e., septicaemic or hypovolaemic shock; profuse intraoperative or postoperative bleeding (>1 litre); severely cachectic patients requiring simultaneous total parenteral nutrition; re-exploration cases; patients requiring intensive care in postoperative period; severe systemic organ dysfunction (chronic liver, renal or heart diseases, diabetes mellitus); massive small intestinal resection; immunocompromised patients were excluded from the study.
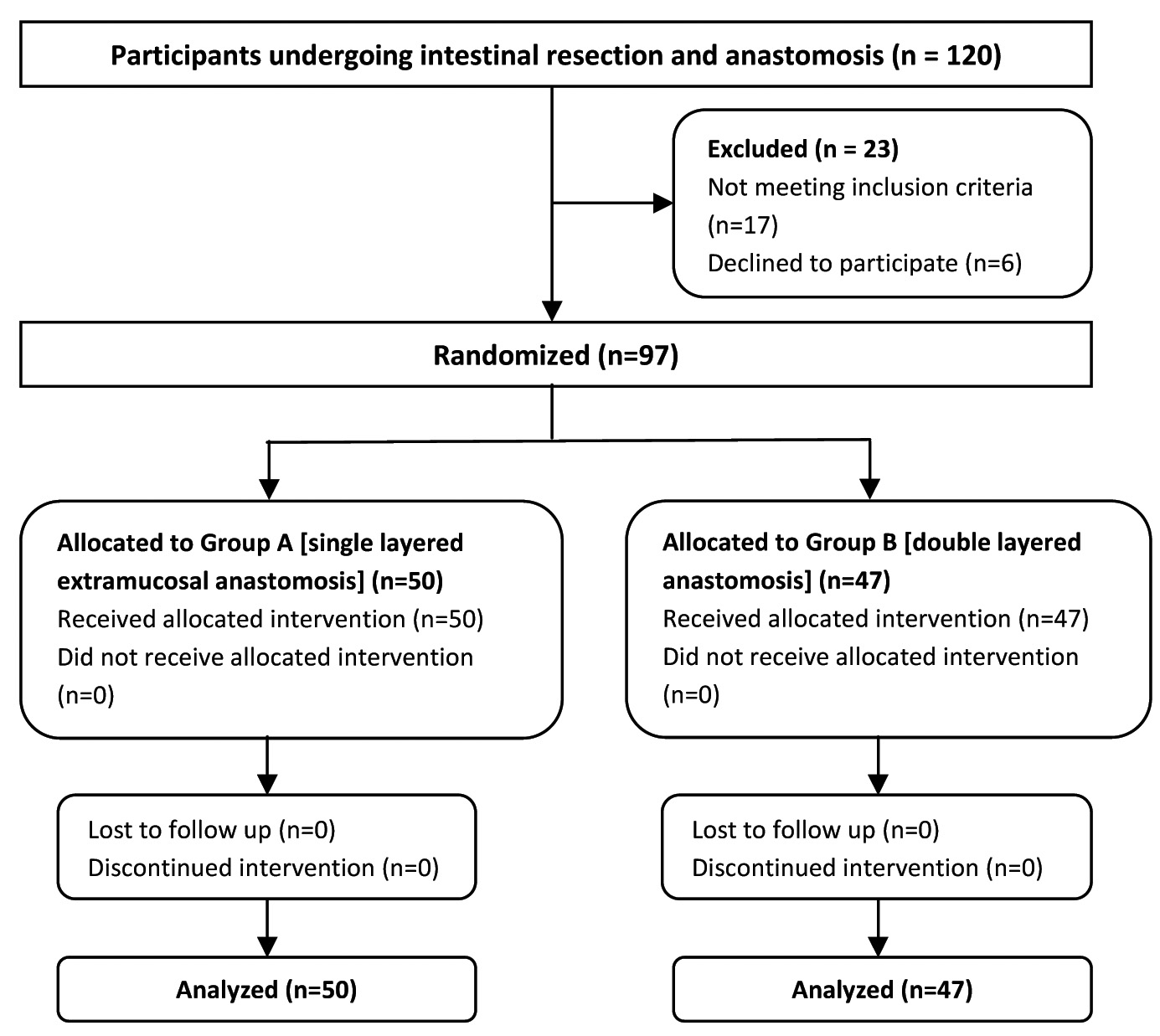
A total of 97 eligible patients who underwent intestinal resection and anastomosis were randomized [Table/Fig-1].
Flow diagram showing participant recruitment, allocation, follow up and analysis.
Prior written informed consent was obtained from all the study subjects after explaining them the study protocol. Randomization for each patient was predetermined by a random number generator and was performed using random permuted blocks of size 10. Participants were randomly assigned to undergo either single layered extramucosal intestinal anastomosis (Group-A) or double layered intestinal anastomosis (Group-B) by opening a sealed opaque envelope indicating the technique to be used. These envelopes were placed in the operating room and were drawn sequentially just before surgery. At this point, each patient was considered randomized. The study participants and the care providers who followed up the patients in the postoperative ward were unaware of the type of anastomosis.
Primary outcome measures included average time taken for anastomosis in minutes, incidence of postoperative complications (such as anastomotic leak, intra-abdominal abscess, pelvic collection, persistent vomiting, abdominal distension), mean duration of hospital stay, and cost of suture material used. Secondary outcome measures assessed the postoperative return of bowel function and included duration of nasogastric tube kept in situ (in days), duration for return of bowel sounds postoperatively (mean in days) and day of first postoperative bowel movement (mean in days).
All patients were operated and managed postoperatively by the same surgical unit. The affected segment of bowel was resected as per the standard technique. All anastomoses were of end-to-end type. The single layered anastomoses were performed by using continuous 3-0 polydioxanone suture beginning at the mesenteric border and taking all layers of bowel wall except the mucosa into the bite. The double layered anastomoses were performed using interrupted 3-0 silk Lembert sutures for outer layer and continuous 3-0 polyglycolic acid suture for the transmural inner layer. Stitch advancement was approximately 5 mm. Each bite included 4 to 6 mm of the seromuscular wall; the larger bites were taken at the mesenteric border to ensure an adequate seal. Only enough pressure was applied to the suture while approximating the bowel ends so as to make the anastomosis watertight and at the same time avoid ischemia.
Intraoperative findings, hemodynamics and complications if any, quantity and cost of suture material used, were noted. Time taken for the anastomosis was recorded from the beginning with the placement of first stitch and ending with cutting of extra suture material from the last stitch of anastomosis. Nasogastric tube was not used preoperatively in any of the patients undergoing stoma closure with selective insertion of the nasogastric tube being done postoperatively depending on the patient’s clinical course.
All patients received similar antibiotics (i.e., Injection Ceftriaxone and Metronidazole) and standard postoperative care. Patients were followed up till two weeks post surgery. The time taken for postoperative return of bowel function was assessed. Any immediate or delayed complications were recorded. Anastomotic leak was defined as radiographic demonstration of a fistula or non-absorbable material draining from a wound after oral administration, or visible disruption of the suture line during re-exploration. Intra-abdominal abscess without visible discharge was seen in patients as fever, persistent abdominal pain, tachycardia, and raised leucocyte count and was confirmed on ultrasound of the abdomen. The total length of hospital stay (in days) was calculated from the day of operation.
Expecting the difference of means to be detected in cost of procedures in both groups of patients as Rs. 92 (with Standard Deviation=90), the sample size calculated was 26 subjects in each group with α error 0.05 and power of study 90%. The sample size calculated for another variable i.e., the total time taken for the anastomosis was 12 subjects in each group. So, minimum sample size for studying both variables was 26 participants in each group. Study was approved by Institutional Ethical Committee.
Statistical Analysis
Data was analysed based on the intention-to-treat principle. Statistical analysis was performed using the Statistical Package for Social Sciences for Windows (SPSS, version 20.00). Differences between the two groups were assessed using the Chi-square test with or without Yates correction for categorical data and student t-test for continuous variables. A p-value of <0.05 was considered as statistically significant.
Results
A total of 97 participants were randomized. Fifty patients were allocated to single layered extramucosal continuous anastomosis (Group-A) and 47 patients to double layered anastomosis (Group-B). The patients in each group were well matched for age, sex and diagnosis [Table/Fig-2].
Comparison of study groups with respect to age, sex and diagnosis.
| Parameters | Group-Α (n=50) | Gtoup-B (n=47) | p-value |
|---|
| Age (in years; Mean±SD) | 42.96 ± 3.76 | 42.63 ± 3.34 | 0.6495 |
| Sex:MaleFemale | 3317 | 2918 | 0.6590 |
| Diagnosis:TraumaCancerInflammatoryStoma closureOther | 1210071803 | 1111051604 | 0.8619 |
Total 63 resection anastomosis and 34 stoma closure were performed. Out of the 50 anastomoses performed using the single layered method, the most common was ileostomy closure followed by ileo-ileal anastomosis; the double layered anastomosis was most commonly performed for ileo-ileal anastomosis and ileostomy closure [Table/Fig-3].
Distribution of cases according to site of anastomosis and method of anastomosis; figures in parenthesis indicate percentage of cases in respective groups.
| Site of anastomosis | Single layered (n=50) | Double layered (n=47) | Total (n=97) |
|---|
| Jejuno-jejunal | 05 (10%) | 03 (6.38%) | 08 (8.24%) |
| Ileo-ileal | 14 (28%) | 12 (25.53%) | 26 (26.80%) |
| Ileo-ascending | 02 (4%) | 03 (6.38%) | 05 (5.15%) |
| Ileo-transverse | 07 (14%) | 08 (17.02%) | 15 (15.46%) |
| Colo-colic | 04 (8%) | 05 (10.64%) | 09 (9.28%) |
| Ileostomy closure | 15 (30%) | 11 (23.40%) | 26 (26.80%) |
| Colostomy closure | 03 (6%) | 05 (10.64%) | 08 (8.25%) |
| Total | 50 (100%) | 47 (100%) | 97 (100%) |
The mean time taken for anastomosis and the length of hospital stay was significantly shorter in Group-A. The total number of suture packs required in double-layered anastomosis was 3, 1 pack of 3–0 polyglactin and 2 packs of 3–0 silk, whereas in single-layer anastomosis, only one pack of 3–0 polydioxanone was used. The return of bowel function was quicker in the single layer group as compared to the double layer group [Table/Fig-4]. However, there was no significant difference in the complication rates between the two groups (p-value >0.05) [Table/Fig-5]. One anastomotic leak was observed in the double layer group.
Characteristics of patients undergoing single layered extramucosal anastomosis versus double layered anastomosis;
| Observed parameter | Study group characteristics | p-value |
|---|
| Single layered extramucosal (n=50) | double layered (n=47) |
|---|
| Mean time taken for anastomosis (in minutes) | 15.12±2.27 | 24.38 ± 2.26 | <0.001* |
| Duration of nasogastric tube kept in situ (in days) | 1.91±0.75 | 2.32 ± 1.01 | 0.0249* |
| Return of bowel sounds on postoperative day(mean in days) | 2.42±1.11 | 3.1 ± 1.34 | 0.0076* |
| Day of first postoperative bowel movement (mean in days) | 4.18±1.22 | 4.85 ± 1.63 | 0.0236* |
| Complications recorded (total no. of cases) | 04 | 09 | 0.14001† |
| Mean duration of hospital stay (in days) | 5.90±1.43 | 7.29 ± 1.89 | <0.001* |
| Cost of suture material in INR | 564 | 480 | |
continuous variables expressed as Mean ± SD;
Student’s t-test;
Chi-square test
Distribution of complications in relation to method of anastomosis; figures in parenthesis indicate percentage of complications in respective method of anastomosis group.
| Type of complication (postoperative) | Method of anastomosis | p-value |
|---|
| Single layered (n=50) | Double layered (n=47) |
|---|
| Anastomotic leak | (0%) | 01 (2.13%) | 0.4878 |
| Abdominal abscess | 02 (4%) | 02 (4.25%) | 0.7259 |
| Pelvic collection | - (0%) | 01 (2.13%) | 0.4878 |
| Persistent vomiting | 01 (2%) | 03 (6.38%) | 0.7638 |
| Abdominal distension | 01 (2%) | 02 (4.25%) | 0.9126 |
| Total | 04 | 09 | |
The leak was detected on the eighth postoperative day following ileo-ileal anastomosis; it was managed conservatively without fecal diversion. There were two mortalities one in each group and none was related to anastomotic complications.
Discussion
The most important factors in the creation of a bowel anastomosis are meticulous technique, gentle tissue handling, adequate apposition of bowel ends, good blood supply and absence of tension or distal obstruction [1]. As evident from randomized trials, no differences in rates of leakage, duration of hospital stay, and overall morbidity have been noted between stapled and hand-sewn anastomosis [4]. Interrupted sutures have no advantage over continuous sutures; however, evidence for this comes from retrospective studies only [5]. The conventional sutured anastomosis may be performed either in a double layer or a single layer. The double layered intestinal anastomosis was formulated in the early 19th century by Travers B in his experimental work [6].
Interrupted absorbable or non-absorbable sutures are utilized for outer sero-muscular layer and continuous or interrupted absorbable sutures are used for the trans-mural inner layer in case of double layered anastomosis [2]. Hautefeuille P in 1976, first gave a detailed account of the single-layer continuous anastomosis [7]. However, either continuous or interrupted absorbable sutures can be used for single layer anastomosis. The present study compared the classical double layered method of intestinal anastomosis with the single layered extramucosal continuous method of anastomosis in terms of efficacy and safety.
The mean age of patients in other studies was similar approximating about 44 years [8]. On analysis of our data, it was found that the time required for the construction of single layered anastomosis was significantly lower than the double layered anastomosis with the p-value <0.001 which was highly significant. Previous studies reported significantly shorter duration of anastomosis for single layered anastomosis [9,10]. To accomplish a two-layer anastomosis, more meticulous circumferential clearing of mesentery, appendices epiploica, and omentum is required before beginning the anastomosis. While with the single-layer method, less or no circumferential clearing is necessary. Thus, time required to prepare the bowel for anastomosis is also less for one-layer technique [8]. The overall shorter operative time in case of single-layer method might be of significance in patients with haemodynamic instability who are operated in emergency. Moreover, this technique is easily learned, flexible in its application [11].
The ultimate test for safety and efficacy of a technique for intestinal anastomosis is its rate of anastomotic leakage. An anastomotic leak increases the morbidity and mortality associated with the operation: it can double the length of the hospital stay and increase the mortality by threefold [4]. They are diagnosed either clinically or radiographically by contrast enema or computed tomography scan [12]. There was no anastomotic leak in the single layered group while one patient developed leak in the double layered group in our study (p=0.4878). The complication rate including abdominal abscess and pelvic collection was similar to both the groups. A 2006 meta-analysis analysing 670 patients concluded that there was no difference in the rate of postoperative leakage between the two techniques [2]. Burch JM et al., and Ceraldi CM et al., too observed no statistically significant difference in the rates of anastomotic leaks or abdominal abscess between the two techniques [8,13]. In a prospective series of 553 single-layer interrupted serosubmucosal anastomoses, the leakage rate was 0.2% which was similar to our study [14].
In the double layer technique, submucosal vascular plexus may be compromised and there may be excessive inversion and inflammation of tissue leading to narrowing of lumen. Single layer anastomosis causes least damage to submucosal vascular plexus, least chances of luminal narrowing, incorporates strongest submucosal layer and accurate tissue apposition [15]. Although evidence is lacking, continuous sutures are speculated to have better serosal apposition and blood flow than interrupted sutures [16]. Postoperative return of bowel function was quicker in the single layer group as compared to the double layer group in our study which accords with observations from previous studies [17,18]. This may be related to the intrinsic difference between the two techniques as highlighted above. In contrast, some authors observed no difference in the duration of return of bowel sounds between the two methods [19]. The clinical parameters that can accurately demonstrate the return to normal function of the anastomosed bowel further needs to be defined.
The length of hospital stay was shorter in the single-layer group as compared to the two-layer group (p-value <0.001); it might be due to the earlier resumption of bowel function in the former. Maurya SD et al., also observed shorter duration of stay in one-layer arm as compared to the two-layer arm (11.4 days versus 18.6 days, respectively) [17]. Another Indian study reported comparable length of hospital stay in both groups [9]. Burch JM et al., observed a 2-day shorter length of stay in the one-layer group although it was not statistically significant [8]. However, a Cochrane review inferred that both single and double-layer methods were comparable in terms of perioperative complications, mortality and hospital stay [3].
In the present study, the cost of suture material used was relatively more in the single layered group (564 INR vs. 480 INR) which might be the only factor favouring a double layered anastomosis. Due to difference in suture material used, other studies reported lower cost for the single-layer technique [8,9,15]. No significant difference has been observed between absorbable and non-absorbable sutures with respect to the strength of anastomosis [4]. The important characteristics of polydioxanone, an absorbable monofilament suture, are its better tensile strength retention, lower incidence of wound infection, and longer period of wound support owing to its slow absorption [18].
Since our conclusion was derived from smaller number of patients, further clinical trials with large sample sizes are required to establish significant advantage of single layered anastomosis over double layer in terms of postoperative morbidity, complications and hospital stay. Moreover, long term follow up is required to evaluate the late complications of intestinal anastomosis which include bowel stenosis, stricture or obstruction.
Conclusion
Keeping in view the shorter operative time, comparable complication rates, and lesser hospital stay duration for single layered extramucosal continuous anastomosis as compared to the conventional double layer method, it can be concluded from our study that former is equally safe and perhaps more cost effective than the latter. Thus, single layer technique may represent the optimal choice for routine surgical practice.
continuous variables expressed as Mean ± SD;
*Student’s t-test;
†Chi-square test