Peripheral Smear Review and Bone Marrow Biopsy Correlation
Adrian R. Bersabe1, James K. Aden2, Nathan M. Shumway3, Michael B. Osswald4
1 Fellow, Department of Internal Medicine: Hematology/Oncology, San Antonio Military Medical Centre, Fort Sam Houston, Texas, USA.
2 Statistician, Institute of Surgical Research, San Antonio Military Medical Centre, Fort Sam Houston, Texas, USA.
3 Staff Physician, Private Practice in Oncology, San Antonio, Texas, USA.
4 Staff Physician, Department of Internal Medicine: Hematology/Oncology, San Antonio Military Medical Centre, Fort Sam Houston, Texas, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Adrian R. Bersabe, Fellow, Department of Internal Medicine: Hematology/Oncology, San Antonio Military Medical Center, Fort Sam Houston, Texas, USA, 3551 Roger Brooke Drive, Fort Sam Houston, Texas-78234
E-mail: adrian.r.bersabe.mil@mail.mil
Introduction
Peripheral Blood Smear (PBS) interpretation is a useful skill for Haematology/Oncology Clinicians (HOC).
Aim
To explore practice patterns of PBS utilization for all benign haematology diagnosis in a non-simulated environment and to evaluate how it may guide the HOC in determining further work up and whether or not to perform a Bone Marrow Biopsy (BMB).
Materials and Methods
A retrospective review was conducted on 451 outpatient referrals for benign haematology diagnosis. Patient demographics and diagnostic tests were recorded. We further analysed cases in which a blood smear was ordered or reviewed. In cases with PBS review, we recorded testing ordered by the HOC.
Results
Records of 451 patients met inclusion criteria. The median age was 55 with males representing 51.9% of the cohort. Distribution of disorders were 50.6% (n = 228) erythrocyte (RBC), 25.5% (n = 114) leukocyte (WBC), 11.3% (n = 51) platelet (PLT), and 12.8% (n = 58) “other.” A CBC was ordered in 82.7% of cases (373/451). A PBS was ordered in 47.4% of CBCs obtained (177/373, p<0.001). Of these, documentation occurred in 49.2% (87/177) which led to further testing 41.4% of cases (36/87). A BMB was performed in 11.5% (10/87) of cases in which a PBS was reviewed compared to 4.3% (16/373) of cases where BMB was performed without PBS review (p=.019).
Of the 36 cases in which PBS review led to testing, 10 BMBs (27.8%) were performed—all of which led to specific haematologic diagnosis. A specific diagnosis was found in 43.8% (7/16) BMBs performed without prior PBS review.
Conclusion
PBS interpretation is an important skill for HOCs. Haematology/Oncology (H/O) training programs should continue to teach this skill to increase proficiency in order to help guide diagnostic evaluation of various haematologic disorders.
Blood platelets, Erythrocyte, Leukocyte, Peripheral blood
Introduction
The practice of PBS interpretation is an extremely important diagnostic skill in the subspecialty of H/O and it enhances the clinicians’ understanding of how to appropriately interpret laboratory results in conjunction with the entire clinical picture [1,2]. PBS examination may provide further insight into the aetiologic basis of many haematologic conditions such as various aetiologies of anaemia and haemoglobinopathies. Physician review of the a PBS can also be helpful in cases of platelet disorders, leukaemias, lymphomas, and bone marrow failure as distinct abnormalities may be noted leading to timely and accurate diagnosis, further evaluation, and potential treatment [1,3-9]. BMB are another important procedural skill used by HOC for the evaluation of both haematologic and non haematologic disorders. Depending on the clinical presentation, and sometimes, PBS interpretation, a clinician may determine if a BMB is indicated [10].
There has been a relatively recent push for haematologists to make it regular practice to become more proficient in routinely reviewing and correctly interpreting peripheral smears [11]. However, in today’s era of sophisticated automated blood cell-analysers, routine analysis of blood smears by clinicians is becoming less common. Over the past century automated haematology analysers have decreased the proportion of blood-count samples that require peripheral smear review [3,12,13]. Common laboratory practice is to review only specimens that the automated instruments have flagged for review due to distributional, morphologic, or instrumental error. In these instances an experienced laboratory technician followed by an assistant laboratory manager and/or a haematopathologist reviews the sample that later disseminates the information to the clinician [2,3,7,8,11]. Thus, many ordering clinicians, now rely on the laboratory for accurate interpretation of the PBS by qualified laboratory technologists and/or haematopathologists as this routine practice can be time consuming and labour-intensive [2,3,7,14].
To our knowledge, there is currently no literature describing how often HOCs in an accredited training program routinely interpret PBS or how often their interpretations lead to further diagnostic studies. However, one study by Simmons JO et al., simulated the initial work up of common anaemia wherein 65 clinicians were asked to review 12 case histories and subsequently review associated peripheral smears. They were then asked to identify morphologic features on the PBS and then instructed to select from a list their diagnosis and work up plans based on the available information and their interpretation of the PBS. Presence or absence of morphologic findings in PBS review was correctly identified 82% of the time. These authors reported that the number of further diagnostic tests was not affected by PBS review suggesting that this skill does not add value to the work up of common anaemia [15].
The aim of this study was to explore practice patterns of PBS utilization for all benign haematology diagnosis in a non-simulated environment and to evaluate how it may guide the HOC in determining further work up and whether or not to perform a BMB. Furthermore, in the cases where a BMB was performed, we examined the correlation of abnormal bone marrow results with the clinician’s documentation of abnormal PBS findings. Practice patterns between staff and fellow HOC were also compared.
Materials and Methods
A retrospective review was conducted on 474 consecutive, initial outpatient referrals for benign haematology diagnosis (ICD-9 codes 280-289) evaluated by seven staff physicians and nine fellows from Aug 2011 to May 2012. Adults from age 18 to 85 were included. Patient demographics and diagnostic tests were recorded. In cases with PBS review, we recorded further testing ordered by the HOC. We also assessed whether staff or fellow clinicians were more likely to review and document their PBS findings. A total of 23 patients were excluded due to age criteria or no data was available within the Electronic Medical Record (EMR).
The probability of events in the ordering and review of blood smears in an accredited H/O fellowship program was reported as the estimate of a binomial probability and its 95% confidence interval.
Statistical Analysis
The data was summarized using percentages and counts. Chi-Squared tests or Fisher’s-Exact test were used for analysis whichever is most appropriate. Significance for results was established when p-values were less than 0.05.
Results
Four hundred and fifty-one records met inclusion criteria. Patient’s demographics and distribution of diagnosis by peripheral blood cell type are presented in [Table/Fig-1]. The five most common diagnosis were anaemia, unspecified (n = 96, 21.3%), iron deficiency anaemia (n = 64, 14.2%), leukocytosis, unspecified (n = 49, 10.9%), thrombocytopenia (TCP), unspecified (n = 48, 10.6%), and leukopenia, unspecified (n = 21, 4.7%).
Characteristics of outpatient benign haematology referrals.
| Number of records studied | 451 |
| Age(median) | 55 |
| Male | 234 (52%) |
| Race/Ethnicity Caucasian African American Other | 200 (44%)106 (24%)145 (32%) |
| Diagnosis Erythrocyte (RBC) disorders Leukocyte (WBC) disorders Platelet (PLT) disorders Other | 228 (51%)114 (25%)51 (11%)58 (13%) |
A CBC was ordered in 82.7% cases (373/451). A PBS was ordered in 47.4% of cases that the provider ordered a CBC. A PBS was most likely to be ordered for RBC disorders when compared to WBC disorders, PLT disorders, and “other” diagnosis as depicted in the flow diagram, p≤0001 [Table/Fig-2]. HOCs documented their PBS findings within the EMR in 49.2% of cases in which they were ordered. Two hundred and twenty-nine CBCs were ordered by seven staff physicians, and 138 CBCs were ordered by nine fellows during the period of this review. There was no significant difference in practice patterns of ordering a PBS between staff (45.9%, 105/229) and fellow physicians (52.2%, 72/138), p=0.28. The likelihood that a staff physician documented their PBS findings (51.4%, 54/105) did not differ from the likelihood that fellows documented their PBS findings (45.8%, 33/72), p=0.54).
CBC and PBS ordered for outpatient benign. haematology referrals.
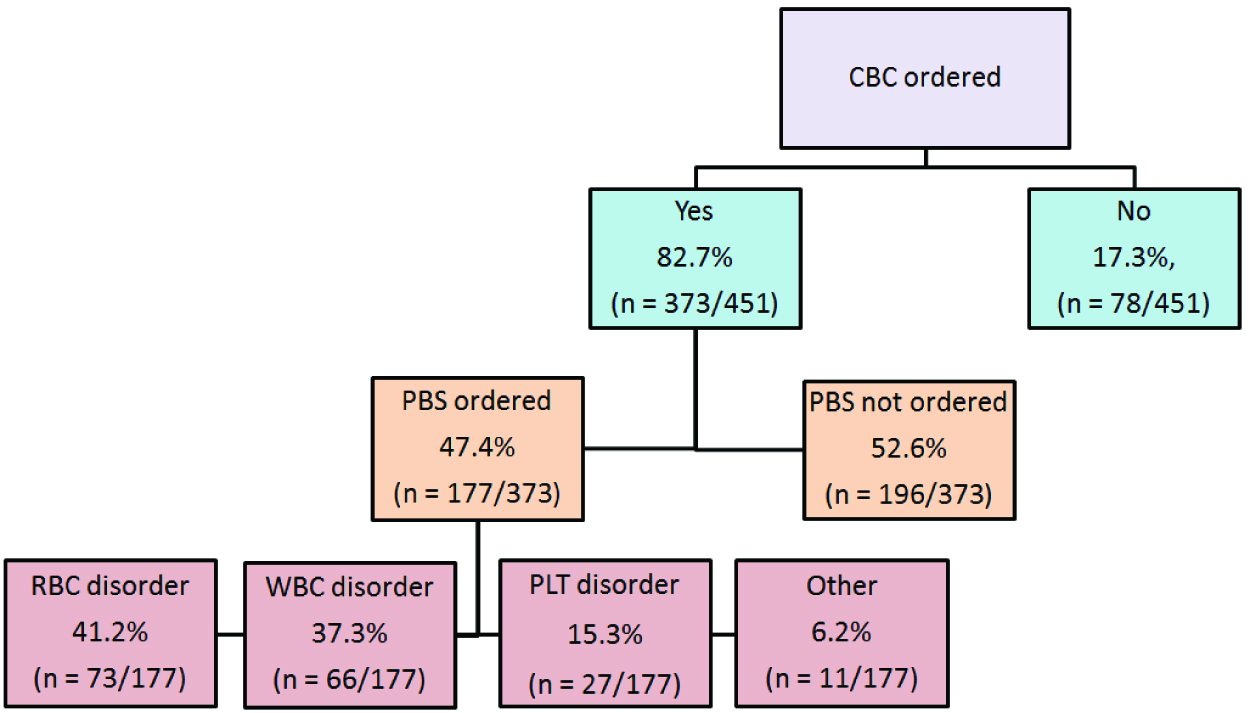
Further diagnostic evaluation with laboratory testing, imaging, and/ or other specialty referral occurred in 41.4% of cases that the HOC documented specific PBS findings. In total, PBS review lead to further diagnostic testing in 8% (36/451) of the entire cohort. Of the 36 cases in which PBS review led to testing, 10 (27.8%) were RBC disorders, 17 (47.2%) were WBC disorders, six (16.7%) were PLT disorders, and three (8.3%) were categorized as “other” [Table/Fig-3]. Additional non-laboratory tests included one Gastroenterology referral for anaemia, an ultrasound to evaluate for splenomegaly, and 10 BMBs.
PBS and further diagnostic evaluation for outpatient benign haemat ology referrals.
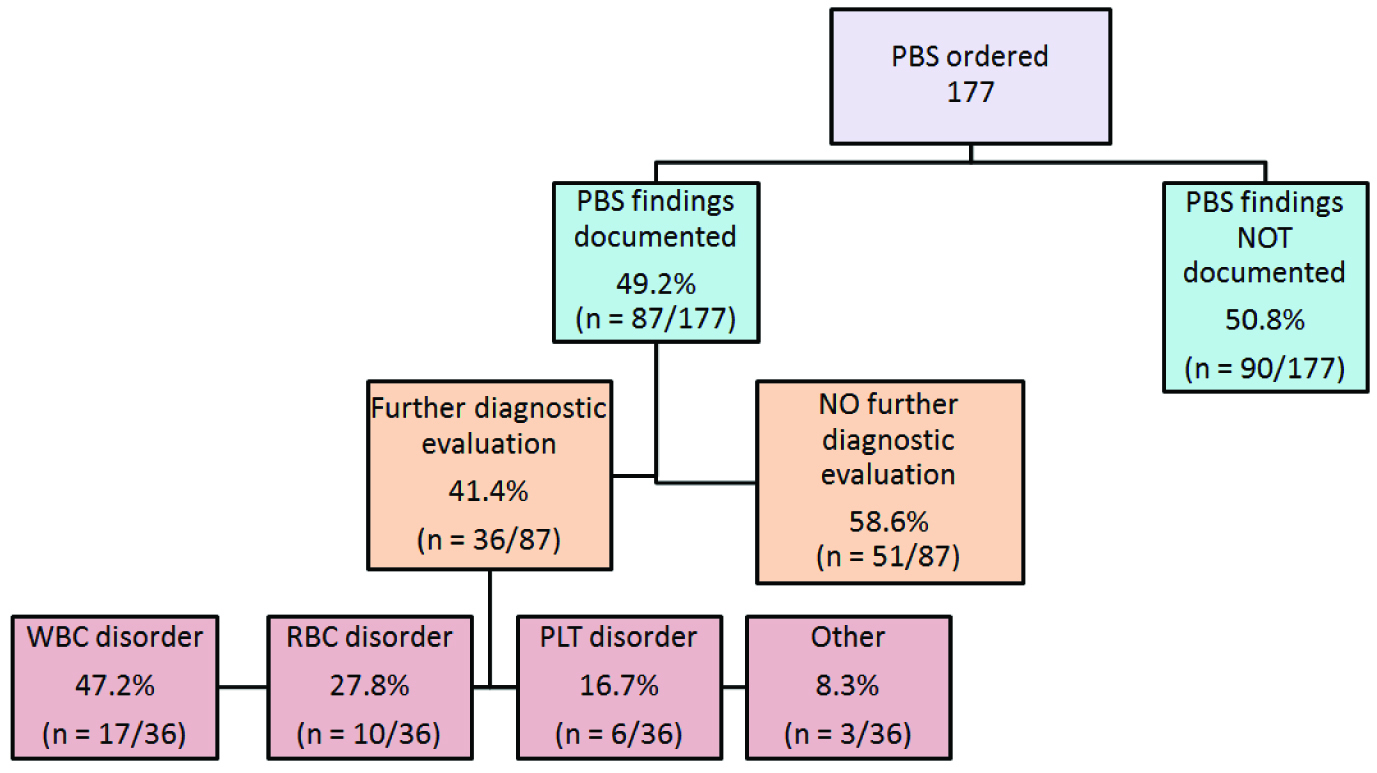
A BMB was performed in 5.8% (26/451) of all initial benign haematology referrals. Of the BMBs performed after PBS interpretation (11.5%, 10/87), one was obtained for a RBC disorder showing Primary Myelofibrosis (PMF). Four BMBs for WBC disorders revealed two cases of chronic myelocytic leukaemia, one myelproliferative disease, and one toxin-mediated marrow suppression. Three BMBs performed for low PLTs aided in the diagnosis of aplastic anaemia, idiopathic thrombocytopenia purpura, and large granular lymphocytic leukaemia. The BMBs performed for two cases in “other” diagnosis carried ICD-9 codes for splenomegaly and Monoclonal Gammopathy of Undetermined Significance (MGUS), and the BMB confirmed PMF and MGUS.
In 4.3% of cases (16/373), the HOC performed a BMB without prior PBS review. Of these, four (25%) were initially referred for a RBC disorder with a BMB leading to the diagnosis of T-cell LGL leukaemia. Five (31.3%) were referred for a WBC disorder revealing one case of chronic lymphocytic leukaemia and another lymphocytic eosinophilia. Four (25%) were referred for thrombocytopenia with BMB aiding in the diagnosis of myelodysplastic syndrome, ITP, and metastatic stage IV carcinoma of unknown primary. Lastly, three of these referrals were categorized as “other” with BMB confirming the diagnosis of multiple myeloma in one case. Thus, a specific diagnosis was found in 43.8% (7/16) of BMB performed without prior PBS review. A BMB was more likely to be diagnostic in cases that the HOC used PBS findings to determine the necessity of a BMB than in cases where the HOC performed a BMB without prior PBS review (p=0.0265, p=0.012, respectively).
Discussion
Examination of the PBS is an important skill for clinicians—especially Haematologists [3,11,16]. Various case reports also highlight the significance of PBS evaluation aiding in the diagnosis of rare or difficult cases as well as cases requiring immediate diagnosis and treatment [17-20]. However, some authors suggest that PBS review may not be as useful and may even lead the clinician to order more inappropriate tests. This was seen particularly in common anaemia diagnosis such as iron deficiency, vitamin B12 deficiency, and thalassaemias [15,21].
This retrospective study sought out to describe practice patterns of PBS utilization for benign haematology referrals by HOCs an accredited H/O training program. We investigated the frequency in which the HOC ordered and actually documented their interpretation of the PBS within the EMR and the likelihood that this clinical skill led to further evaluation and/or diagnosis. A CBC was ordered in the majority of benign haematology referrals, and of these, a PBS was ordered in less than half of cases. HOC documentation of PBS findings occurred in less than half of cases that it was determined PBS review should be done. The HOC was significantly more likely to order a PBS for disorders relating to RBC, followed by WBC, PLTs, and “other” diagnosis, respectively. The likelihood of HOC documentation of PBS interpretation did not differ based on the haematologic diagnosis, and there were no significant differences in PBS ordering or documentation of PBS findings between staff and fellow providers.
Further diagnostic testing was ordered in nearly half cases (41.4%) in which the HOC documented PBS findings. A BMB was ordered in close to a third of these cases, and a definitive diagnosis was made in all BMBs obtained after PBS examination. However, when a BMB was performed without prior PBS review, definitive marrow findings were seen in less than 50% of cases. There was a higher likelihood that BMB was more likely to be performed and lead to a specific haematologic diagnosis after HOC PBS review than without PBS review.
Microscopic examination and interpretation of a PBS serves to ensure that no clinically significant finding is missed and to aid in accurate diagnosis especially when interpreted by a haematopathologists, pathologist, or haematologist with training and experience [22]. It should be noted that interpretation of PBS is a requirement by the Accreditation Council for Graduate Medical Education (ACGME) in Haematology fellowship programs. To our knowledge, however, there are no standardized criteria for PBS review within H/O training programs. Other than an abnormal CBC and differential, which are the major determinants leading to PBS review, there are other factors such as clinician concerns and level of reviewer training and experience which may lead to PBS review [22]. The level of training of the HOC did not seem to impact the likelihood of PBS review in this study.
limitation
Some limitations of this review include those that are commonly inherent of retrospective studies. Furthermore, the HOC often did not provide specific reasoning regarding why or why not a PBS was ordered, and if ordered, why specific PBS findings were not documented in the EMR. Lastly, we did not evaluate whether or not PBS review led cost-effective diagnostic evaluation.
Conclusion
While many may agree that clinician examination of the PBS may not be necessary in all benign haematology consultations, our data suggests that the practice of PBS interpretation remains an important and useful skill for HOCs. In our study, we found that the diagnostic yield of a BMB was higher when prior PBS was reviewed led to the decision to perform the procedure. This data suggests that review of the PBS by clinicians may aid in more appropriately identifying patients for BMB in order to obtain a definitive diagnosis. Haematology/Oncology training programs should continue to teach this skill and work to become more experienced in PBS interpretation to guide diagnostic testing and potential management of various haematologic disorders.
[1]. Jen P, Woo B, Rosenthal PE, Bunn F, Loscalzo A, Goldman L, The value of the peripheral blood smear in anaemic patientsArch Intern Med 1983 143:1120-25. [Google Scholar]
[2]. Pierre RV, Peripheral blood film review:The demise of the eye-count leukocyte differentialClin Lab Med 2002 22:279-97. [Google Scholar]
[3]. Bain BJ, Diagnosis from the blood smearN Engl J Med 2005 353:498-507. [Google Scholar]
[4]. Child JA, Haematology reportingNurs Times 1975 71:1045-48. [Google Scholar]
[5]. Froom P, Havis R, Barak M, The rate of peripheral blood smear reviews in outpatientsClin Chem Lab Med 2009 47:1401-05. [Google Scholar]
[6]. Gulati G, Song J, Florea AD, Gong J, Purpose and criteria for blood smear scan, blood smear examination, and blood smear reviewAnn Lab Med 2013 33:1-7. [Google Scholar]
[7]. Javidian P, Garshelis L, Powers P, Pathologist review of the peripheral smear:A mandatory quality assurance activity?Clin in Lab Med 1993 13:853-61. [Google Scholar]
[8]. Jenkins C, Hewamana S, The blood film as a diagnostic toolBr J of Hosp Med (Lond) 2008 69:144-47. [Google Scholar]
[9]. Peterson P, Blomberg DJ, Rabinovitch A, Cornbleet PJ, Physician review of peripheral blood the smear:When and whyLab Hematol 2001 7:175-79. [Google Scholar]
[10]. Kaur M, Rana AP, Kapoor S, Puri A, Diagnostic value of bone marrow aspiration and biopsy in routine hematology practiceJ Clin Diagn Res 2014 8:13-16. [Google Scholar]
[11]. Shattil SJ, A (blood) smear campaignBlood 2003 101:2453 [Google Scholar]
[12]. Barnes PW, McFadden SL, Machin SJ, Simson E, The International Consensus Group for Hematology Review:Suggested criteria for action following automated CBC and WBC differential analysisLab Hematol 2005 11:83-90. [Google Scholar]
[13]. Novis DA, Walsh M, Wilkinson D, St Louis M, Ben-Ezra J, Laboratory productivity and the rate of manual peripheral blood smear reviewArch Pathol Lab Med 2006 130:596-601. [Google Scholar]
[14]. Sandhaus LM, Wald DN, Kenan J, Steele EL, Meyerson HJ, Measuring the clinical impact of pathology reviews of blood and body fluid smearsArch Pathol Lab Med 2006 131:468-72. [Google Scholar]
[15]. Simmons JO, Noel GL, Diehl LF, Does review of peripheral blood smears help in the initial workup of common anaemias?J Gen Intern Med 1989 4:479-81. [Google Scholar]
[16]. Adewoyin AS, Nwogoh B, Peripheral blood film—A reviewAnn Ibd Pg Med 2014 12:71-79. [Google Scholar]
[17]. Rajajee S, Sathyasekaran M, Shankar J, Dhathathri L, Dhathathri A, Importance of screening the peripheral smearIndian J Pediatr 2002 69:821-22. [Google Scholar]
[18]. Geier C, Davis J, Siegel M, Severe human monocytic ehrlichiosis presenting with altered mental status and seizuresBMJ Case Rep 2016 2016:pii:bcr2016215967 [Google Scholar]
[19]. Abus-Hishmeh M, Sattar A, Zarlasht F, Ramadan M, Abdel-Rahman A, Hinson S, Systemic lupus erythematosus presenting as refractory thrombotic thrombocytopenic purpura:A diagnostic and management challenge. A case report and concise review of the literatureAm J Case Rep 2016 17:782-87. [Google Scholar]
[20]. Waheed N, Cheema HA, Suleman H, Mushtaq I, Fayyaz Z, Chanarin-Dorfman SyndromeJ Coll Physicians Surg Pak 2016 26:787-89. [Google Scholar]
[21]. Fairbanks VF, Is the peripheral blood film reliable for the diagnosis of iron deficiency anaemia?Am J Clin Pathol 1971 55:447-51. [Google Scholar]
[22]. Gulati G, Song J, Gong J, Purpose and criteria for blood smear scan, blood smear examination, and blood smear reviewAnn Lab Med 2013 33:1-7. [Google Scholar]