Role of Anaemia and Magnesium Levels at the Initiation of Tuberculosis Therapy with Sputum Conversion among Pulmonary Tuberculosis Patients
Yuthika Agrawal1, Vipin Goyal2, Abhishek Singh3, Sandhya Lal4
1 Senior Resident, Department of Biochemistry, Shaheed Hasan Khan Mewati Government Medical College, Nalhar, Haryana, India.
2 Assistant Professor, Department of Chest and TB, Shaheed Hasan Khan Mewati Government Medical College, Nalhar, Haryana, India.
3 Assistant Professor, Department of Community Medicine, Shaheed Hasan Khan Mewati Government Medical College, Nalhar, Haryana, India.
4 Senior Resident, Department of Biochemistry, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yuthika Agrawal, C2-404, Shaheed Hasan Khan Mewati Government Medical College, Nalhar-122107, Haryana, India.
E-mail: yuthika.agrawal@yahoo.in
Introduction
Both pulmonary Tuberculosis (TB) and anaemia are prevalent in India. Magnesium levels also influence TB. There is limited and inconsistent literature on the association among anaemia, serum magnesium levels and sputum conversion during tuberculosis treatment.
Aim
To study the effect of anaemia and serum magnesium levels on sputum conversion in pulmonary TB patients.
Materials and Methods
One hundred each of newly diagnosed sputum smear positive Pulmonary Tuberculosis (PTB), sputum smear negative PTB patients initiated on Directly Observed Treatment Short Course chemotherapy (DOTS) and healthy age and sex matched controls were recruited in the study. Patients were followed up prospectively until completion of first two months of intensive phase. Patients were evaluated before initiation of TB treatment by performing the complete blood counts with peripheral blood smear, serum biochemistry, serum iron, serum magnesium, serum ferritin and microscopic examination of sputum. After giving two months of Antitubercular Therapy (ATT), sputum smears were re-examined for presence of acid fast bacilli. Haemoglobin values less than 13 g/dl in males or 12 g/dl in females was defined as anaemia. Mean and Standard deviations were calculated. Independent t-test was used to compare between the groups.
Results
Serum iron and serum ferritin was significantly lower in sputum positive PTB as compared to sputum negative PTB and controls. Anaemia was present in 162 (81%) patients of the study PTB cases. About 60% of anaemia in sputum positive cases was iron deficiency anaemia. Serum magnesium level was significantly lower in sputum positive PTB as compared to sputum negative PTB and controls though not in hypomagnesemic range. Delayed sputum smear conversion occurred in 12 (12%) sputum positive PTB patients. Of these, eight had severe iron deficiency anaemia, four with moderate anaemia. All 12 delayed sputum smear conversion had serum magnesium levels < 1.7 mg/dl (below normal reference range) (mean 1.42 ±0.22 mg/dl).
Conclusion
Sputum was found to be positive even after two months of ATT course because of baseline anaemia and lower levels of serum magnesium. Further multicentric studies are warranted to study mechanisms for TB associated anaemia and possible role of intervention for anaemia in TB patients. One needs to find out the mechanisms behind the role of anaemia and lower magnesium levels in delaying the sputum smear conversion in order to lay the foundation of effective interventions. Randomized controlled trials are warranted to generate higher levels of evidences to support our findings.
Anti tubercular treatment, Haemoglobin, Serum magnesium
Introduction
The second most common cause of deaths in the world from infectious diseases is TB [1,2]. In 2011 worldwide, 8.7 million new active cases of TB were seen and 1.4 million deaths were estimated to be due to TB [2]. The situation is worse in India where TB disproportionately affects the young. India accounts for 1/5th of the global burden, with 1.8 million developing the disease each year and nearly 0.4 million dying due to TB annually [3].
This data indicates the need to strengthen strategies for infection control, identification and management of TB patients, in addition to effective chemotherapy to reduce TB related morbidity and mortality. Bacilli load falls drastically in the expelled sputum soon after initiating TB treatment, containing rifampicin and isoniazid [4-6]. It cuts down the chain of transmission thus, reducing the further spread of tuberculosis [7-10]. Majority of patients become smear or culture negative after two to three months of treatment with DOTS therapy. But still cultures of approximately 10% of TB patients remain positive after two months of TB chemotherapy [7]. This group of patients maintain the chain of transmission. This plays an important role in persistence of infectiousness. It is also observed that longer smear conversion time is more closely associated with poor TB treatment outcomes and relapse within two years of follow up [11,12]. There are certain risk factors for delayed smear conversion. A few of these risk factors are cavitatory lesions, high Acid Fast Bacilli (AFB) load, multi drug resistant TB, geriatric patients diabetes and duration of symptoms before initiation of treatment [13,14].
About 1%-8% of world’s population is anaemic. Anaemia is third leading cause of YLD (years lived with disability) worldwide and has caused >600 YLD/100,000 people [15]. Incidence and prevalence of anaemia varies from place to place [15,16] and that among TB patients has reported great variation ranging between 30%-94% [17-21]. Case contol studies have shown that anaemia more frequently occurs among subjects having TB as compared to those not having TB (healthy controls) [22]. On the other hand, association of anaemia has been observed with more severe forms of TB [22] and unfavourable TB outcomes [18,20,23]. There is paucity of capricious literature on relationship between anaemia and sputum smear conversion. One set of evidence came up with no association between anaemia and positivity of TB culture at one month of TB therapy [18], whereas another set of evidence observed higher mean haemoglobin following sputum smear conversion at two months of TB treatment compared to baseline haemoglobin [24].
Magnesium is the most abundant cation in the body next to potassium. Only 0.3% of total body magnesium exists in serum [3]. Serum or plasma magnesium is a better marker for magnesium imbalance as it is not expensive and easily available [25]. Magnesium is a part of hundreds of enzyme systems, plays a role in process of innate and acquired immune response, involved in synthesis of immunoglobulin as cofactor, role in immune cell adherence, antibody dependent cytosis, helps in binding of IgM lymphocyte, T-helper B-cell adherence and additional responses. Epidemiological data have shown that higher intake of magnesium is associated with lower incidence of respiratory problems. More recently, effect of magnesium on respiratory airways has been studied and it is observed that magnesium sulphate improves lung function and causes vasodilatation. But a few studies from past have shown inconclusive data of magnesium levels in PTB [3].
Hence, this prospective study was planned to examine the effect of anaemia and serum magnesium levels on sputum smear conversion, after giving two months of antituberculosis chemotherapy.
Materials and Methods
The present case-control study was planned and executed in the department of Chest and TB, Shaheed Hasan Khan Mewati Government Medical College, Nalhar, Haryana, India, during 2015-2016. Study participants were 100 new sputum positive PTB patients (defined as having presence of at least one Acid Fast Bacilli (AFB) in at least one sputum sample on microscopy), aged between 15 years and 60 years of age, 100 new sputum negative PTB and 100 healthy age and sex matched controls.
Informed consent was taken from all participants and ethical approval was taken from Institutional Ethics Committee. This sample size of 300 subjects was taken as per convenient sampling. The criterion for the sputum negative pulmonary tuberculosis was persistence of cough after two weeks of administration of antibiotics and positive finding on chest X-ray like cavitation and/or consolidation in upper lungs with sputum smear negative for AFB on repeated testing two times.
Ziehl–Neelsen stain was used in the process of preparing the sputum smears. These sputum smears were examined for presence of AFB at baseline and at two months of TB treatment in sputum positive PTB. HIV testing was also done. Sputum and blood samples were examined after obtaining consent from study participants. TB patients were treated with standard DOTS therapy for six months. ATT comprised of four drugs namely rifampicin, isoniazid, pyrazinamide and ethambutol in intensive phase. After the completion of the intensive phase, sputum smear microscopy for AFB is done. If sputum smear is negative for AFB, then patient is continued with rifampicin and isoniazid for four months in continuation phase. Patients who had sputum smear positive for AFB at two months of follow up were advised to take an extended intensive phase of ATT for another month. Old TB patients were excluded, who had history of complete ATT.
The outcome measure for this study was delayed sputum smear conversion, defined as sputum smear positive for AFB at two months of ATT. The primary exposure of interest was magnesium levels and anaemia at baseline, anaemia defined as per World Health Organization guidelines as haemoglobin <13 g/dl (males) or haemoglobin <12 g/dl (female) [26]. Anaemia was further categorized according to severity with the following haemoglobin cut off points: mild anaemia; 11-13 g/dl (male) and 11-12 g/dl (female), moderate anaemia; 8-11 (both sexes), severe anaemia; less than 8 g/dl for both sexes [26]. Ferritin was determined by chemiluminescence immunoassay, serum magnesium by xylidyle blue dye method. Peripheral blood smear was also performed.
Statistical Analysis
Results were expressed using appropriate statistical methods. Mean and Standard deviations were calculated. Independent t-test was used to compare between the groups. A p-value less than 0.05 were considered to be statistically significant.
Results
The median age of the participants was 45 (15-75) years. Most participants (67%) were males. Baseline characteristic of PTB patients are shown in [Table/Fig-1]. Five of PTB patients were found to be reactive to HIV.
Baseline characteristic of PTB patients.
| Characteristic | Sputum positive PTB | Sputum negative PTB |
|---|
| Age in years, | 45 (range 15-75) |
| Sex (M,F) | 67,33 |
| Blood urea (mg/dl) | 22.71+9.8 | 34.65+10.23 |
| Serum creatinine (mg/dl) | .69+.16 | .74 +.35 |
| Serum sodium (meq/dl) | 134.6 +4.2 | 135.9+4.6 |
| Serum potassium (meq/dl) | 3.9 +0.5 | 3.9+0.4 |
| Serum total calcium (mg/dl) | 8.9+0.5 | 8.5+0.7 |
| ALT (U/L) | 29.5±6.61 | 26.9±6.51 |
| AST (U/L) | 33.30±5.25 | 33.13±5.64 |
Serum iron and serum ferritin was significantly lower in sputum positive PTB as compared to sputum negative PTB and controls as shown in [Table/Fig-2]. Anaemia was present in 162 (81%) patients of the PTB cases. A total of 104 (52%) had moderate to severe anaemia. Of these, 71 of sputum were positive while 33 of sputum negative had moderate to severe anaemia. A 60% of anaemia in sputum positive cases was iron deficiency anaemia characterised by low ferritin and low iron levels with microcytic hypochromic anaemia in peripheral smear. While 22% of anaemic sputum negative cases had iron deficiency anaemia.
Anaemia parameters and serum magnesium levels.
| Parameter | Sputum positive PTB | Sputum negative PTB | Controls |
|---|
| Hb (g/dl) | 9.02+1.9 | 11.2+2.3 | 14.2+3.2 |
| Iron (μg/dl) | 29.6+10.2*/** | 56.2+10.4** | 107.6+12.8 |
| Ferritin (ng/ml) | 32.5+16.4*/** | 227.8+28.28 | 250.7+29.54 |
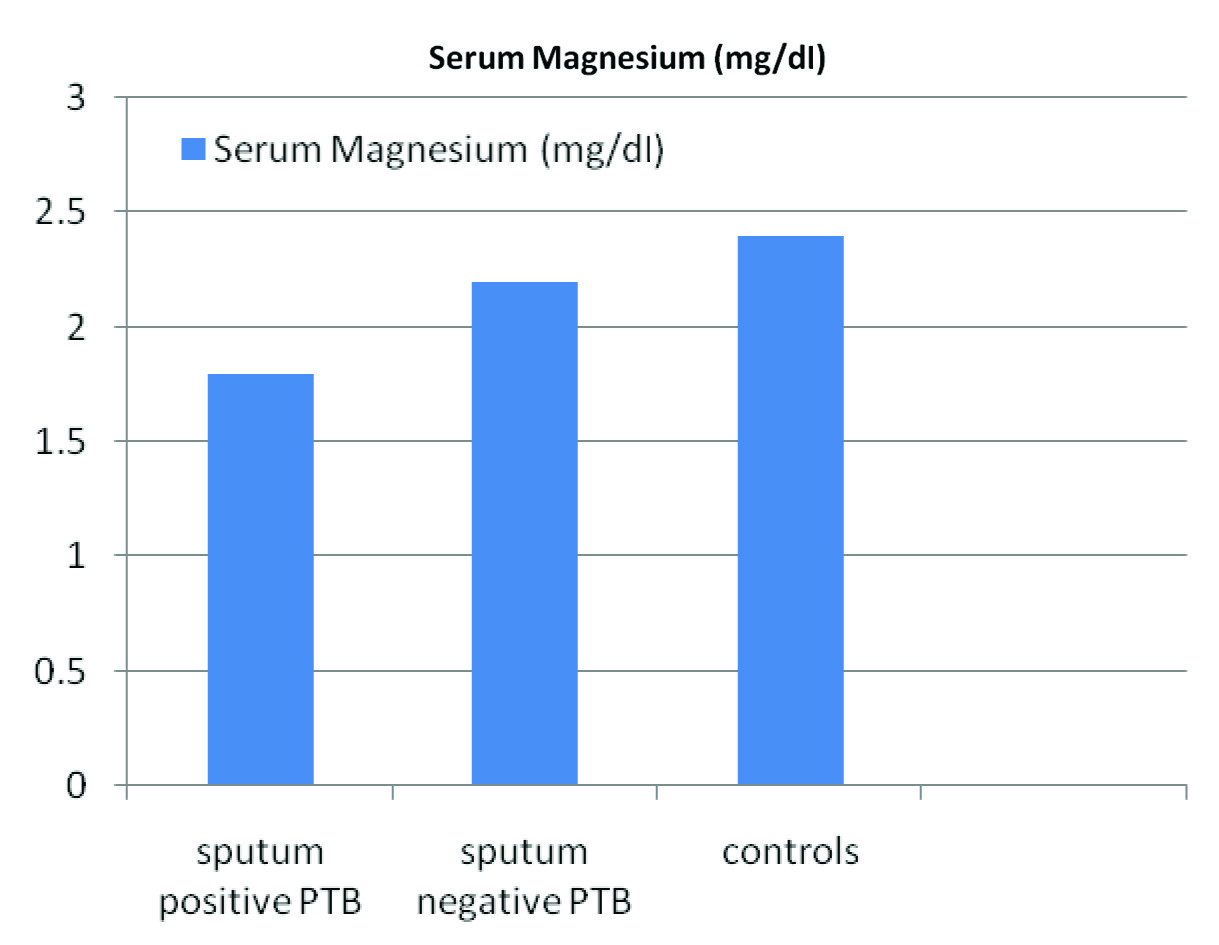
| Magnesium (mg/dl) | 1.8+.3*/** | 2.2+.4** | 2.4+0.6 |
significant with respect to Sputum negative PTB
significant with respect to Controls
Serum magnesium level was significantly lower in sputum positive PTB as compared to sputum negative PTB and controls (p-value <0.05) though not in hypomagnesemic range [Table/Fig-2,3]. Delayed sputum smear conversion occurred in 12 (12%) sputum positive PTB patients. Eight of these patients had severe iron deficiency anaemia while four had moderate anaemia. [Table/Fig-4] shows the association between anaemia at the time of enrollment and delayed sputum smear conversion at two months of ATT. All 12 delayed sputum smear conversion had serum magnesium levels < 1.7 mg/dl (below normal reference range) (mean 1.42 ±0.22 mg/dl).
Serum magnesium levels in sputum positive PTB, sputum negative PTB and controls
Association between anaemia at the time of enrollment and delayed sputum smear conversion at two months of ATT.
| Anaemia | Sputum positive PTB(100) | Sputum negative PTB(100) |
|---|
| Mild | 21 | 37 |
| Moderate | 50 | 26 |
| Severe | 21 | 7 |
| Sputum delayed conversion with mild anaemia | 0 | - |
| Sputum delayed conversion with moderate anaemia | 8/50 | - |
| Sputum delayed conversion with severe anaemia | 12/21 | - |
Ninety two sputum positive PTB patients were found to be anaemic, out of which 21 had severe anaemia. Out of total 21 severely anaemic sputum positive PTB patients, 12 had delayed conversion of sputum smear. Eight of the sputum positive PTB patients had delayed conversion of sputum smear among 71 patients having mild to moderate anaemia. Thus, this delayed conversion was found to be statistically highly significant (p<0.001) [Table/Fig-4].
Out of the 100 sputum positive PTB patients, 30 had serum magnesium levels <1.7 mg/dl. Of these, 12 had delayed conversion of sputum smear. Seventy sputum positive PTB patients had serum magnesium levels >1.7 mg/dl. Eight of these patients also had delayed conversion of sputum smear. Thus this delayed conversion was found to be statistically significant (P<0.05) [Table/Fig-5].
Association between serum magnesium levels at the time of enrollment and delayed sputum smear conversion at two months of ATT.
| Variable | Sputum positive PTB (100) |
|---|
| Sputum delayed conversion with Magnesium level <1.7 mg/dl | 12/30 |
| Sputum delayed conversion with Magnesium level >1.7 mg/dl | 8/70 |
p<0.05
Discussion
Early diagnosis and effective treatment of TB remains the key to success for infection control. For assessment of outcome of TB treatment, sputum smear microscopy at two months of DOTS treatment is a very important parameter. In this study, we made an attempt to find out probable association of anaemia and serum magnesium levels with sputum smear conversion after two months of ATT. Our discussion will focus on observations of these two variables.
First, anaemia and lower serum magnesium levels are associated with delayed sputum smear conversion; especially iron deficiency anaemia (low ferritin and microcytic hypochromic picture in peripheral smear) at two months of anti TB therapy. Secondly, there was increase in number of cases for delayed sputum conversion with increase in severity of anaemia. The present study findings were in contradiction to the study done by Isanaka et al., as they did not find any association between anaemia and sputum culture conversion after giving one month of ATT [18].
Variation in the results could be due to following reasons. Firstly, in the study, majority of subjects had mild to moderate anaemia [18]. As observed in this study, subjects with milder forms of anaemia were at a lower risk for delayed sputum conversion. This finding suggests inclusion of more study subjects to achieve optimum statistical power to detect the smaller effect. Secondly, variation in the result could be due to another method of outcome assessment. In this study, we used sputum smear microscopy whereas, previous study adopted culture conversion. Another study from Russia [23] showed definitive association between sputum non conversion among TB patients and persistent anaemia during TB treatment. That study observed lower mean haemoglobin among patients with positive sputum smear compared to those with negative sputum smear at three months.
In the present study, serum magnesium level were similar to study conducted by Jain MK et al., [27]. Possible reason can be as narrated by Oladipo OO et al., that hypomagnesemia can be due to malnutrition in PTB patients [28].
We are not clear about mechanisms explaining the association of delayed sputum conversion with baseline anaemia and lower serum magnesium. It is a known fact that tuberculosis causes anaemia but why a few patients do not become anaemic, still remain blurred. Evidences from previous studies have shown that malnourished TB patients had lower mean levels of haemoglobin, magnesium (as stated earlier) and zinc, as compared to controls, malnourished controls and well-nourished TB patients [22].
Magnesium and iron supplements may be effective in patients of hypomagnesemia and iron deficiency anaemia in PTB, and may achieve better therapeutic results, but further investigation is needed.
There are certain strengths and weaknesses of this investigation. Regarding strong points of our study, firstly we tried to generate evidence for an under explored issue like association of anaemia and serum magnesium levels with sputum smear conversion after two months of anti-TB treatment. Paucity of literature warrants this probe. Very few related studies are available in the literature and none from India. Second, keeping prevalence of anaemia among TB patients in mind, we categorized severity of anaemia in study subjects which provided us an opportunity for setting the priorities. Third, application of our findings at community level may lead to reduction in the transmission of TB infection thus, reduced mortality and morbidity associated with TB.
Limitation
Our study had some limitations as well. First, small sample size is an evident limitation of this study. Second, mycobacteria cultures should also have been performed after giving ATT for two months, as non viable mycobacteria can give false positive results. Though, in most cases, it is seen that smear turns negative prior to culture and almost all sputum smear positive for AFB on microscopy after two months of ATT show culture positivity. Thirdly, bias is possible due to non-adherence to ATT as it is an important factor for sputum conversion and cure of TB.
Conclusion
An anaemia and lower serum magnesium level at the initiation of TB treatment is significantly associated with delayed sputum smear conversion among sputum positive TB patients. Also, there was increase in number of cases for delayed sputum conversion with increase in severity of anaemia. One needs to find out the mechanisms behind the role of anaemia and lower magnesium levels in delaying the sputum smear conversion in order to lay the foundation of effective interventions. Randomized controlled trials are warranted to generate higher levels of evidences to support our findings.
*significant with respect to Sputum negative PTB
**significant with respect to Controls
p<0.05
[1]. Tuberculosis:a global emergencyWorld Health Forum 1993 14(4):438 [Google Scholar]
[2]. World Health Organization (WHO)Global Tuberculosis Report 2012 2012 accessed on 9th October 2016GenevaWorld Health OrganizationAvailable at: http://www.who.int/iris/bitstream/10665/75938/1/9789241564502_eng.pdf [Google Scholar]
[3]. Das B, Prasanna C, Thimmaraju KV, Sumeru S, Raju SM, Study of serum magnesium values in pulmonary tuberculosis patientsJour Adv Res Med Sci 2012 4(1):54-57. [Google Scholar]
[4]. Shaw JB, Wynn-Williams N, Infectivity of pulmonary tuberculosis in relation to sputum statusAm Rev Tuberc 1954 69(5):724-32. [Google Scholar]
[5]. Rouillon A, Perdrizet S, Parrot R, Transmission of tubercle bacilli:The effects of chemotherapyTubercle 1976 57(4):275-99. [Google Scholar]
[6]. Jindani A, Dore´ CJ, Mitchison DA, Bactericidal and sterilizing activities of antituberculosis drugs during the first 14 daysAm J Resp Crit Care Med 2003 67(10):1348-54. [Google Scholar]
[7]. Fitzwater SP, Caviedes L, Gilman RH, Coronel J, LaChira D, Salazar C, Pro-longed infectiousness of tuberculosis patients in a directly observed therapy short-course program with standardized therapyClin Infect Dis 2010 51(4):371-78. [Google Scholar]
[8]. Fortún J, Martín-Dávila P, Molina A, Navas E, Hermida JM, Cobo J, Sputum conversion among patients with pulmonary tuberculosis:are there implications for removal of respiratory isolation?J Antimicrob Chemother 2007 59(4):794-98. [Google Scholar]
[9]. Long R, Bochar K, Chomyc S, Talbot J, Barrie J, Kunimoto D, Relative versus absolute non-contagiousness of respiratory tuberculosis on treatmentInfect Control Hosp Epidemiol 2003 24(11):831-38. [Google Scholar]
[10]. Parikh R, Nataraj G, Kanade S, Khatri V, Mehta P, Time to sputum conversion in smear positive pulmonary TB patients on category I DOTS and factors delaying itJ Assoc Physicians India 2012 60:22-26. [Google Scholar]
[11]. Chien JY, Chen YT, Shu CC, Lee JJ, Wang JY, Yu CJ, Outcome correlation of smear-positivity for acid-fast bacilli at the fifth month of treatment in non-multidrug-resistant TBChest 2013 143(6):1725-32. [Google Scholar]
[12]. Tiwari S, Kumar A, Kapoor SK, Relationship between sputum smear grading and smear conversion rate and treatment outcome in the patients of pulmonary tuberculosis undergoing dots–a prospective cohort studyIndian J Tuberc 2012 59(3):135-40. [Google Scholar]
[13]. Güler M, Unsal E, Dursun B, Aydln O, Capan N, Factors influencing sputum smear and culture conversion time among patients with new case pulmonary tuberculosisInt J Clin Pract 2007 61(2):231-35. [Google Scholar]
[14]. Senkoro M, Mfinanga SG, Morkve O, Smear microscopy and culture conversion rates among smear positive pulmonary tuberculosis patients by HIV status in Dar es Salaam, TanzaniaBMC infectious diseases 2010 10:210 [Google Scholar]
[15]. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010:a systematic analysis for the Global Burden of Disease Study 2010Lancet 2012 380(9859):2163-96. [Google Scholar]
[16]. McLean E, Cogswell M, Egli I, Wojdyla D, de Benoist B, Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System 1993–2005Public Health Nutrition 2009 12:444-54. [Google Scholar]
[17]. Lee SW, Kang YA, Yoon YS, Um SW, Lee SM, Yoo CG, The prevalence and evolution of anaemia associated with tuberculosisJ Korean Med Sci 2006 21(6):1028-32. [Google Scholar]
[18]. Isanaka S, Mugusi F, Urassa W, Willett WC, Bosch RJ, Villamor E, Iron deficiency and anaemia predict mortality in patients with tuberculosisJ Nutr 2012 142(2):350-57. [Google Scholar]
[19]. Saathoff E, Villamor E, Mugusi F, Bosch RJ, Urassa W, Fawzi WW, Anaemia in adults with tuberculosis is associated with HIV and anthropometric status in Dar es Salaam, TanzaniaInt J Tuberc Lung Dis 2011 15(7):925-32. [Google Scholar]
[20]. Hussain SF, Irfan M, Abbasi M, Anwer SS, Davidson S, Haqqee R, Clinical characteristics of 110 miliary tuberculosis patients from a low HIV prevalence countryInt J Tuberc Lung Dis 2004 8(4):493-99. [Google Scholar]
[21]. Olaniyi JA, Aken’Ova YA, Haematological profile of patients with pulmonary tuberculosis in Ibadan, NigeriaAfr J Med Med Sci 2003 32(3):239-42. [Google Scholar]
[22]. Karyadi E, Schultink W, Nelwan RH, Gross R, Amin Z, Dolmans WM, Poor micronutrient status of active pulmonary tuberculosis patients in IndonesiaJ Nutr 2000 130(12):2953-58. [Google Scholar]
[23]. Kourbatova EV, Borodulin BE, Borodulina EA, del Rio C, Blumberg HM, Leonard MKJr, Risk factors for mortality among adult patients with newly diagnosed tuberculosis in Samara, RussiaInt J Tuberc Lung Dis 2006 10(11):1224-30. [Google Scholar]
[24]. Morris CD, Bird AR, Nell H, The haematological and biochemical changes in severe pulmonary tuberculosisQ J Med 1989 73(272):1151-59. [Google Scholar]
[25]. Durlach J, Pages N, Bac P, Bara M, Guiet-Bara A, Importance of the ratio between Ionized and total Mg in the serum or plasma:new data on the regulation of Mg status and practical importance of total Mg concentration in the investigation of Mg imbalanceMagnes Res 2002 15:203-05. [Google Scholar]
[26]. WHO, Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity 2011 Geneva (Switzerland)World Health Organisation [Google Scholar]
[27]. Jain MK, Khanuo SK, Chande RD, Jain GC, Bisarya BN, Serum magnesium in pulmonary tuberculosisInd J Tuber 1976 23:177-81. [Google Scholar]
[28]. Oladipo OO, Chukwu CC, Ajala MO, Adewole TA, Afonja OA, Plasma magnesium in adult asthmatics at the Lagos University Teaching Hospital, NigeriaEast Afr Med J 2003 80(9):488-91. [Google Scholar]