Paroxysmal Atrial Fibrillation due to Venomous Snake Bite
Samarth Virmani1, Rama Bhat2, Raghavendra Rao3, Raahat Kapur4, Savio Dsouza5
1 Intern, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Professor, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Assistant Professor, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Intern, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Senior Resident, Department of Medicine, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra Rao, Assistant Professor, Department of Medicine, Kasturba Medical College, Manipal-576104, Karnataka, India.
E-mail: ragsmanipal1983@gmail.com
Snake bites are common all around the world with a great prevalence in South Asia and the Indian subcontinent. Although they are associated with common complications such as local swelling, bleeding at site of bite, coagulopathy, etc., few rare cardiac complications such as myocardial infarctions and arrhythmias have also been described in literature. The following is a case report of a patient who had a snake bite with a Russell’s viper which resulted in atrial fibrillation, which resolved on treatment with anti snake venom.
Arrhythmia, Cardiotoxicity, Viper
Case Report
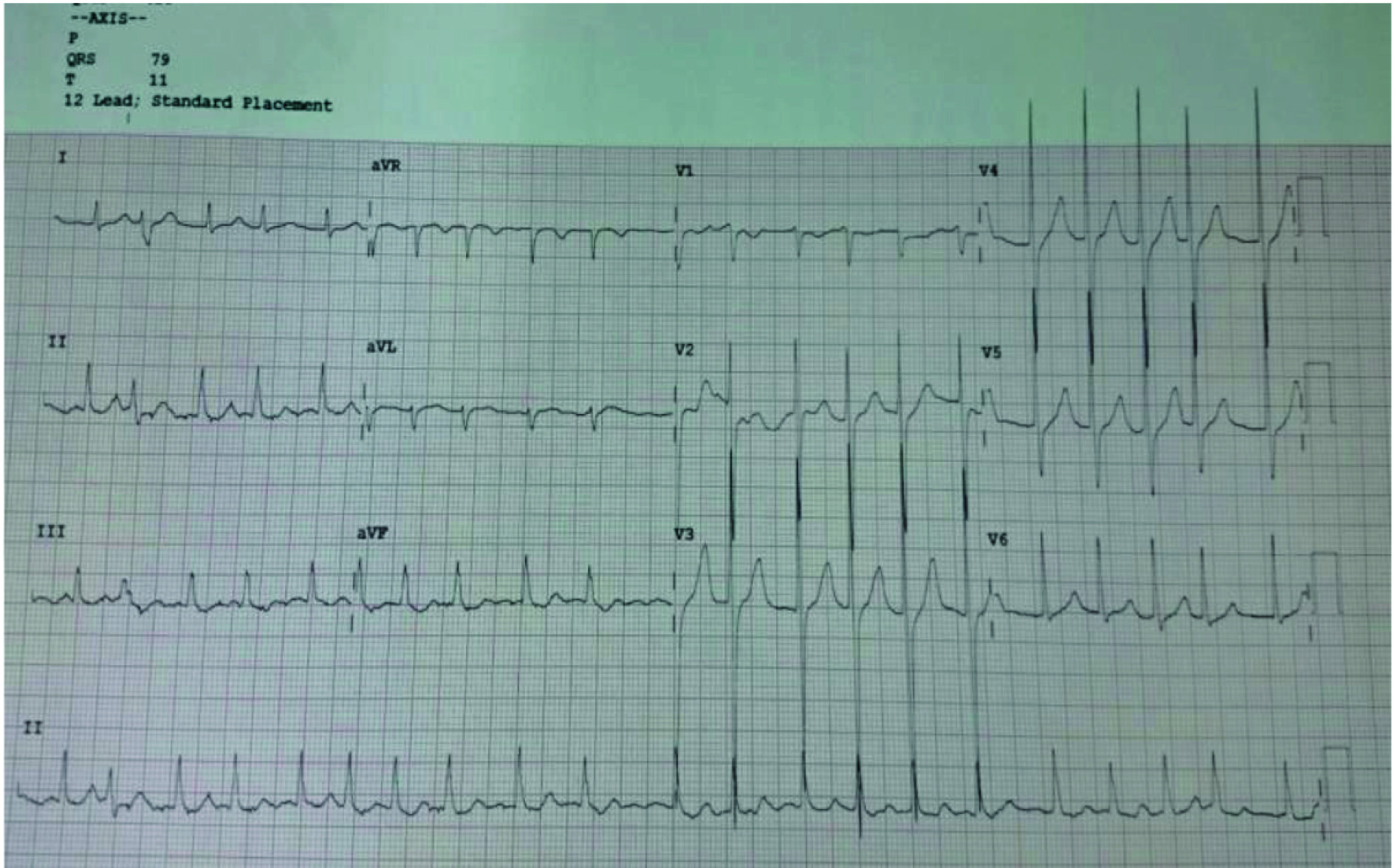
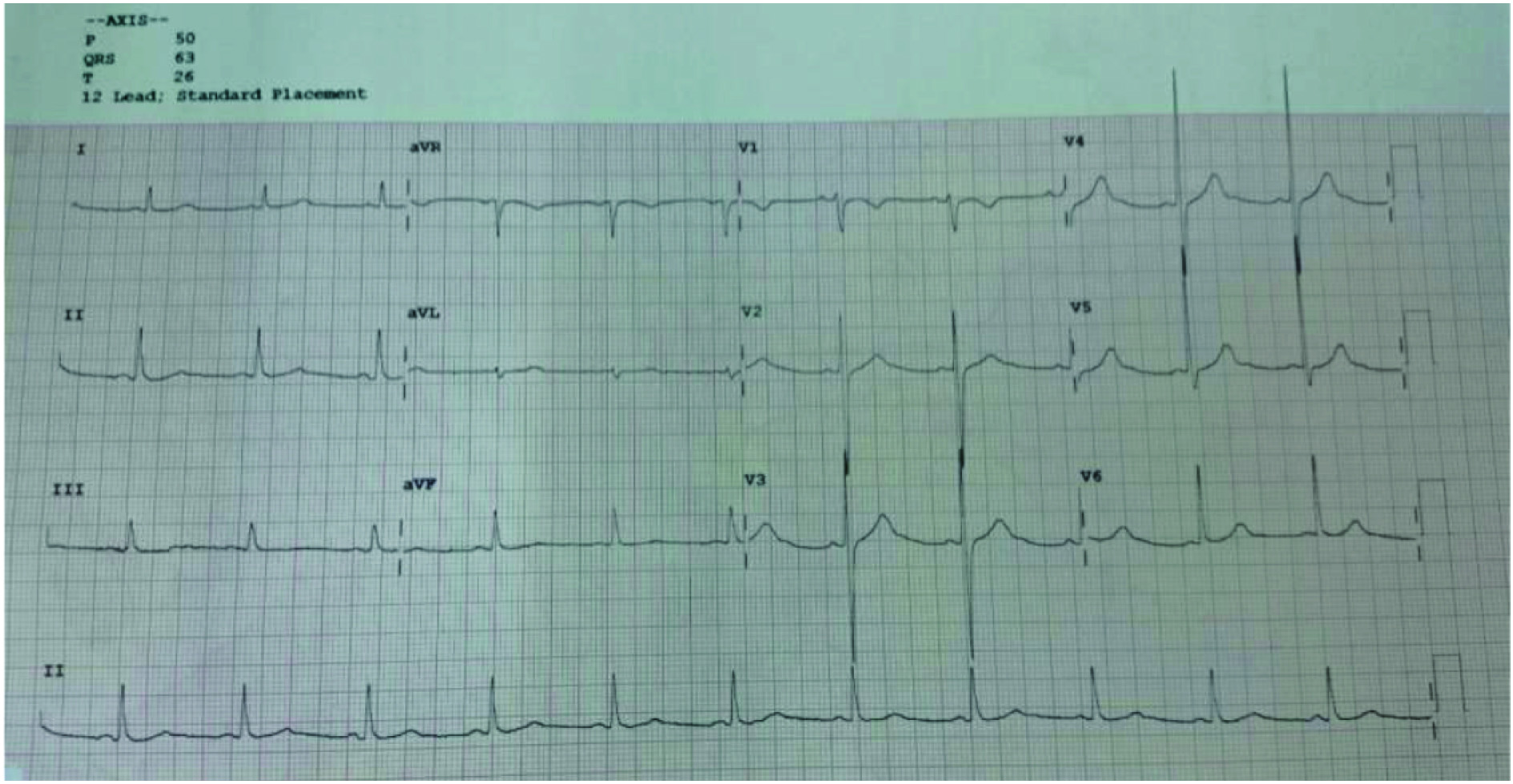
A 60-year-old male, presented to the emergency room with a complaint of alleged snake bite on his left ankle three hours prior to arrival. He also complained of giddiness, diffuse abdominal pain and vomiting, the onset of which was one hour after the bite. There was no history of generalised weakness, diplopia, dysphagia, ptosis, swelling of left limb, bleeding from site of bite, rashes, etc. He had no prior medical history. The snake was killed by the patient’s relatives and brought to the emergency room by them where it was identified to be a Russell’s viper. On examination, his pulse rate was 146 beats/minute, with rhythm being irregularly irregular. All peripheral pulses were palpable. His blood pressure was 100/60 mmHg, his respiratory rate was 18 breaths/minute and oxygen saturation at room air was 98%. There were no rashes on the skin. On systemic examination, no abnormalities were present. On local examination, there was swelling of left lower limb below the level of ankle. Fang marks of the snake bite were seen on the lateral aspect of the left ankle. Blood samples were sent to the laboratory which showed deranged coagulation profile with Prothrombin time (PT) and Activated Partial Thromboplastin Time (APTT) of over 120 seconds each, and low platelet count of 53,000/mm3. Liver function test and renal function tests were normal. Serum electrolytes done were within normal limits. The levels of cardiac enzymes i.e., Creatine Kinase-MB (CKMB) and Troponin T were normal. ECG and ECHO were done in the emergency room. The ECG showed the presence of atrial fibrillation with fast ventricular rate of 126 beats/minute [Table/Fig-1]. The ECHO showed normal biventricular systolic function, tachycardia, no definite wall motion abnormality, no left ventricular hypertrophy and no clot or pericardial effusion. The patient was shifted to the ICU and was given a total of 120 ml (12 vials) of polyvalent anti snake venom along with intravenous ceftriaxone 2 gm once daily for five days. He did not develop anaphylactic reaction to anti snake venom. The patient’s coagulation profile and platelet count improved the next day and was shifted to the wards from ICU. ECG done the next day showed normal sinus rhythm with ventricular rate of 68 beats/minute [Table/Fig-2]. The swelling of the left lower limb also decreased over the next two days and the patient was finally discharged after clinical recovery, normal coagulation profile and normal platelet count. The patient had come for follow up four weeks later. He had no swelling of left lower limb and his complete blood picture was normal.
A 12 lead ECG showing atrial fibrillation with fast ventricular rate.
A 12 lead ECG showing normal sinus rhythm with a rate of 68 beats/minute.
Discussion
Envenomation as a result of snake bites is a globally neglected disease and a major public health problem in South Asia, with an estimated 1.8 to 2.5 million venomous snake bites occurring worldwide each year resulting in at least 1,00,000 to 1,25,000 deaths [1-5].
Some of the common snakes in the Indian subcontinent capable of causing lethal envenomation are the Indian cobra (Naja naja), Common krait (Bungarus caeruleus), Russell’s viper (Daboia russelii) and Saw-scaled viper (Echis carinatus) [6].
Envenomation by bite of Russell’s viper can results in features such as local swelling, local necrosis, coagulopathy, neurotoxicity, nephrotoxicity, cardiac effects and myotoxicity [7]. Rarely, ischemic cardiac events [7], arrhythmias [8] and cardiac tamponade [9] can also occur following bites by Russell’s viper. Russell’s viper venom contains components like factor V and factor X activators, which create high procoagulant potential within the bite victim giving rise to venom induced consumption coagulopathy in humans [10,11].
Cardiac complications such as acute myocardial infarction after snake bite have been reported occasionally, however atrial fibrillation as a result of Russell’s viper bite has been rarely reported.
Sogut O et al., has reported a case of atrial fibrillation with transient ischemic attack in the management of snake bite which was thought to be probably due to subcutaneous epinephrine given for anaphylaxis due to anti venom therapy [12]. Virmani SK has reported a case of atrial fibrillation in an elderly woman with snake bite having no premorbid illnesses. She was treated with xylocaine and anti snake venom. Serial ECG showed reversal to sinus rhythm in 48 hours [13]. Nayak NC et al., reported hypotension, sinus tachycardia, sinus bradycardia, atrioventricular block and acute myocardial infarction as complications following a snake bite [14].
Thillainathan S et al., reported a case of bite by hump nosed viper which resulted in ECG changes suggestive of inferior wall myocardial infarction and atrial fibrillation. The transient ECG changes were thought to be because of coronary arterial spasm causing myocardial infarction [15].
The direct toxic effect of the viper venom may have damaged the myocardium and triggered the cardiac arrhythmia as seen in our patient [16]. It is believed that the electrophysiological properties of the cardiac cell membrane can be modified by the snake venom, which can also have a profound effect on impulse generation and conduction [17]. This cardiac arrhythmia can also be attributed to the adrenergic surge following the bite as a result of psychological fear of death [5].
Conclusion
A patient with a viper bite may have cardiac complications in addition to other anticipated complications. It is of utmost importance for the physician to anticipate the possibility of atrial fibrillation and treat the patient with anti snake venom which may be enough to resolve the fibrillation.
[1]. Alirol E, Sharma SK, Bawaskar HS, Kuch U, Chappuis F, Snake bite in South Asia: a reviewPLoS Negl Trop Dis 2010 4:e603 [Google Scholar]
[2]. Warrell DA, Snake biteLancet 2010 375:77-88. [Google Scholar]
[3]. Rahman R, Faiz MA, Selim S, Rahman B, Basher A, Jones A, Annual incidence of snake bite in rural BangladeshPLoS Negl Trop Dis 2010 4:e860 [Google Scholar]
[4]. Mohapatra B, Warrell DA, Suraweera W, Bhatia P, Dhingra N, Jotkar RM, Snakebite mortality in India: a nationally representative mortality surveyPLoS Negl Trop Dis 2011 5(4):e1018 [Google Scholar]
[5]. Kasturiratne A, Wickremasinghe AR, de Silva N, Gunawardena NK, Pathmeswaran A, Premaratna R, The global burden of snakebite: a literature analysis and modelling based on regional estimates of envenoming and deathsPLoS Med 2008 5:e218 [Google Scholar]
[6]. Simpson ID, Norris RL, Snakes of medical importance in India: is the concept of “Big 4” still relevant and useful?Wilderness Environ Med 2007 18(1):2-9. [Google Scholar]
[7]. Kularatne SAM, Epidemiology and clinical picture of the Russell’s viper (Daboiarusseliirusselii) bite in Anuradhapura, Sri Lanka: a prospective study of 336 patientsSoutheast Asian J Trop Med Public Health 2003 34:855-62. [Google Scholar]
[8]. Thewjitcharoen Y, Poopitaya S, Ventricular tachycardia, a rare manifestation of Russell’s viper bite: case reportJ Med Assoc Thai 2005 88:1931-33. [Google Scholar]
[9]. Senthilkumaran S, Meenakshisundaram R, Thirumalaikolundusubramanian P, Cardiac tamponade in Russell viper (Daboiarusselii) bite: case report with brief reviewJ Emerg Med 2012 42:288-90. [Google Scholar]
[10]. Chippaux JP, Snake venoms and envenomations 2006 FloridaKreiger Publishing Company [Google Scholar]
[11]. Isbister GK, Snakebite doesn’t cause disseminated intravascular coagulation: coagulopathy and thrombotic microangiopathy in snake envenomingSemin Thromb Hemost 2010 36:444-51. [Google Scholar]
[12]. Sogut O, Kaya H, Gokdemir M, Sayhan M, Halis N, Atrial fibrillation and transient ischemic attack encountered in the management of snake biteCardiol Res 2010 1(1):27-28. [Google Scholar]
[13]. Virmani SK, Cardiac involvement in snake biteMed J Armed Forces India 2002 58(2):156-57. [Google Scholar]
[14]. Nayak KC, Jain AK, Sharda DP, Mishra SN, Profile of cardiac complication of snake biteIndian Heart J 1990 42:185-88. [Google Scholar]
[15]. Thillainathan S, Priyangika D, Marasinghe I, Kanapathippillai K, Premawansa G, Rare cardiac sequelae of a hump-nosed viper biteBMC Research Notes 2015 8:437 [Google Scholar]
[16]. Aravanis C, Ioannidis P, Ktenas J, Acute myocardial infarction and cerebrovascular accident in a young girl after a viper biteBr Heart J 1982 47:500-03. [Google Scholar]
[17]. Agarwal A, Kumar T, Ravindranath K, Bhat P, Manjunath C, Agarwal N, Sinus node dysfunction complicating viper biteAsian Cardiovascular and Thoracic Annals 2015 23(2):212-14. [Google Scholar]