Page Kidney in Wunderlich Syndrome Causing Acute Renal Failure and Urosepsis: Successful Timely Minimally Invasive Management of a Devastating Clinical Entity
Sundaramoorthy Vijayganapathy1, Vilvapathy Senguttuvan Karthikeyan2, Ashwin Mallya3, Jayaram Sreenivas4
1 Senior Resident, Deparment of Urology, Institute of Nephro Urology, Bengaluru, Karnataka, India.
2 Senior Resident, Deparment of Urology, Institute of Nephro Urology, Bengaluru, Karnataka, India.
3 Senior Resident, Deparment of Urology, Institute of Nephro Urology, Bengaluru, Karnataka, India.
4 Associate Professor, Deparment of Urology, Institute of Nephro Urology, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vilvapathy Senguttuvan Karthikeyan, Senior Resident, Deparment of Urology, Institute of Nephro Urology, Bengaluru, Karnataka-560002, India.
E-mail: sengkarthik@yahoo.co.in
Wunderlich Syndrome (WS) is an uncommon condition where acute onset of spontaneous bleeding occurs into the subcapsular and perirenal spaces. It can prove fatal if not recognized and treated aggressively at the appropriate time. A 32-year-old male diagnosed elsewhere as acute renal failure presented with tender left loin mass, fever and hypovolemic shock with serum creatinine 8.4 mg/dl. He was started on higher antibiotics and initiated on haemodialysis. Ultrasonogram (USG), Non-Contrast Computed Tomography (NCCT) and Magnetic Resonance Imaging (MRI) showed bilateral perirenal subcapsular haematomas – right 3.6 x 3.1 cm and left 10.3 x 10.3 cm compressing and displacing left kidney, fed by capsular branch of left renal artery on CT angiogram. Initial aspirate was bloody but he persisted to have febrile spikes, renal failure and urosepsis and he was managed conservatively. Repeat NCCT 10 days later revealed left perinephric abscess and Percutaneous Drainage (PCD) was done. Patient improved, serum creatinine stabilized at 2 mg/dl without haemodialysis and PCD was removed after two weeks. To conclude, bilateral idiopathic spontaneous retroperitoneal haemorrhage with renal failure is a rare presentation. This case highlights the need for high index of suspicion, the role of repeated imaging and successful minimally invasive management with timely PCD and supportive care.
Acute kidney injury, Hypertension, Percutaneous drainage, Renin mediated, Spontaneous retroperitoneal haemorrhage
Case Report
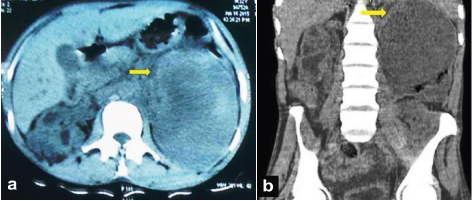
A 32-year-old male, presented with pain in abdomen, distension, breathlessness and anuria for three days. He was diagnosed elsewhere to have Acute Kidney Injury (AKI) and had undergone one session of Haemodialysis (HD) two days before presenting to our institute. He was pale with a pulse rate of 110/min, systolic blood pressure of 90 mm Hg and tachypnea (respiratory rate 30/minute). He had left sided abdominal fullness with a firm mass palpable in the left hypochondrium and lumbar regions. His blood urea 235 mg/ dl, serum creatinine was 8.2 mg/dl and haemoglobin was 6.5 g/dl. He was stabilised haemodynamically and HD was done. Ultrasound (US) showed an enlarged left kidney and a lower pole anechoic collection with septations, 11.4 x 9.9 x 8.6 cm [Table/Fig-1] and diagnostic aspirate was bloody. NCCT of kidneys showed left perinephric collection with compressed kidney [Table/Fig-2].
Ultrasound showing enlarged left kidney with 11.4 x 9.9 cm lower pole anechoic collection.

(a) & (b)]: NCCT KUB showing left perinephric collection with compressed kidney (arrow).
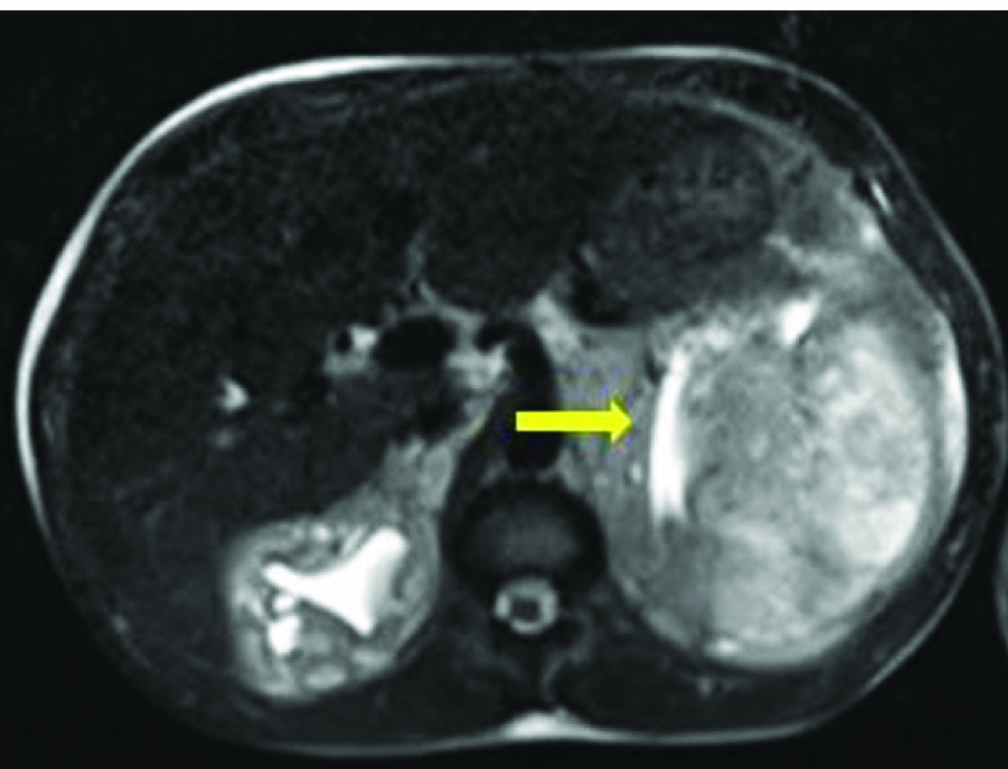
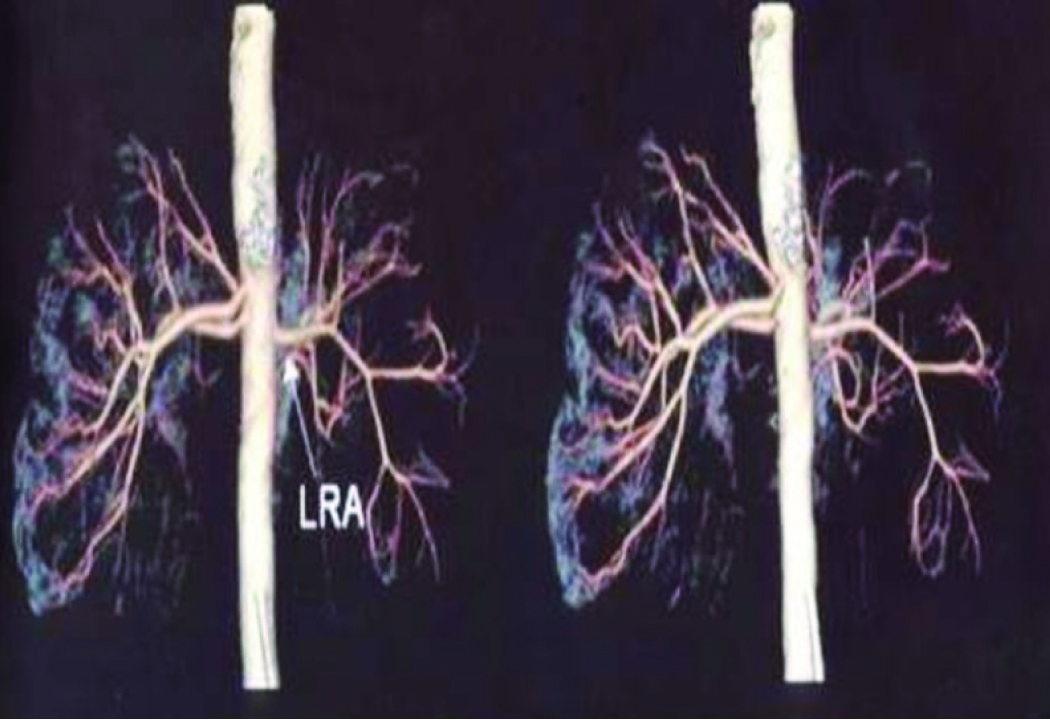
MRI was suggestive of bilateral perirenal haematoma [Table/Fig-3]. After this a CT Angiogram (CTA) was done which revealed left subcapsular haematoma 10.3 x 10.3 cm compressing and displacing the left kidney, fed by capsular branch of the left renal artery [Table/Fig-4]. He also had right perinephric subcapsular haematoma of 3.6 x 3.1 cm. He was managed with three sessions of HD, packed red blood cell transfusions and intravenous antibiotics. As he persisted to have febrile spikes, renal failure and urosepsis, repeat NCCT was done after 10 days which revealed left perinephric abscess. PCD was done with 14F pigtail catheter. Patient improved and his serum creatinine stabilized at 2 mg/dl without haemodialysis. PCD was removed after two weeks and is on regular follow up for six months with stable renal function and his perinephric haematoma have resolved.
MRI suggestive of bilateral perirenal haematoma (arrow showing compressed left kidney).
CT angiogram showed left subcapsular haematoma 10.3 x 10.3 cm compressing and displacing left kidney, fed by capsular branch of left renal artery.
Discussion
WS is an uncommon condition where acute spontaneous bleeding occurs into the subcapsular and perirenal spaces and can be fatal if not diagnosed early and treated aggressively. The commonest cause for WS is neoplasms. Renal Angiomyolipoma (AML) has been reported to be the most common benign renal neoplasm and renal cell carcinoma is the most common malignant neoplasm to cause WS [1]. Other causes of WS include tuberous sclerosis-related renal AML, vasculitis among which Polyarteritis Nodosa (PAN) is the commonest, renal artery aneurysm, arteriovenous malformation, renal vein thrombosis, cystic disease of the kidney, infections of the kidney, renal calculi, nephritis and coagulation disorders [2,3]. Page Kidney (PK) is a condition where the kidney is compressed by a subcapsular or perirenal process causing renal ischemia, inducing unilateral hypersecraetion of renin and contralateral suppression.
Spontaneous renal haematoma was initially reported by Bonet in 1679 and later described by Wunderlich in 1856 [4,5]. Classic presentation is the Lenk’s triad consisting of acute flank pain, tenderness and symptoms of internal bleeding [6] It may mimic acute abdominal conditions like acute appendicitis, perforated viscus or dissecting aorticaneurysm [7]. WS or Spontaneous Retroperitoneal Haemorrhage (SRH) is a relatively uncommon cause of acute abdominal pain [2]. It can occur due to a number of reasons, the commonest being bleeding renal neoplasms, especially renal AML [8]. Symptoms can range from mild to life-threatening [9].
Idiopathic SRH is very rare cause of a surgical acute abdomen and it can be life threatening. The typical initial presentation includes generalized abdominal pain, nausea and anorexia. Hypovolemic shock occurs later in the course of this disease [2]. The management of idiopathic SRH is primarily conservative. Early diagnosis can avert unnecessary exploration in these patients especially when they are haemodynamically unstable. This goes a long way in reducing the morbidity and mortality in this group of patients.
US is extremely valuable for the rapid identification of SRH. Some-times SRH might be misdiagnosed as a renal tumor or abscess [7]. US findings have to be confirmed on a CT scan. CT is 100% sensitive for diagnosis and gives valuable information regarding the aetiology of haematoma. CT has higher sensitivity and specificity than US for identification of an underlying mass. Presence of fat density in the haematoma is a strong pointer towards renal AML. CT also gives valuable information about the contralateral kidney [8]. Our patient did not have fat density or renal tumor on CT. MRI is a useful alternative to CT scan especially in the presence of renal failure [9,10].
It has been shown that angiography is mandatory whenever CT fails to reveal the underlying cause as PAN can be diagnosed only on angiography. The typical findings of PAN on angiography include eccentric or concentric nodules, aneurysms and vessel stenosis or occlusions localized in segmental and interlobular arteries [7,8]. In the past, if radiologic investigations fail to identify the cause of SRH, surgical exploration and biopsy were recommended. In our patient, since the initial presentation was renal failure and urosepsis, he was unfit for surgical exploration. However, he responded to conservative management and later a PCD was done.
Conclusion
Bilateral idiopathic spontaneous retroperitoneal haemorrhage with renal failure is a rare presentation. This case highlights the need for high index of suspicion, the role of repeated imaging and successful minimally invasive management with timely percutaneous drainage and supportive care.
[1]. Wang BH, Pureza V, Wang H, A tale of Wünderlich syndromeJ Surg Case Rep 2012 11:1-3. [Google Scholar]
[2]. Monib S, Ritchie A, Thabet E, Idiopathic retroperitoneal hematomaJ Surg Tech Case Rep 2011 3(1):49-51. [Google Scholar]
[3]. Katabathina VS, Katre R, Prasad SR, Surabhi VR, Shanbhogue AK, Sunnapwar A, Wunderlich syndrome:cross-sectional imaging reviewJ Comput Assist Tomogr 2011 35(4):425-33. [Google Scholar]
[4]. Albi G, del Campo L, Tagarro D, Wünderlich’s syndrome:causes, diagnosis and radiological managementClin Radiol 2002 57(9):840-45. [Google Scholar]
[5]. Daliakopoulos SI, Spontaneous retroperitoneal haematoma:a rare devastating clinical entity of a pleiada of less common originsJ Surg Tech Case Rep 2011 3(1):8-9. [Google Scholar]
[6]. Wolff JM, Jung PK, Adam G, Jakse G, Spontaneous retroperitoneal haemorrhage associated with renal diseaseJ R Coll Surg Edinb 1998 43:53-56. [Google Scholar]
[7]. Baishya RK, Dhawan DR, Sabnis RB, Desai MR, Spontaneous subcapsular renal hematoma:A case report and review of literatureUrol Ann 2011 3(1):44-6. [Google Scholar]
[8]. Brkovic D, Moehring K, Doersam J, Pomer S, Kaelble T, Riedasch G, Aaetiology, diagnosis and management of spontaneous perirenal haematomasEur Urol 1996 29(3):302-07. [Google Scholar]
[9]. Belville JS, Morgentaler A, Loughlin KR, Tumeh SS, Spontaneous perinephric and subcapsular renal haemorrhage:evaluation with CT, US, and angiographyRadiology 1989 172(3):733-38. [Google Scholar]
[10]. Zhang JQ, Fielding JR, Zou KH, Aetiology of spontaneous perirenal haemorrhage:a meta-analysisJ Urol 2002 167(4):1593-96. [Google Scholar]