Aggressive Angiomyxoma in Males
Priyadarshini Dehuri1, Debasis Gochhait2, BH Srinivas3, Sarath Chandra Sistla4
1 Senior Resident, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Pondicherry, India.
2 Assistant Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Pondicherry, India.
3 Associate Professor, Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Pondicherry, India.
4 Professor, Department of Surgery, Jawaharlal Institute of Postgraduate Medical Education and Research, Puducherry, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Debasis Gochhait, Department of Pathology, Institute Block 2nd Floor, JIPMER-605006, Pondicherry, India.
E-mail: Debasis.go@gmail.com
Paratesticular aggressive angiomyxoma is a very rare tumour in males. Most of documented cases of aggressive angiomyxomas have been seen in genital, perineal and pelvic regions in women of child bearing age. We report two cases of aggressive angiomyxomas in males who presented with inguinal swellings. A globular mass with greyish white, glistening cut surface was received after excision of the mass. Microscopic examination revealed a paucicellular tumour comprising of spindle shaped cells along with vessels of varying calibre. The accompanying stroma was myxocollagenous. In addition there was evidence of fat infiltration in one of the cases. Immunohistochemical staining showed CD34, desmin, vimetin positivity and negative staining for S100, actin, Estrogen Receptors (ER) and Progesterone Receptors (PR). The microscopic and immunohistochemical features favoured the diagnosis of aggressive angiomyxoma. This report of angiomyxoma in two cases of males assumes great significance in view of the extreme rarity of the tumour in males and its locally infiltrative nature.
Locally infiltrative, Paratesticular, Paucicellular
Case Report
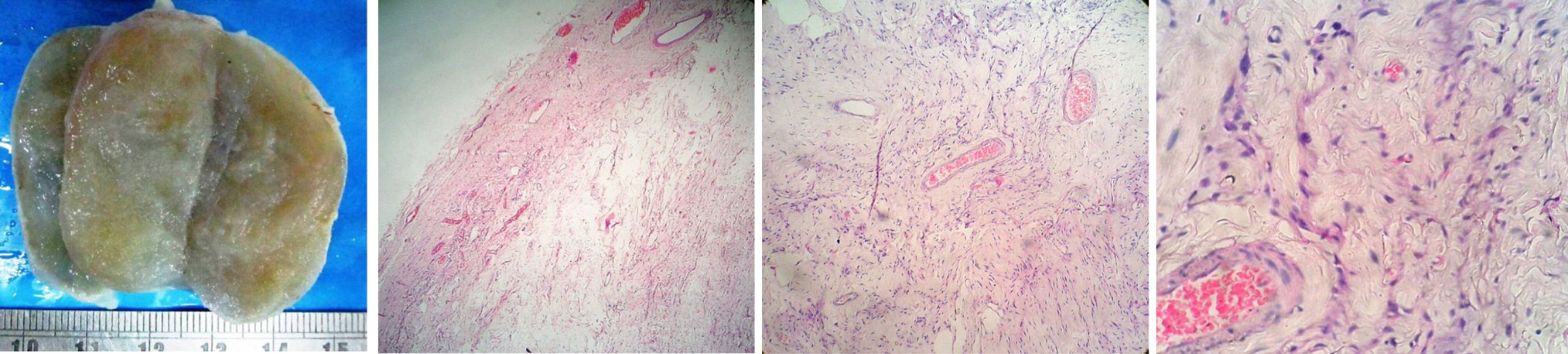
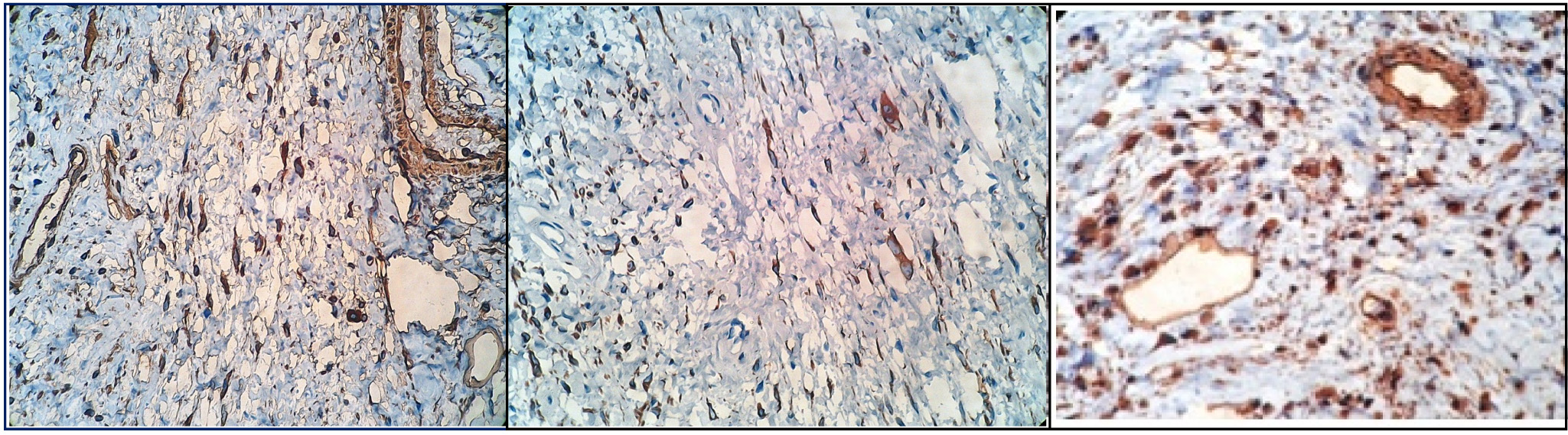
Case 1: A 39-year-old male presented with a slow growing mass in the left inguinal region since six months. It was initially painless and then became painful. Clinically, it suggested an encysted hydrocele of cord. Ultrasonography studies found a hypoechoic lesion and concluded that it was a soft tissue mass, probably of neurogenic lineage. Post excision, we received a greyish white, ovoid, capsulated mass measuring 5 X 3 X 2 cm. The cut surface was greyish white, homogenous and glistening due to myxoid change [Table/Fig-1a]. Microscopic examination revealed an encapsulated tumour. It was a paucicellular lesion with prominence of vessels of varying calibre, both thin and thick walled. It consisted of spindle shaped cells with fine chromatin and indistinct nucleolus in a myxocollagenous stroma [Table/Fig-1b-d]. There was no evidence of any pleomorphism, hyperchromasia, increased mitotic figures or necrosis. Focal extravasation of RBCs was seen. Immunohistochemical studies further showed positive staining of tumour cells for CD34, desmin and vimentin and negative for S100, ER and PR [Table/Fig-2]. The above morphologic and immunohistochemical features lead to a diagnosis of aggressive angiomyxoma of spermatic cord.
(a) Gross appearance showing glistening cut surface; (b) Scanner view showing circumscribed tumour with prominent blood vessels (H&E 4x); (c) Low power view showing hypocellular tumour with blood vessels of varying calibre (H&E 10x). (d) High power view showing spindle shaped cells in myxocollagenous stroma (H&E 40X).
Showing immunohistochemical reactivity of tumour cells for: (a) CD 34; (b) Desmin; (c) Vimentin.
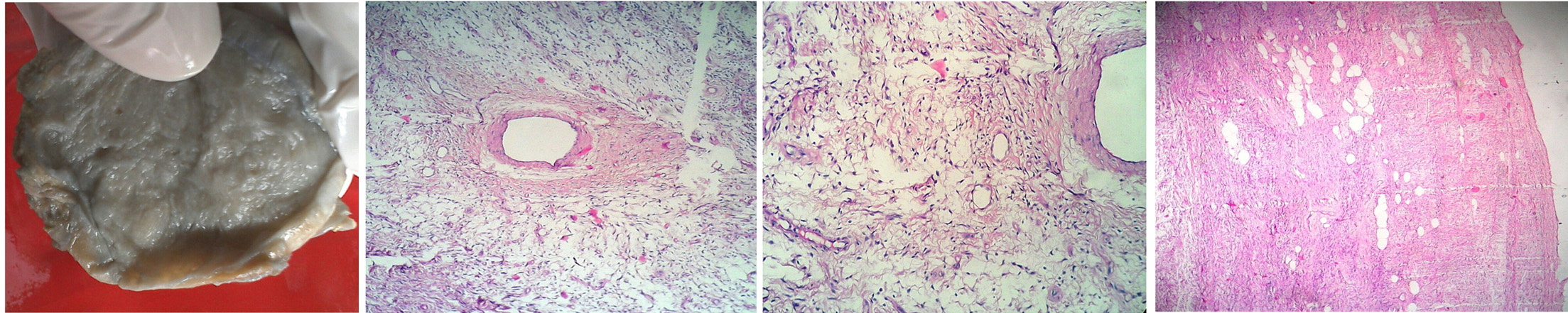
Case 2: A 50-year-old male presented with a firm, non tender swelling in the right inguinal region since four months. There was a clinical and radiological suspicion of a spermatic cord neoplasm. The excision specimen was a Globular, encapsulated mass measuring 7 x 6 x 4 cm. The cross sectional surface was soft, fleshy, predominantly whitish in colour with patchy faint bluish areas [Table/Fig-3a]. Microscopic sections showed an unencapsulated tumour comprising of sparsely populated benign spindle shaped cells in a myxoid background in most of the areas. Fibrofatty areas were also seen. There were numerous randomly distributed blood vessels mostly of small and medium calibre [Table/Fig-3b,c]. Focal hypercellularity was noticed resulting from the condensation of tumour cells around some of the blood vessels. Scattered lymphocytic infiltration was seen in the stroma. In addition, the histologic feature of utmost importance in this case was fat infiltration seen as entrapment of fat cells [Table/Fig-3d]. Immunohistochemical findings were desmin, vimentin and CD 34 positivity and actin, ER and PR negative. The typical histomorphologic features supported by immunohistochemical findings suggested a paratesticular aggressive angiomyxoma as the diagnosis.
(a) Gross image showing myxoid cut surface; (b) Low power view showing thick walled blood vessel and small calibre vessels surrounded by cells in a myxoid stroma (H&E 10X); (c) High power view showing spindle shaped cells in a myxoid stroma (H&E 40X); (d) Scanner view showing fat infiltration (H&E 4X).
As far as our cases are concerned there have been no local recurrences post curative excision in a one and a half year follow up period for the first case and an eight month follow up period for the second case.
Discussion
Since its inception in 1983 by Steeper TA et al., aggressive angiomyomas have been reported mostly in female pelviperineal pathology [1]. There is a clear female predilection for this tumour with a male to female ratio of 1:6 [2]. The sites that are involved in males as suggested in the limited case reports till date are scrotum, spermatic cord, inguinal region, prostate and epididymis [3–7]. Preoperative diagnosis is often a problem because of the rarity of these neoplasms and lack of specific features on imaging studies. Since most cases are diagnosed by histopathological examination after primary surgical excision [8,9], the histomorphologic findings have immense significance.
The proposed origin of this rare tumour is myofibroblastic [10]. The aggressive angiomyxomas need to be differentiated from benign myxoid tumours like intramuscular myxoma, myxoid neurofibroma and myxoid lipoma as well as malignant tumours such as myxofibrosarcoma and myxoliposarcoma. As far as our cases are concerned the other tumours which came into consideration because of similar morphologic features at this site were angiomyofibroblastoma and cellular angiofibroma. Both these entities are well circumscribed lacking any infiltrative behaviour and rather cellular tumours. So paucicellularity of the tumour along with the immunohistochemical staining for CD34, desmin and vimentin favoured the diagnosis of angiomyxoma in our cases [11]. There were subtle morphologic variations in the above two cases of aggressive angiomyxoma. Microscopic fat infiltration was noted in the second case evidenced by entrapment of adipocytes. It was also accompanied by focal areas of hypercellularity.
As far as the hormone receptors reactivity is concerned, these tumours have been mostly reported to be positive in females [7,12,13]. The significance of association with hormone receptors still remains unclear, though some therapeutic advantage using hormone agonists have been proposed. However, the tumour cells did not stain positively for oestrogen and progesterone receptors in both of our cases of male patients.
Aggressive angiomyxoma, unlike its name is not known to carry significant metastatic potential to suggest a malignant tumour. It is rather considered as a benign, locally infiltrative tumour arising from deeper soft tissues. Owing to the significant rate of local recurrence of 20% post excision, wide local excision with careful follow up has been recommended [14]. A yearly follow up has been proposed with the help of imaging modalities as well as clinical supervision [6]. The management guidelines further emphasize the need to differentiate this tumour from other similar benign tumours (like angiomyofibroblastoma) which are adequately treated by local excision only [5].
Conclusion
Aggressive angiomyxomas should be considered in the differential diagnosis of paratesticular tumours presenting as clinically significant masses. This case discussion assumes great significance in view of the extreme rarity of the tumour in males, its typical histologic findings and its adequate management, keeping in mind its locally infiltrative nature. In addition, the recommended management needs to be emphasized and the metastatic potential mandates further research.
[1]. Steeper TA, Rosai J, Aggressive angiomyxoma of the female pelvis and perineum. Report of nine cases of a distinctive type of gynecologic soft-tissue neoplasmAm J Surg Pathol 1983 7:463-75. [Google Scholar]
[2]. Chandra Gupta T, Rani B, Kumari S, Murthy V, Angiomyxoma of genitalia: A case reportIndian J Sex Transm Dis 2007 28:103-05. [Google Scholar]
[3]. Kondo T, Aggressive angiomyxoma in the inguinal region: a case reportJ Med Case Reports [Internet] 2010 4:396 [Google Scholar]
[4]. Idrees MT, Hoch BL, Wang BY, Unger PD, Aggressive angiomyxoma of male genital region. Report of 4 cases with immunohistochemical evaluation including hormone receptor statusAnn Diagn Pathol 2006 10:197-204. [Google Scholar]
[5]. Tsang WY, Chan JK, Lee KC, Fisher C, Fletcher CD, Aggressive angiomyxoma. A report of four cases occurring in menAm J Surg Pathol 1992 16:1059-65. [Google Scholar]
[6]. Rao KSS, Rao KA, Praveen S, Aggressive Angiomyxoma of Scrotum Presenting as Scrotal Lymphedema in a Case of Postoperative Carcinoma PenisIndian J Surg [Internet] 2015 77:170-71. [Google Scholar]
[7]. Morag R, Fridman E, Mor Y, Aggressive angiomyxoma of the scrotum mimicking huge hydrocele: case report and literature reviewCase Rep Med 2009 2009:157624 [Google Scholar]
[8]. Haldar K, Martinek IE, Kehoe S, Aggressive angiomyxoma: a case series and literature reviewEur J Surg Oncol 2010 36:335-39. [Google Scholar]
[9]. Haq RS, Safriadi F, Aggressive Angiomyxoma of the Scrotum: A Case Report and Literature ReviewAmerican Journal of Medical Case Reports [Internet] 2016 4:232-35. [Google Scholar]
[10]. Medina R, Fernando J, Carrera S, Javier A, Ibáñez Heinz O, Martinez CE, Aggressive angiomyxoma in men: Clinical case report and literature reviewRevista Colombiana de Gastroenterologia [Internet] 2011 26:304-10. [Google Scholar]
[11]. Weiss SW, Goldblum JR, Weiss SW, Goldblum JR, Benign Tumors of Smooth muscleEnzinger & Weiss’s soft tissue tumors 2008 5th editionPhiladelphiaMosby:537-42. [Google Scholar]
[12]. Iezzoni JC, Fechner RE, Wong LS, Rosai J, Aggressive angiomyxoma in males. A report of four casesAm J Clin Pathol 1995 104:391-96. [Google Scholar]
[13]. McCluggage W, Patterson A, Maxwell P, Aggressive angiomyxoma of pelvic parts exhibits ooestrogen and progesterone receptor positivityJ Clin Pathol [Internet] 2000 53:603-05. [Google Scholar]
[14]. Khoubehi B, Mishra V, Ali M, Motiwala H, Karim O, Adult paratesticular tumoursBJU International [Internet] 2002 90:707-15. [Google Scholar]