Fabrication and Appraisal of Poly (Lactic-Co-Glycolic Acid) – Moxifloxacin Nanoparticles using Vitamin E-TPGS: A Potential Intracanal Drug Delivery Agent
Hardik Makkar1, Gaurav Patri2
1 Postgraduate student, Department of Conservative Dentistry and Endodontics, Kalinga Institute of Dental Sciences, Bhubaneswar, Odisha, India.
2 Professor, Department of Conservative Dentistry and Endodontics, Kalinga Institute of Dental Sciences, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hardik Makkar, Postgraduate student, Department of Conservative Dentistry and Endodontics, Kalinga Institute of Dental Sciences, Campus 5, KIIT University, Bhubaneswar-751024, Odisha, India.
E-mail: drhardikmakkar@gmail.com
Introduction
Nanotechnology is gaining momentum in the search for ideal biomaterials by dental researchers. The expansible nature of Endodontology deems exploration, learning and scrutinizing newer avenues which have the potential to be applied and investigated. The popularity of polymers as drug delivery vehicles has opened avenues for their application in the root canal system. This study utilized application of biodegradable polymers as potential drug delivery vehicles against Enterococcus faecalis, one of the main reasons for post treatment disease.
Aim
This study aimed at fabricating Poly (Lactic-co-Glycolic Acid) (PLGA)-moxifloxacin nanoparticles and assessing its sustained antimicrobial efficacy with calcium hydroxide and chitosan-moxifloxacin hydrogel against Enterococcus faecalis.
Materials and Methods
PLGA (50:50) in a quantity of 100 mg was dissolved in 1 ml ethyl acetate and 45 ml of 0.3% w/v Vitamin-E Polyethylene Glycol 1000 Succinate (vitamin E-TPGS) was kept for magnetic stirring in separate beaker. Moxifloxacin (50 μl) was added to polymer PLGA following which vitamin E-TPGS was added to the polymer. Nanoparticles were fabricated using ultrasonication and collected by centrifugation. Surface characterization was assessed using scanning electron microscope. Results were obtained in the form of zone of inhibition by the nanoparticles against Enterococcus faecalis and comparisons were made with chitosan-moxifloxacin hydrogel and calcium hydroxide using Analysis of Variance (ANOVA) followed by Student t-test.
Results
Upon statistical analysis, the zone of inhibition against E. faecalis remained constant with PLGA-moxifloxacin nanoparticles for 14 days while it decreased with chitosan-moxifloxacin hydrogel and remained nil for calcium hydroxide (p<0.01).
Conclusion
The study posits that PLGA encapsulated moxifloxacin nanoparticles showcased sustained antibacterial effect in low doses against the test pathogen. Its sustained and programmed release makes them unique contenders for further evaluation in Endodontics as potential intracanal medicaments.
Biodegradable polymers, E. faecalis, Intracanal medicament
Introduction
Complete debridement of the root canal system is unachievable even when root canal therapy is performed to the highest technical standards due to the complexity of the root canal system incorporating isthmuses, ramifications and dentinal tubules [1].
Although obligate anaerobes predominate primary endodontic infections, gram positive facultative anaerobes are associated with non surgical endodontic treatment failures in high proportion [2,3]. Enterococcus faecalis has garnered continued interest due to its persistence and survival in post-treatment disease. With its vast spectrum of virulence factors and its relationship to endodontic disease [4], enterococcal bacterial efflux system is posing a great threat and is of interest to counter emergence of multidrug resistant strains.
Emergence of nanotechnology and popularity of polymers as drug delivery vehicles have opened avenues for their application in the root canal system. The advantage of polymers being used as encapsulating agents for drug delivery lies behind their property to protect the drug from early degradation, thereby rendering longer biological half life and potentiated efficacy [5-7].
Recent years have witnessed various drug delivery systems among which PLGA has gained enormous attention. As a copolymer of lactic and glycolic acid, it has exquisite properties like biocompatibility, biodegradability and allowing sustained and controlled release of encapsulated agent [8]. Numerous intracanal medicaments used in endodontic practice have phased out due to controversial formulations, inadvertent usage, ill defined dosages, early degradation and inactivation and most important, occurrence of resistance. Development of effective and novel strategies against root canal pathogens thus is imperative.
Hence, the aim of this study was to fabricate PLGA-moxifloxacin nanoparticles using vitamin E-TPGS and to assess its antimicrobial efficacy against Enterococcus faecalis. A comparative evaluation of this formulation was done with calcium hydroxide and chitosan -moxifloxacin hydrogel on culture plates. The hypothesis formulated was that PLGA-moxifloxacin nanoparticles will have sustained drug release and antimicrobial activity against E. faecalis as compared to chitosan moxifloxacin hydrogel and calcium hydroxide.
Materials and Methods
The present in vitro study was conducted between March 2016 to September 2016 at Kalinga Institute of Dental Sciences and School of Biotechnology, KIIT University, Bhubaneswar, India.
1. Preparation of Formulations for Testing Antibacterial Efficacy
Fabrication of PLGA-moxifloxacin nanoparticles using vitamin E-TPGS as emulsifying agent (Formulation 1) [Table/Fig-1]:(a-i): Methodology for fabrication of PLGA-moxifloxacin nanoparticles
a: Overnight dissolution of polymer (PLGA) in ethyl acetate;
b: Stock solution of Vitamin E-TPGS under magnetic stirring;
c: Moxifloxacin- PLGA solution ultrasonicated and homogenized to obtain encapsulate;
d: Antibiotic polymer solution added to vitamin E-TPGS and vortexed to form emulsion;
e: Emulsion ultrasonicated;
f; Nanoparticle emulsion transferred to vitamin E-TPGS stock and magnetically stirred;
g,h: Centrifugation of emulsion and collection of nanoparticles;
i: PLGA-Moxifloxacin nanoparticles as observed under scanning electron microscopy.
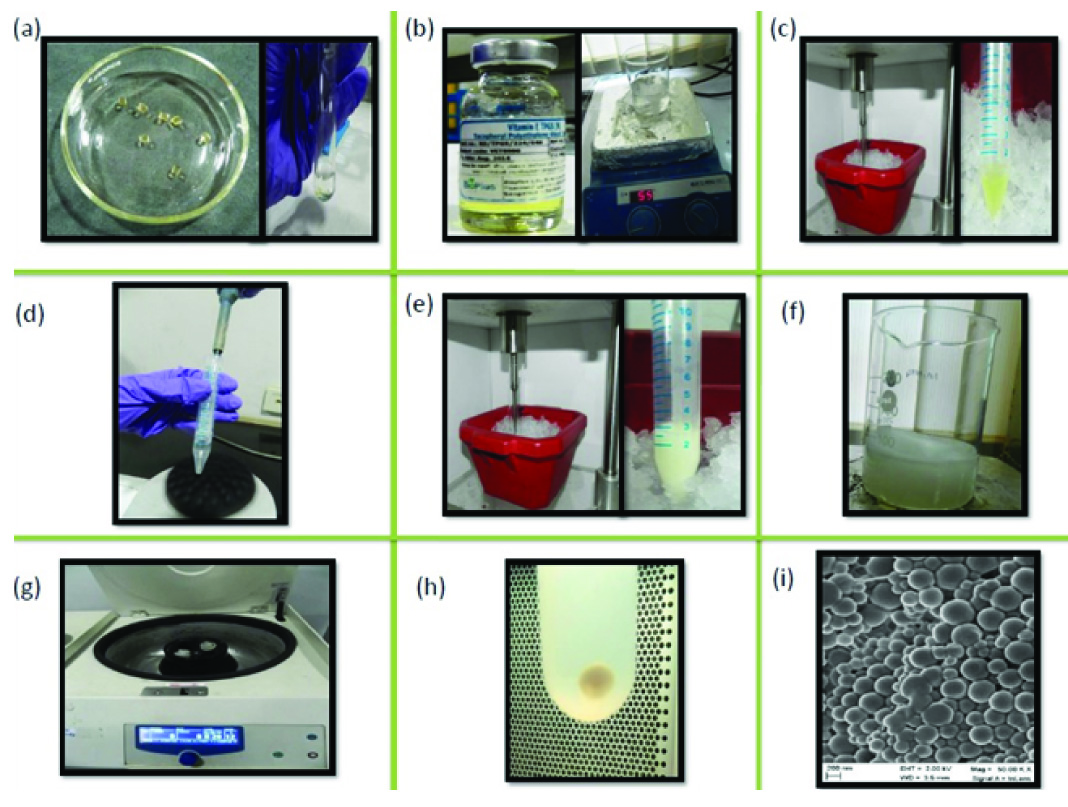
Fabrication of nanoparticles was done as previously reported (9) with modifications. PLGA (50:50) (B6010-2 Durect corporation, AL) in a quantity of 100 mg was dissolved overnight in 1 ml of ethyl acetate (Sigma Chemical Co., St Louis, MO, USA).
Vitamin E-TPGS (0.3% w/v, 45 ml) (BioPlus Life Sciences, India) was magnetically stirred at 360 rpm and 2 ml transferred in a separate test tube.
Moxifloxacin HCl (4 g/dl, 50 μl) (Sigma Chemical Co., St Louis, MO, USA) was added to PLGA polymer solution and ultrasonicated to obtain a homogenous solution. The test tube containing 2 ml vitamin E-TPGS was kept vertically on a high vortex and polymer encapsulant solution was added to this drop wise till emulsion was formed which then was transferred to the ultrasonicater (Qsonica, Newtown, CT). Keeping the test tube immersed in ice water, the emulsion was sonicated in three 10 second bursts (40% amplitude) with a pause between each burst to allow the solution to cool. The emulsion was transferred in the beaker containing vitamin E-TPGS and kept for magnetic stirring for three hours to facilitate solvent evaporation.
The emulsion was centrifuged for 20 minutes at 14000 rpm following which the supernatant was discarded. The nanoparticle pellet was finally resuspended in distilled water to a final volume of 10 ml. A 5 ml of nanoparticle emulsion was transferred in a centrifuge tube and kept at -80°C and lyophilized. The surface morphology of nanoparticles was visualized using field emission scanning electron microscope (Shimadzu, Japan).
Preparation of Chitosan-Moxifloxacin Hydrochloride Hydrogel (Formulation 2):
The Hydrogel was prepared by mixing 100 mg chitosan (75– 85% deacetylated, Sigma-Aldrich) with 50 μl moxifloxacin HCl (4 g/dl) at room temperature. The pH was adjusted to 6.5 using 1M NaOH, and the preparation was magnetically stirred overnight. The hydrogel was then transferred to a sterile container and stored at 4°C.
Preparation of Calcium Hydroxide Solution (Formulation 3):
A saturated solution of calcium hydroxide was prepared by dissolving 400 mg calcium hydroxide powder (Sigma Chemical Co., St Louis, MO, USA) in 10 ml distilled water. The saturated solution was centrifuged (3000 × g, 10 minute); the supernatant was removed resulting in a stock calcium hydroxide solution, pH 11.5.
2. Antibacterial Testing of Three Formulations Against Enterococcus Faecalis (ATCC®29212™)
Precultured E. faecalis on bile esculin agar was streaked on freshly prepared plates containing Luria Bertini agar (Himedia Laboratories, Mumbai). A 10 μl of each formulation was dropped in culture plates with test organism under a laminar flow and area of inhibition of bacterial growth were calculated at 24 hour interval for 14 days in an incubator under static conditions. The sample for each formulation across each time zone was 10, making a total sample of 140 for each formulation [Table/Fig-2]. All the samples were photographed and the area of inhibition (area devoid of bacterial growth) was calculated using Adobe Photoshop CS4 (adobe systems, CA).
Experimental design and result criteria.
| Group | PLGA-Moxifloxacin Nanoparticles | Chitosan-Moxifloxacin Hydrogel | Calcium Hydroxide |
|---|
| Sample Culture plates (A) Number of time zone (B) | 10 14 | 10 14 | 10 14 |
| Total sample size (A * B) | 140 | 140 | 140 |
| Quantity of drug loading on plates | 10 μl | 10 μl | 10 μl |
| Test organisms | Enterococcus faecalis (ATCC®29212™) | Enterococcus faecalis (ATCC®29212™) | Enterococcus faecalis (ATCC®29212™) |
| Result criteria | Area of the zone of inhibition | Area of the zone of inhibition | Area of the zone of inhibition |
| Area of inhibition was calculated at 24 hours interval for 14 days keeping culture plates in incubator under static condition. |
Statistical Analysis
The data obtained was statistically analysed using software Statistical Package for Social Sciences (SPSS) version 17.0. The data was subjected to Analysis of Variance followed by Student t-test with level of significance set at p<0.01.
Results
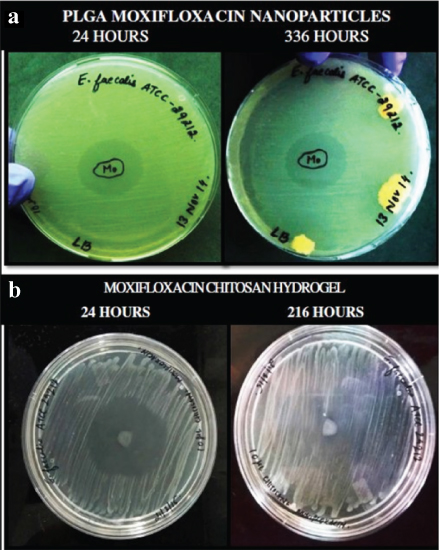
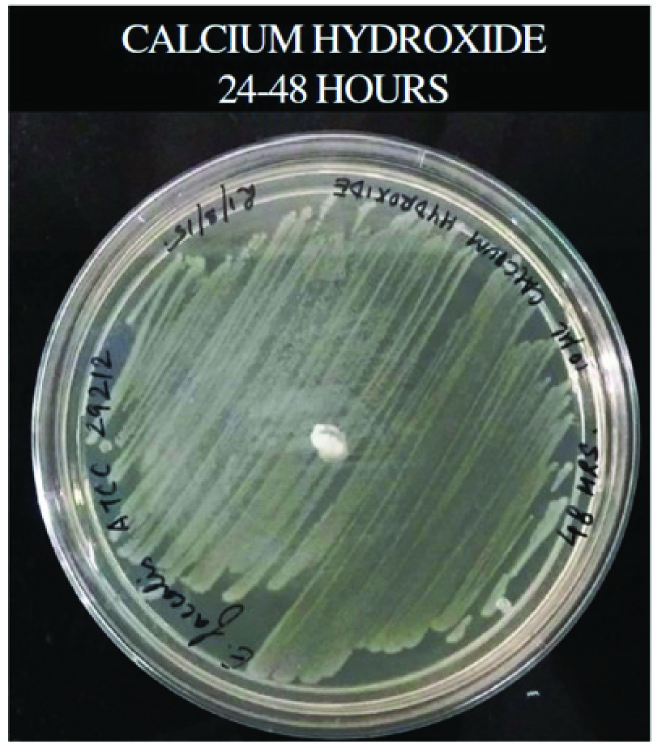
The area of inhibition of the three drug formulations can be seen in [Table/Fig-3]. The mean area of inhibition of PLGA-moxifloxacin nanoparticles was constant from 24 hours to 336 hours at 1178.938 mm2 [Table/Fig-3,4a]. On the contrary, for chitosan-moxifloxacin hydrogel, the mean area of inhibition (1569.491 mm2) at 24 hours was more which displayed reduction with progressive increase in time, dropping to zero at 216 hours [Table/Fig-3,4b]. Calcium hydroxide completely failed to inhibit the test organism with a mean area of inhibition at 0 [Table/Fig-5].
Area of inhibition across time intervals of the drug formulations.
| Time | N (Sample Size) | PLGA-Moxifloxacin Nanoparticles | Chitosan Moxifloxacin Hydrogel | Calcium Hydroxide |
|---|
| Mean (mm2) | SD | Mean (mm2) | SD | Mean (mm2) | SD |
|---|
| 24 | 10 | 1178.938 | 16.9137 | 1569.491 | 48.5463 | 0 | 0 |
| 48 | 10 | 1178.938 | 16.9137 | 1292.144 | 213.1269 | 0 | 0 |
| 72 | 10 | 1178.938 | 16.9137 | 1062.166 | 221.544 | 0 | 0 |
| 96 | 10 | 1178.938 | 16.9137 | 723.21 | 334.2526 | 0 | 0 |
| 120 | 10 | 1178.938 | 16.9137 | 424.859 | 284.6812 | 0 | 0 |
| 144 | 10 | 1178.938 | 16.9137 | 213.395 | 215.6036 | 0 | 0 |
| 168 | 10 | 1178.938 | 16.9137 | 76.156 | 118.4808 | 0 | 0 |
| 192 | 10 | 1178.938 | 16.9137 | 3.5 | 11.068 | 0 | 0 |
| 216 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| 240 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| 264 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| 288 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| 312 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| 336 | 10 | 1178.938 | 16.9137 | 0 | 0 | 0 | 0 |
| Total | 140 | 1178.938 | 16.1033 | 383.209 | 554.6005 | 0 | 0 |
Culture plates showing zone of inhibition a) by PLGA-moxifloxacin nanoparticles against E. faecalis (ATCC®29212™) from 24 hours to 336 hours and b) chitosan moxifloxacin hydrogel from 24 hours to 226 hours.
Culture plates showing no inhibition by Calcium hydroxide against E. faecalis.
The statistical analysis conducted to establish the effectiveness of sustained antimicrobial drug release from three drug formulations namely PLGA-moxifloxacin nanoparticles, chitosan-moxifloxacin hydrogel and calcium hydroxide revealed highly significant results. The result from two-way ANOVA indicated a highly significant F value of 407.306 (p<0.001) [Table/Fig-6]. The descriptive statistics [Table/Fig-3] reveals that calcium hydroxide group had a mean of zero (no zone of inhibition) since the beginning. Thus, a t-test was used to investigate the difference between PLGA-moxifloxacin nanoparticles and chitosan-moxifloxacin hydrogel, which also revealed significant results with a t-value of 16.969 (p<0.001) [Table/Fig-6].
Comparison of means (area of inhibition) of the three drug formulations using ANOVA and student t-test.
| Drug formulation | N (Sample Size) | Mean | Std. Deviation | F value (ANOVA) | t-test |
|---|
| PLGA-Moxifloxacin Nanoparticles | 140 | 1178.938 | 16.1033 | 407.306 (Sig. 0.00) | 16. 969 (Sig. 0.00) |
| Chitosan Moxifloxacin Hydrogel | 140 | 383.209 | 554.6005 |
| Calcium Hydroxide | 140 | 0 | 0 |
Discussion
Advancement in nanotechnology has allowed researchers to generate various therapeutics and delivery vehicles. Endodontic researchers have imbibed and adopted such advancements for its utilization and application in our clinical scenario. In this study, PLGA-moxifloxacin nanoparticles were fabricated and tested for the first time as potential intracanal medicament. Moxifloxacin, a flouroquinolone was chosen as the antibiotic to be encapsulated and evaluated for the first time along with polymer as a potential intracanal medicament because of its broad spectrum activity and added anaerobic coverage, intranuclear inhibition of DNA gyrase and postantibiotic effect [9]. This study utilized vitamin E-TPGS as an emulsifying agent so as to deal with the problem of multidrug resistance and to improve encapsulation and emulsification efficiency as shown previously [10].
Enterococcus faecalis has been the phoenix of the root canal, and for more than a decade this microorganism has gained much attention. Literature is replete eliciting this gram positive’s role in nosocomial infection and one of the etiological agent for emergence of multidrug resistance [11,12].
With an ability to form monospecies biofilm in vitro [13], this notorious organism utilizes enterococcal surface protein (Esp) [14], gelatinase (GelE), transcriptional regulator BopD and quorum sensing locus fsr to induce biofilm formation [15].
Presence of transmembrane efflux pumps on cell wall of E. faecalis is another mode of antimicrobial resistance which has been less focused upon. Efflux is a process by which bacteria transports toxic compounds outside the cell [16]. Using bioinformatics, thirty four potential multidrug resistance encoding genes have been reported in E. faecalis [17].
In this study, PLGA encapsulated moxifloxacin nanoparticles were effective in inhibition of Enterococcus faecalis for a period of 14 days (constant zone of inhibition) which shows how effectively sustained release of moxifloxacin from its polymer encapsulation delivered such a result [Table/Fig-4a]. With chitosan-moxifloxacin hydrogel group, a larger area of inhibition was seen in all the samples initially, which can be attributed to higher quantity of antibiotic release from the mesh of hydrogel. It is noteworthy that all the samples in this group had gradual reduction in inhibition zones with complete growth in 192 hours which shows initial high release of antibiotic followed by its early degradation. An explanation for the above mentioned result was due to different methods of drug binding and that drug encapsulation was a better method for sustained and effective release than hydrogel which had early release and degradation of the antibiotic as inferred from the results.
Calcium hydroxide on the contrary, completely failed to inhibit the test organism in all the samples. This can be supported by previous study which highlighted the presence of a proton pump driven resistance to calcium hydroxide in E. faecalis [18] which was further reiterated by a study showing EmeA gene mediated efflux of diverse compounds through a proton-motive force in E. faecalis [19].
Calcium hydroxide was thus chosen as a control in this study to compare how addition of a p-glycoprotein inhibitor (vitamin E-TPGS) to moxifloxacin will counter efflux mediated resistance in the form of constant zone of inhibition.
The intention of fabricating nanoparticles was to create a formulation which has antimicrobial properties through receptor blockade mechanism. Vitamin E-TPGS inhibiting the transmembranous efflux pump will allow antibiotic to easily penetrate the cell membrane and cause lysis without incurring resistance. The nanoparticles have an advantage due to their size as they have the potential to easily penetrate intricate structures inside the root canal including dentinal tubules, isthumi and anatomic locations where instrumentation is not feasible [20].
Utilizing PLGA for encapsulation has a plethora of ideal properties of a drug delivery agent including inertness, biodegradability [21,22] and smart release of the drug [23] as erosion of these particles with simultaneous drug release will take place only in change with pH, temperature, fluids (exudates/transudate) which are most commonly seen in inflammatory challenges. The nanoparticles formed were lyophilized which showcases their effective storage capabilities and enhanced shelf life [24].
Moxifloxacin has been previously shown to be highly active against E. faecalis isolated from filled root canals with periapical lesions [25]. This result has been reiterated by other authors including against periodontal pathogens and bacteria isolated from dentoalveolar abscesses [26-28].
Chitosan as a drug carrier has been previously evaluated in combination with triple antibiotic paste and calcium hydroxide against E. faecalis, showing better antibacterial effects compared to the combination of these medicaments with saline [29]. The present study merits polymer encapsulated moxifloxacin as compared to chitosan moxifloxacin hydrogel against E. faecalis.
The novelty of this study lies behind the antibiotic concentration used for fabrication of these nanoparticles. The results obtained in this group were with 0.002 mg of antibiotic loading as compared to extremely high doses used systemically. It would also be noteworthy to compare the dose and effect of this single antibiotic agent with locally applied triple antibiotic pastes in the root canal. This study thus demonstrated a model through which effective antimicrobial effect can be achieved by sustained release of drug without incurrence of resistance as determined qualitatively from the results (constant zone of inhibition).
Limitation
This study however illustrated preliminary assessment of these nanoparticles against test organism on culture plates. Agar diffusion assay was chosen as the first means to assess the properties of these nanoparticles in the form of sustained zones of inhibition for 14 days (qualitatively) and measurement of these zones for quantitative analysis.
Further vitro/vivo studies are required for evaluation and comparison of these nanoparticles with treatment options available for recurrent root canal infections.
Conclusion
In conclusion, PLGA encapsulated moxifloxacin nanoparticles were more effective than other formulations due to their effective and sustained antibiotic release with significant result. Its programmed release makes them unique contenders for further evaluation in vitro and vivo models as potential intracanal medicaments.
This study opens future avenues for the application of polymer encapsulated antibiotics with importance to Moxifloxacin, and its potential role in eliminating diverse and pathogenic endodontic microflora without incurring resistance.
[1]. Siqueira JF, Araújo MC, Garcia PF, Fraga RC, Dantas CJS, Histological evaluation of the effectiveness of five instrumentation techniques for cleaning the apical third of root canalsJ Endod 1997 23(8):499-502. [Google Scholar]
[2]. Rolph H, Lennon A, Riggio M, Saunders W, MacKenzie D, Coldero L, Molecular identification of microorganisms from endodontic infectionsJ Clin Microbiology 2001 39(9):3282-89. [Google Scholar]
[3]. Siqueirajr J, Rocas I, Nested PCR detection of centipeda periodontii in primary endodontic infectionsJ Endod 2004 30(3):135-37. [Google Scholar]
[4]. Kayaoglu G, Orstavik D, Virulence factors of enterococcus faecalis: relationship to endodontic diseaseCrit Rev Oral Biol Med 2004 15(5):308-20. [Google Scholar]
[5]. Haag R, Kratz F, Polymer therapeutics: concepts and applicationsChem Inform 2006 37:20 [Google Scholar]
[6]. Tong R, Cheng J, Anticancer polymeric nanomedicinesPolymer Reviews 2007 47(3):345-81. [Google Scholar]
[7]. Kumari A, Yadav S, Yadav S, Biodegradable polymeric nanoparticles based drug delivery systemsColloids and Surfaces B: Biointerfaces 2010 75(1):01-18. [Google Scholar]
[8]. Langer R, Drug delivery and targetingNature 1998 392(6679 Suppl):05-10. [Google Scholar]
[9]. Katzung BG, Masters SB, Trevor AJ, Basic and clinical pharmacology 2011 New YorkMcGraw Hill Medical [Google Scholar]
[10]. McCall R, Sirianni R, PLGA nanoparticles formed by single- or double-emulsion with vitamin E-TPGSJ Vis Exp 2013 82:e51015 [Google Scholar]
[11]. Fernandez-Guerrero M, Herrero L, Bellver M, Gadea I, Roblas R, De Gorgolas M, Nosocomial enterococcal endocarditis: a serious hazard for hospitalized patients with enterococcalbacteraemiaJ Intern Med 2002 252(6):510-15. [Google Scholar]
[12]. Huycke M, Multiple-drug resistant Enterococci: the nature of the problem and an agenda for the futureEmerg Infect Dis 1998 4(2):239-49. [Google Scholar]
[13]. Toledo-Arana A, Valle J, Solano C, Arrizubieta M, Cucarella C, Lamata M, The enterococcal surface protein, esp, is involved in enterococcus faecalis biofilm formationAppl Environ Microbiol 2001 67(10):4538-45. [Google Scholar]
[14]. Tendolkar P, Baghdayan A, Gilmore M, Shankar N, Enterococcal surface protein, esp, enhances biofilm formation by enterococcus faecalisInfect. Immun 2004 72(10):6032-39. [Google Scholar]
[15]. Kishen A, Upadya M, Tegos G, Hamblin M, Efflux pump inhibitor potentiates antimicrobial photodynamic inactivation of enterococcus faecalis biofilmPhotochem. Photobiol 2010 86(6):1343-49. [Google Scholar]
[16]. Upadya M, Shrestha A, Kishen A, Role of efflux pump inhibitors on the antibiofilm efficacy of calcium hydroxide, chitosan nanoparticles, and light-activated disinfectionJ Endod 2011 37(10):1422-26. [Google Scholar]
[17]. Lee E, Huda M, Kuroda T, Mizushima T, Tsuchiya T, EfrAB, an ABC multidrug efflux pump in enterococcus faecalisAntimicrob. Agents Chemother 2003 47(12):3733-38. [Google Scholar]
[18]. Evans M, Davies J, Sundqvist G, Figdor D, Mechanisms involved in the resistance of Enterococcus faecalis to calcium hydroxideInt Endod J 2002 35(3):221-28. [Google Scholar]
[19]. Lee E, Chen J, Huda M, Kuroda T, Mizushima T, Tsuchiya T, Functional cloning and expression of emea, and characterization of emea, a multidrug efflux pump from Enterococcus faecalisBiol Pharm Bull 2003 26(2):266-70. [Google Scholar]
[20]. Chou L, Ming K, Chan W, Strategies for the intracellular delivery of nanoparticlesChem Soc Rev 2011 40(1):233-45. [Google Scholar]
[21]. Pagonis T, Chen J, Fontana C, Devalapally H, Ruggiero K, Song X, Nanoparticle-based Endodontic Antimicrobial Photodynamic TherapyJ Endod 2010 36(2):322-28. [Google Scholar]
[22]. Jaberi-Ansari Z, Ekrami M, Nojehdehian H, Controlled release of drugs for management of pulpitisAvicenna J Dent Res 2013 6(1):e21610 [Google Scholar]
[23]. Zolnik B, Burgess D, Effect of acidic pH on PLGA microsphere degradation and releaseJ Control Release 2007 122(3):338-44. [Google Scholar]
[24]. Abdelwahed W, Degobert G, Stainmesse S, Fessi H, Freeze-drying of nanoparticles: Formulation, process and storage considerationsAdv. Drug Deliv. Rev 2006 58(15):1688-713. [Google Scholar]
[25]. Pinheiro ET, Gomes BP, Drucker DB, Zaia AA, Ferraz CC, Souza-Filho FJ, Antimicrobial susceptibility of Enterococcus faecalis isolated from canals of root filled teeth with periapical lesionsInt Endod J 2004 37(11):756-63. [Google Scholar]
[26]. Speciale A, Musumeci R, Blandino G, Milazzo I, Caccamo F, Nicoletti G, Minimal inhibitory concentrations and time-kill determination of moxifloxacin against aerobic and anaerobic isolatesInt J Antimicrob Agents 2002 19(2):111-18. [Google Scholar]
[27]. Milazzo I, Blandino G, Musumeci R, Nicoletti G, Bue AL, Speciale A, Antibacterial activity of moxifloxacin against periodontal anaerobic pathogens involved in systemic infectionsInt J Antimicrob Agents 2002 20(6):451-56. [Google Scholar]
[28]. Sobottka I, Cachovan G, Stürenburg E, Ahlers MO, Laufs R, Platzer U, In vitro activity of moxifloxacin against bacteria isolated from odontogenic abscessesAntimicrob Agents Chemother 2002 46(12):4019-21. [Google Scholar]
[29]. Shaik J, Garlapati R, Nagesh B, Sujana V, Jayaprakash T, Naidu S, Comparative evaluation of antimicrobial efficacy of triple antibiotic paste and calcium hydroxide using chitosan as carrier against Candida albicans and Enterococcus faecalis: An in vitro studyJ Conserv Dent 2014 17(4):335 [Google Scholar]