Parietal Wall Abscess Perforating to Transverse Colon: A Rare Presentation
Sudeepta Kumar Swain1, Dinesh Zirpe2, Somak Das3, Tirupporur Govindaswamy Balachandar4, Prasanna Kumar Reddy5
1 Consultant, Department of Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
2 Registrar, Department of Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
3 Senior registrar, Department of Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
4 Consultant, Department of Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
5 Consultant, Department of Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sudeepta Kumar Swain, Consultant, Department of Surgical Gastroenterology, Apollo Hospital, A1, Peach Block, Appasamy Orchards, Arcot Road, Vadapalani, Chennai-600026, Tamil Nadu, India.
E-mail: sudeepdadu@gmail.com
Extrapulmonary tuberculosis affects an isolated organ or presents secondary to pulmonary involvement. Lymph nodes are the common sites for extrapulmonary tuberculosis. Primary extrapulmonary tuberculosis involving parietal wall is an unusual presentation. Tubercular abscess of the abdominal wall perforating to large bowel has not been reported. Here, we are reporting a very rare case of anterior abdominal wall abscess of tubercular origin in a 57-year-old female patient who presented with complaints of pain in upper abdomen for four months. CT scan and intraoperative findings revealed perforation of the abscess into transverse colon. Histopathology report confirmed the aetiology and origin of the abscess.
Abdominal wall, Colon perforation, Extrapulmonary tuberculosis
Case Report
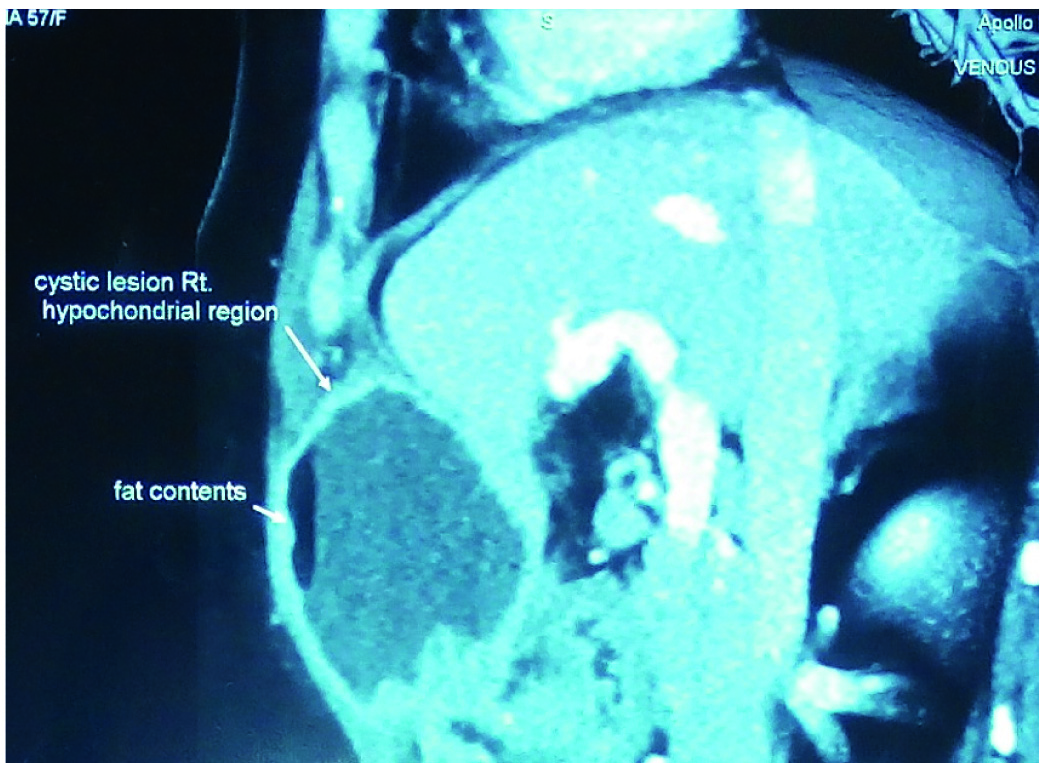
A 57-year-old female patient presented with a complain of pain in the upper abdomen for four months. It was dull aching continuous type of pain with no relation to food. It was non-radiating without any aggravating factor. She had loss of appetite and weight loss of 4 kg over four months. There was no history of vomiting, melena, constipation, fever or jaundice. She had no comorbid illness or history of prior abdominal surgery. Before coming to our hospital, she was evaluated elsewhere and found to have cystic abdominal swelling and underwent ultrasound guided aspiration. Aspirated fluid cytology was negative for malignancy and no growth was seen on aerobic culture. Physical examination revealed ill defined non tender fixed lump over deep parietal wall (approximate size – 8 cm X 8 cm) at right hypochondrium. There was no other positive physical finding. Ultrasonography showed thick walled cystic lesion with debris in deeper layers of abdominal wall, suspecting rectus sheath haematoma or soft tissue neoplasm with central necrosis. Later, multidetector CT scan delineated well defined hypodense cystic lesion (7 cm x 6.4 cm x 5.0 cm) with thick enhancing walls, over right hypochondriac region underlying rectus muscle and anterior to peritoneum [Table/Fig-1]. The underlying peritoneum was diffusely thickened with enhancing nodule in transverse mesocolon. There was intraperitoneal extension and it was closely applied to segment 4B of liver. Adjacent liver parenchyma was edematous. Lesion was adherent to anterior stomach wall at antropyloric region. Haematological and biochemical parameters were within normal limit. Upper GI endoscopy was normal.
CT scan of the abscess and surrounding organs.
One of the differential diagnoses was transverse colon pathology (unknown malignancy) with perforation and involvement of surrounding area. She underwent elective surgery. Abscess cavity was found beneath the right rectus muscle containing air and about 50 ml thick pus with intraperitoneal extension. Abscess wall was adherent to liver (Segment 4B) tissue and anterior wall of stomach at prepyloric region [Table/Fig-2].
Intraoperative finding showing abscess wall adherent to surrounding organs.

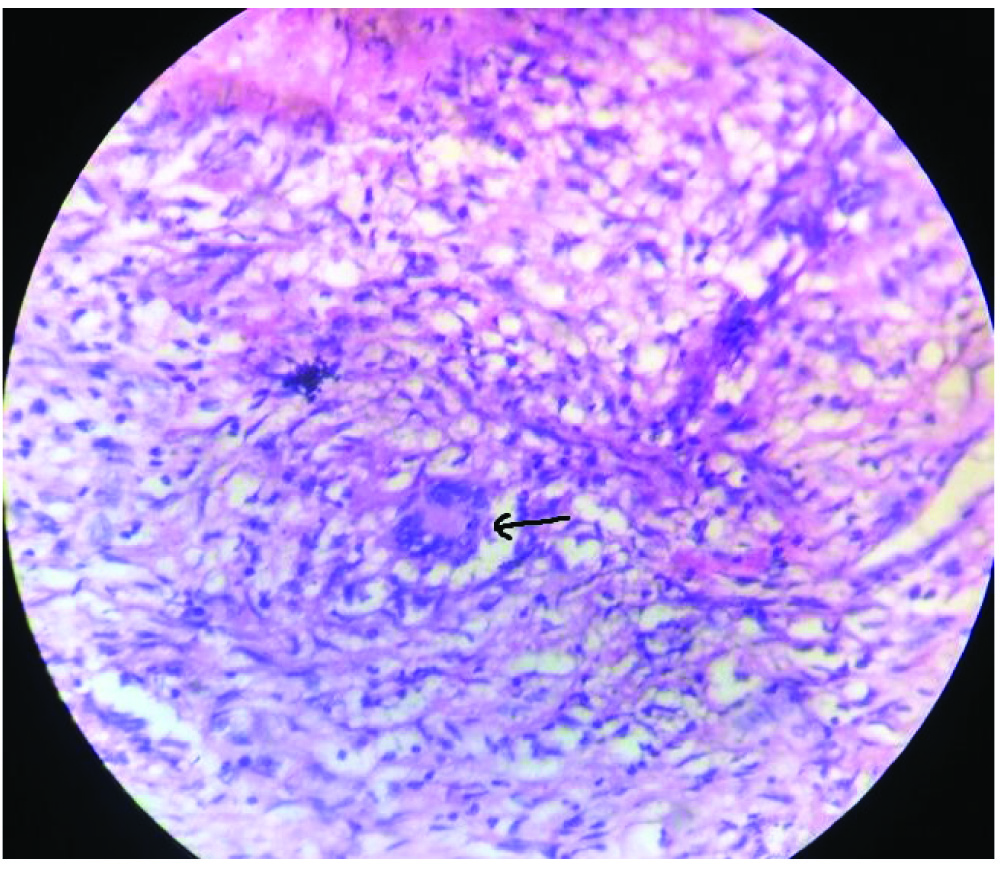
Rest of liver was normal. Abscess cavity was densely adherent to the proximal transverse colonic wall. Rest of the colon and other organs were normal. Abscess cavity was dissected all around with a rim of liver tissue with it. Segmental colonic resection was done. Pus was sent for culture and cytological analysis. On dissecting the specimen, abscess cavity was found to be connecting to colonic lumen. Surrounding colonic wall appeared normal, except at the site of perforation [Table/Fig-3]. She had an uneventful postoperative recovery and discharged on sixth postoperative day. Cytology of pus revealed chronic inflammatory cells and culture was negative after 48 hours. Biopsy report revealed tuberculosis, arising from abdominal wall with perforation to colon [Table/Fig-4]. Gene test was positive for tuberculosis.
Specimen showing perforation into colon.

Histopathology-tubercular granuloma (Langhans giant cell, H&E stain, Magnification 200X).
Colonoscopy was done three weeks after surgery which did not reveal any pathology. Patient received antitubercular drugs for six months and was doing well during follow up till 15 months.
Discussion
Of all the tuberculosis patients, 11%-16% present with involvement of extrapulmonary sites, out of which only 3%-4% have abdominal tuberculosis [1]. It is more commonly seen in developing countries like India. The increasing incidence and prevalence of HIV/AIDS patients has caused recent resurgence of extrapulmonary tuberculosis [2]. Tuberculosis of abdomen can be intestinal or extraintestinal according to the location or organ of involvement. It comprises of tuberculosis of gastrointestinal tract, peritoneum, omentum, mesentery and its lymph nodes and sometimes abdominal organs like liver, spleen and pancreas. The presentation resembles with many abdominal conditions which can clinically be either acute or chronic. Primary abdominal wall tuberculosis is rarely seen and few isolated cases or case series have been found in literature [3-5]. The incidence of primary muscular tuberculosis has been reported as 0.015% [3]. There are two possible ways to get skeletal muscle of anterior abdominal wall involved. Most commonly it spreads to the muscle through extension from the nearby structures like lymph nodes, bone, joint or tendon [4]. A tubercular abscess from neighbouring structures may track down to the rectus and may spread between the internal oblique and transverse abdominis muscles. It may also involve the rectus sheath and muscle. It can also involve the abdominal wall muscles by haematogenous spread. Sometimes, it can be due to intra-abdominal tuberculosis with extension to anterior abdominal wall which is very rare. Cases of isolated abdominal wall tuberculosis have been reported, where pulmonary and other extrapulmonary sites are uninvolved [5]. Because of such rarity, our preoperative diagnosis was not tuberculosis. Abe K et al., has discussed a case report of liver abscess extending to anterior abdominal wall [6]. In that case, it was a subcapsular left lobe liver abscess with direct extension to anterior abdominal wall. Similarly, Gupta G et al., and Pandya JS et al., reported cases of tubercular liver abscess of right lobe rupturing to anterior abdominal wall in a 35-year-old woman [7,8]. Extensive literature search did not reveal such case of parietal wall tuberculosis extending to bowel and causing perforation. Our case is a unique case of this type which is extremely rare. The initial impression from intraoperative finding was colonic pathology extending to pericolic area and anterior abdominal wall. But, after opening the lumen of resected colon, the surrounding mucosa and the wall were normal around the perforation. It indicated extracolonic pathology perforating to colon. Also to mention, isolated tuberculosis of transverse colon is unusual and rare. Biopsy report and follow up normal colonoscopy confirmed abdominal wall tuberculosis extending and perforating to transverse colon. Gene test also was positive for tuberculosis. Because of paucity of literature, it is difficult to describe the exact pathogenesis of abdominal wall tuberculosis perforating to bowel lumen.
Conclusion
Parietal wall abscess of tubercular origin is unusual and perforating into adjacent bowel loop is a rare phenomena. But, such rare presentation is possible in developing countries like India and should be considered as an uncommon differential diagnosis.
[1]. Sharma SK, Mohan A, Extrapulmonary tuberculosisInd J Med Res 2004 124:316-53. [Google Scholar]
[2]. Sharma SK, Mohan A, Kadhiravan T, HIV-TB co-infection: Epidemiology diagnosis and managementInd J Med Res 2005 121:550-67. [Google Scholar]
[3]. Malhotra MK, Cold abscess of the anterior abdominal wall: An unusual primary presentationNigerian Journal of Surgery 2012 18(1):22-23. [Google Scholar]
[4]. Nuwal P, Dixit R, Tuberculosis of rectus abdominis muscleIndian J Chest Dis Allied Sci 2007 49:239-40. [Google Scholar]
[5]. Dhar AM, Bhargava S, Bankata S, Isolated abdominal parietal cold abscess diagnosed on ultrasoundIndian J Radiol Imaging 1999 9:157-58. [Google Scholar]
[6]. Abe K, Aizawa T, Maebayashi T, Nakayama H, Sugitani M, Sakaguchi M, Isolated tuberculous liver abscess invading the abdominal wall: report of a caseSurgery Today 2011 41(5):741-44. [Google Scholar]
[7]. Gupta G, Nijhawan S, Katiyar P, Mathur A, Primary tubercular liver abscess rupture leading to parietal wall abscess: A rare disease with a rare complicationJ Postgrad Med 2011 57:350-52. [Google Scholar]
[8]. Pandya JS, Kandekar RV, Tiwari AR, Kadam R, Adhikari DR, Primary liver abscess with anterior abdominal wall extension caused by mycobacterium tuberculosis complexJournal of Clinical and Diagnostic Research 2016 10(11):PD08-PD09. [Google Scholar]