Fractures of distal femur reportedly account for less than 1% of all fractures and 4%-6% of all femoral fractures [1]. Supracondylar femur fractures occur typically due to two discrete mechanisms of injury and in two separate populations. First, in young adults after high energy trauma (60% males <40 years; accidents and sports trauma) and second, elderly population after low energy trauma (60% females, older than 60 years; falls sprains etc.,). Periprosthetic fractures of distal femur proximal to a previous total knee arthroplasty or distal to a total hip arthroplasty is distinguished as the third common population. They are a part of polytrauma in 30% of cases [2]. Open fractures comprise 27% of cases and 58% have intra-articular extensions [3].
The optimal method of treatment is still disputed. After the recent advances in techniques and implants, nonsurgical methods have largely fallen out of favour [4]. With the advent of minimally invasive approaches to honor the concept of biological osteosynthesis, complication rates have declined. Locking plates employ a minimally invasive biologically friendly insertion technique with minimal soft issue stripping securing the blood supply as well as the fracture haematoma. A major headway in the management of these fractures came in 1988 with the arrival of intramedullary nail put in a retrograde fashion by Green [5] which shares many of the assets of locking plate and have been claimed to have high healing rates [6]. Despite the universal use of both the techniques, only a few studies are accessible to contrast them.
In this randomized prospective study, we compared and assessed the radiological and functional outcomes of extra articular distal femur fractures stabilized with a Retrograde Nail (Group RN) or a Locking Plate (Group LP) utilizing LISS techniques.
Materials and Methods
The study included 42 patients operated between July 2011 to January 2014 satisfying the inclusion and exclusion criteria. This was an institutional review board approved randomized prospective analysis of patients with Orthopaedic Trauma Association (OTA)/ Arbeitsgemeinschaft für Osteosynthesefragen (AO) (German for “Association for the Study of Internal Fixation”, or AO) type A distal femur fractures undergoing close reduction and internal fixation with a (Group RN) or a (Group LP) utilizing LISS techniques. Radiological and functional outcomes were assessed and compared. All subjects gave full and informed consent to participate in the study.
Inclusion Criteria
Age >18 years;
Supracondylar femur fractures and supracondylar fractures with fracture line extending to distal third of femoral shaft;
Polytrauma patients without ipsilateral lower limb fractures.
Exclusion Criteria
Follow up <18 months;
Fractures with intra-articular extensions;
Associated knee ligament tears;
Old fractures (>3 weeks);
Gustilo grade 3b and 3c open fractures;
Associated neurovascular injury;
Preexisting significant ipsilateral limb joint arthritis or comorbidities hampering rehabilitation;
Periprosthetic supracondylar femur fractures.
A total of 42 patients matched our criteria and were segregated into two groups: Group LP (22 patients) and Group RN (20 patients) [Table/Fig-1]. Fractures were classified as per the Orthopaedic Trauma Association (AO/OTA) classification [7]. One-way-ANOVA test was used to analyze the difference of means for different parameters. The test was referenced for a two-tailed p-value and 95% confidence interval was constructed around sensitivity proportion using normal approximation method. The Fishers-Exact test was used for the comparison of paired categorical variables.
Demographic and fracture pattern in two groups.
| Parameters | Group LP (22 Subjects) | Group RN (20 Subjects) |
|---|
| Mean Age± SD (years) | 38.7±15.6 | 36.0±14.1 |
| GenderMaleFemale | 1606 | 1307 |
| SideRightLeft | 1309 | 1109 |
| Mode of TraumaHigh EnergyLow Energy | 1408 | 1406 |
| Type of fractureClose fractureOpen fractureGrade 1Grade 2Grade 3a | 1507010303 | 1505010202 |
| Classification (AO/OTA)33-A133-A233-A3 | 090805 | 071003 |
| Mean Preoperative Stay ±SD (days) | 6.2± 2.7 | 5.2± 2.5 |
| Mean follow up± SD (months) | 29.2 ± 9.2 | 27.8 ± 7.0 |
Statistical Anaylysis
SPSS software was used to perform statistical analyses. A value of <0.05 was considered statistically significant.
AP and Lateral X-Ray views of the knee with distal femur were procured to examine fractures. Uncommonly, CT scanning was implemented in cases with suspected intra-articular extensions and profound communition. If sluggish perfusion or a vascular injury was speculated, a conventional or a CT angiography was indicated. An AP view of pelvis with both femora too constituted our diagnostic protocol.
Operative Procedure
The surgeries were performed by the same team of orthopaedic surgeons without ascribing any preference to any implant. All surgeries were accomplished under spinal/epidural or general anaesthesia. No pneumatic tourniquet was used in any of the surgeries.
LP group: The patient was positioned supine on a radiolucent OT table under fluoroscopy imaging with a bolster under the knee to acquire flexion of 20-40 degree in order to relax the deforming force of gastrocnemius; thereby avoiding the typical hyperextension of distal fragment.
Pre-applied proximal tibial traction pin was used intraoperatively to attain reduction. A lateral incision extending just proximal to the joint line was used. The distal femoral LCP was slip under the vastus lateralis proximally and provisionally fixed with k wire distally. Close reduction was accomplished with traction and external manipulation. Essential instruments like Lowmans’ forceps, femoral distractor, percutaneous clamps etc., were kept at bay and employed wherever deemed necessary. Locked screws were inserted in the proximal part of the bone through plate percutaneously with the help of second plate of same size kept over the skin laterally and image intensifier. Skin stab wound were applied through second plate over skin over corresponding screw holes. A screw in compression mode was used in the proximal fragment in case of a need to attain compression at the fracture site. The reduction and hardware placement were confirmed under fluoroscopy. Knee was moved through ROM and ligamentous stability established under anaesthesia.
Retrograde nail: Patients were settled supine with access to fluoroscopy. The affected leg was placed in 60 degree flexion at knee. A 3 cm longitudinal infra-patellar skin incision was centered over the patellar tendon and tendon split longitudinally in its middle. The insertion point was confirmed radiologically with both AP and lateral views in the intercondylar notch anterior to the Blumensaats’ line and in projection of the femoral shaft axis. PCL was identified and entry taken with a bone awl 1 cm anterior to it. A guide wire was inserted respecting the normal 7 degree valgus angle of the knee to the horizontal plane. The fracture was reduced, guide wire extended to intubate the proximal fragment up to a level proximal to the lesser trochanter. Sequential reaming in 1 mm increments was executed until the cortical chatter was appreciated. A nail of size 1 mm less than the last reamer employed was inserted and advanced with the final position of distal end well below the subchondral bone established under fluoroscopy. The distal locking screws were inserted using the aiming device and trocar. Proximally, free hand locking of two interlocking bolts was implemented.
Injectable antibiotics were administered for three to five days after surgery followed by oral, till suture removal. Patients were discharged on 5th-14th day after surgery. Isometric quadriceps exercises and knee hip ankle exercises were initiated at the end of first postoperative day. Non weight bearing mobilization with walker was done from 2nd day onwards. Patients were called for follow-up at two weeks, four weeks and then monthly till six months and three monthly thereafter. Partial weight bearing was consented as per the stability of the fracture at 3 weeks in cases with AO/OTA type A1 fractures and within 6 weeks in AO/OTA type A3 fractures and all fractures in the LP group. Full weight bearing was approved after ascertaining radiological union in both the groups.
At each follow up, AP and lateral views of fracture were obtained. Pain was assessed on Visual Analogue Scale (VAS). Clinical examination comprised of checking for incisional healing, knee stability, alignment, range of motion and any other complication. Osseous healing was designated radiologically as the presence of atleast three of the four cortices with bridging callus formation and crossing trabeculae in AP and lateral radiographs. Absence of pain and tenderness at fracture site dictated the achievement of clinical healing.
Groups were compared in terms of intraoperative parameters (duration of surgery, blood loss), time to union and functional results. Functional results were determined using Knee Society Score (KSS) [8] at 18 months follow up that included knee ROM, pain, deformity, walking, stair climbing capacity and knee stability. Results were allocated as excellent, good, intermediate or poor.
Results
Group LP was composed of 22 patients (16 males and 6 females; mean age 38.7±15.6). Group RN comprised 20 patients (13 males and 7 females; mean age 36.0±14.1). Mean time to surgery was 6.2±2.7 (range 2-12) days in group LP and 5.2±2.5 (range 2-11) days in group RN. The average intraoperative time as well as the blood loss was recognized to be significantly more in group RN as compared to group LP [Table/Fig-2].
Intraoperative parameters in two groups.
| Parameters | Group LP | Group RN | p-value |
|---|
| Mean operating time SD | 88.4±17.6 | 102.3±20.6 | 0.024 |
| Intraoperative blood loss | 228.2±45.8 | 323.0±74.3 | <0.001 |
Mechanism of injury was high energy impact in 63.6% in LP group and 70% in RN group and low energy injury in 36.4% in LP group and 30% in RN group. Average follow up was 29.2±9.2 months in group LP (range 18 to 52 months) and 27.8±7.0 months in group RN (range 18 to 43 months).
Union: Mean duration until union was 26.5 weeks (SD=12.9; range 12 to 64 weeks) in the group LP and 22.6 weeks (SD=13.1: range 12 to 60 weeks) in the group RN. The difference came out to be statistically insignificant [Table/Fig-3].
Functional results in two groups.
| Parameters | Group LP | Group RN | p-value |
|---|
| Union rate | 90.9% | 90% | 1.00 |
| Average time to union (weeks) | 26.5± 12.9 | 22.6± 13.1 | 0.312 |
| Range of motion | 112.0± 9.8 | 107.0 ±9.9 | 0.106 |
| Mean KSS score | 74.4± 10.9 | 77.6± 8.6 | 0.288 |
Delayed union was detected in five patients in group LP and in one patient in group RN. The group RN patient underwent dynamisation at six months.
Nonunion was perceived in two patients in either group. Three of them underwent autologous iliac crest bone grafting with dynamisation in group RN patients and all of them subsequently united 5 to 8 months thereafter. The fourth one was the one who underwent plating and also had deep infection.
Complications: Superficial infections were discerned in four patients in patient LP and two in patient RN and were tackled with antibiotic therapy. One patient in each group developed deep infection. Each of them underwent implant removal and debridement after fracture union. Infection resolved in one to two months thereafter. There was no statistically significant difference in overall incidence of malalignment in any plane. Loosening of plate was discovered in one patient at four months follow-up. Partial weight bearing was then advised and his fracture united at eight months allowing implant removal at nine months [Table/Fig-4].
Postoperative complications in two groups.
| Complications | Group LP | Group RN | p-value |
|---|
| Union disturbance rateDelayed unionNonunion | 31.8%52 | 15%12 | 0.2840.18701.00 |
| Malalignment >10 deg | 1 | 2 | 0.597 |
| 5-10 deg | 2 | 4 | 0.400 |
| Superficial infection | 4 | 2 | 0.665 |
| Deep infection | 1 | 1 | 1.00 |
| Haematoma formation | 3 | 2 | 1.00 |
| Anterior knee pain | 4 | 1 | 0.174 |
| Implant loosening | 1 | 0 | 1.00 |
There were also no statistical significance in the ROM and KSS score in between the two groups [Table/Fig-5].
Knee Society Score (KSS) in two groups.
| Parameters | Group LP | Group RN |
|---|
| Excellent (80-100) | 8 | 9 |
| Good (79-70) | 9 | 7 |
| Fair (69-60) | 3 | 3 |
| Poor (<60) | 2 | 1 |
Discussion
Despite modern fixation techniques, distal femur fractures often result in continued disability and worse outcomes [9]. Although newer biological methods of fixation have reduced the union and infection problems, their treatment still remains an enigma to the treating orthopaedic surgeon.
Two habitually applied methods are Retrograde Intramedullary Nailing (RIMN) and bridge plating [10-12]. The Less Invasive Stabilization System (LISS) [5] acts as an extra medullary anatomically contoured internal fixator with the main asset of soft tissue preservation [9]. They have been credited to have the best functional outcome in both extra as well as intraarticular fractures surpassing DCS and RN by Chander A et al., [13]. They offer good fixation in osteoporotic bones of elderly patients too [6,14,15]. But, prior to plate fixation, fracture reduction needs to be assured. Since the locking plate and screws are not designed to approximate the fracture to the plate, it may render satisfactory reduction more formidable [5]. Weight bearing is also delayed. Implant failure and union problems have been cited [16,17].
Being an intramedullary load sharing device, RIMN extends a distinct assistance in early loading and appears to be an appealing alternative for these fracture but persistent knee pain, conceivable development of knee arthrosis and systemic complications remain a setback for nailing [10].
In our study, earlier union rate was noticed in the nailing group with fractures uniting almost four weeks earlier on an average than plating group but the difference was statistically insignificant. Delayed union was also more frequently detected in plating group with five cases as against only one in nailing group although this difference too came out to be statistically insignificant. There were also no overall statistically significant union disturbance rates (delayed union+nonunion) [Table/Fig-6,7].
(a) Case 1- Preoperative radiograph of supracondylar femoral fracture; (b) Case 1- Postoperative radiograph of supracondylar femoral fracture managed by locking plate; (c) Case 1- Follow up radiograph at 12 weeks showing callus formation; (d) Case 1- Follow up radiograph at 20 weeks showing fracture consolidation.
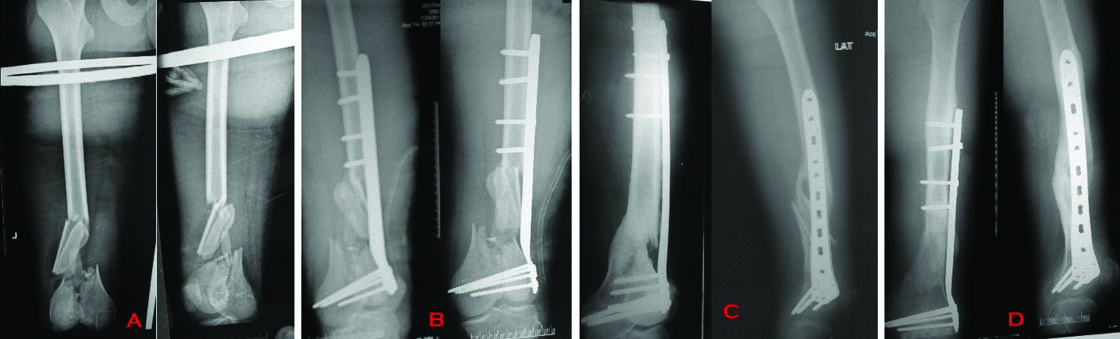
(a) Case 2- Preoperative radiograph of supracondylar femoral fracture; (b) Case 2- Follow up radiograph at 12 weeks showing callus formation after locked plating; (c) Case 2- Follow up radiograph at 20 weeks showing fracture consolidation.
The statistically insignificant mean duration time and union rates perceived in our study is echoed by many previously done studies [10-12]. Comparable nonunion rates have been published by them. On the contrary, in a systematic review of 29 case series with 415 patients, 5.3% nonunion rates with LP as opposed to 1.5% in nailing were proclaimed by Herrara DA et al., [18]. Gao K et al., too found no statistically significant difference in the above parameters although overall union disturbance rates (delayed union + nonunion) were recognized to be higher in plating group in divergence with our study [12].
The release of the medullary contents at the fracture site during the process of preparation for and insertion of nail offers a plausible reason for earlier propensity towards union in these patients as was discerned by us. An intramedullary stabilization along with a long working length also appears to be an adjuvant factor. In their study Henderson CE et al., discovered a two to four times more callus formation at the fracture site at 12 weeks after fixation in nailed patients than in plated patients [19].
Suboptimal placement of plate and locking screws might also be culpable for lengthened union time in plated patients as was seen in two patients with delayed union in our series. Henderson CE et al., discovered no empty holes next to fracture site in 71% of nonunion [19]. Strategic placement of screws away from the fracture site to increase the working length thus allowing elastic deformation of plate screw construct is paramount and thus surgical techniques rather than the choice of implant have a greater impact in optimizing outcomes [8,20]. Currently, leaving 3 to 4 empty holes at the level of fracture on both sides is advocated with a screw ratio of 0.4 to 0.5 [21-23].
Although, RN has been disreputed to produce angular malunion [24,25], employing thicker and longer nails extending proximal to lesser trochanter as well as blocking screws wherever needed checked malalignment in nailed patients and overall commensurable results were detected in between the groups in agreement with many previous studies [12,26]. The mechanical interaction between the femoral diaphysis and nail is enhanced by a snug nail bone fit [27] [Table/Fig-8,9].
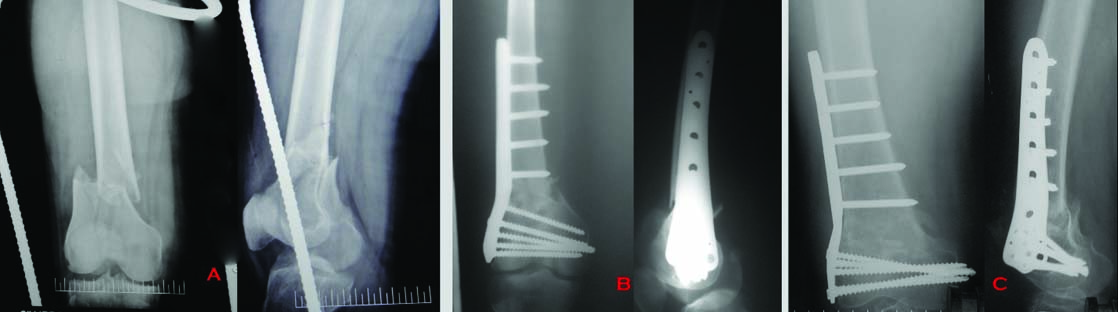
(a) Case 3- Preoperative radiograph of supracondylar femoral fracture; (b) Case 3- Postoperative radiograph of supracondylar femoral fracture managed by locking plate; (c) Case 3- Follow up radiograph at 20 weeks showing fracture union.

(a) Case 4- Preoperative radiograph of supracondylar femoral fracture; (b) Case 4- Postoperative radiograph of case managed by supracondylar nail; (c) Case 4- Follow up radiograph at 12 weeks showing fracture union; (d) Case 4- Follow up radiograph at 20 weeks showing fracture union.
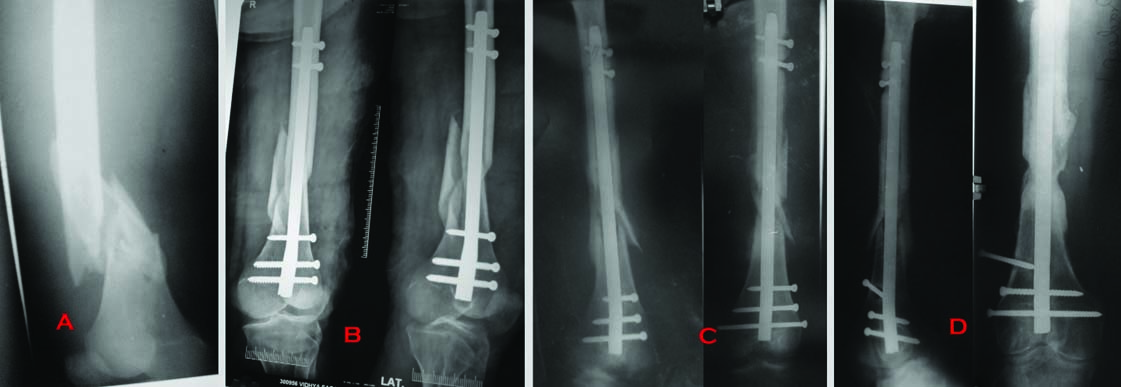
In spite of taking extra efforts to avoid injuring the patellar and femoral cartilage throughout the procedure as well as confirming the distal extent of nail fluoroscopically, anterior knee pain was acknowledged by 20% of our nailed patients and it came out to be statistically insignificant. Two of them had their nails extracted 12 to 18 months after primary surgery. This also did not yield any significant difference in the final ROM which although was more in plating group (p=.106). Long term studies are needed to validate the potential for knee arthrosis secondary to cartilage damage with retrograde nailing.
Talking of deep infection, we had one patient in each group who developed deep infection. Both of them had presented with an open fracture initially. Similar infection rates have been reported by antecedent studies [11,12,15,26,28,29]. Minimally invasive biologically friendly surgical techniques respecting the normal fracture biology appears attributable for low infection rates in both the groups.
Concerns have been voiced for systemic complications secondary to embolization of marrow contents especially with concomitant thoracic trauma [30,31]. We did not have any such incident in our series. Intraoperative time as well as the intraoperative blood loss was significantly more in nailing group. Reaming the medullary canal to get a snugly fitting nail is blame worthy for both. Free hand locking of the proximal screws with nail is also liable for elevated mean operating time with nailing. Gao K et al., documented comparable intraoperative time but increased blood loss with nailing [12].
Functional achievement at 18 months follow up came out to be almost similar in our research. The measurement was carried out on KSS system and it furnished comparable results in between the groups [Table/Fig-10]. Past studies too have discovered undifferenced functional results despite using different functional scoring systems. [11,12,26,28,29]. Demirtas A et al., in their study, using Sanders criteria, announced equivalent patients with excellent to good and fair to bad results [26]. A few studies used Knee Osteoarthritis Outcome Scoring system (KOOS) [28] and had analogous observations. Concordant findings were also narrated by Markmiller M et al., with Lysholm Gillquist scoring system, Gao K et al., and Gupta SKB et al., employing the Hospital for Special Surgery Score (HSS) [11,12,29]. Paradoxically, in a recent study, Hoskins et al., revealed a significant difference in the quality of life in favour of IMN using EuroQol-5 dimensions score at six months although there was weak evidence that the trend continued for one year [32].
Case 4- Clinical outcome of the case managed by supracondylar nail.

Few number of patients with some variability in locking plate techniques in terms of plate length and screw position remain a constraint of our study. Surgical techniques tend to determine final outcome more than the choice of implant. Multicentric studies with more number of patients and longer follow ups will be more dependable to draw any conclusions.
Conclusion
To conclude, nailing proved more cumbersome intraoperatively due to escalated operating time and blood loss and successive anterior knee pain necessitating implant removal but this detriment may be offset by an inclination towards earlier union. With LISS, technical errors are more common and less forgiving and must be overcome with proper preoperative planning and intraoperative attention to detail. With the emergence of modern day locked plates with new innovations like far cortical locking, results are apprehended to improve in near future.