Cytological Diagnosis of Primary Cutaneous Aspergillosis Masquerading as Lipoma in a Known Case of Lepromatous Leprosy
Savitri M. Nerune1, Swati Arora2, Mayank Kumar3
1 Assistant Professor, Department of Pathology, B.L.D.E. University’s Shri B.M. Patil Medical College, Vijayapur, Karnataka, India.
2 Postgraduate Student, Department of Pathology, B.L.D.E. University’s Shri B.M. Patil Medical College, Vijayapur, Karnataka, India.
3 Postgraduate Student, Department of Pathology, B.L.D.E. University’s Shri B.M. Patil Medical College, Vijayapur, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Savitri M. Nerune, B.L.D.E. University’s Shri B.M. Patil Medical College, Vijayapur-586103, Karnataka, India.
E-mail: saviraj31j@gmail.com
Primary cutaneous aspergillosis is a rare disease, caused by organisms like Aspergillus flavus and Aspergillus fumigatus. Fine Needle Aspiration Cytology (FNAC) is a simple and well established tool for the diagnosis of mycotic infections. We report a case of forearm swelling that presented clinically as lipoma in a known case of lepromatous leprosy. It was diagnosed as primary cutaneous aspergillosis on FNAC, which was subsequently confirmed on culture. Cutaneous aspergillosis co-existing with leprosy has rarely been reported in the literature and early diagnosis of aspergillosis in immunocompromised patients is mandatory.
Fine needle aspiration cytology, Fungal infection, Immunocompromised host
Case Report
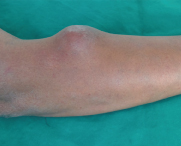
A 48-year-old male presented with complaint of swelling over the right forearm since nine months. The patient was a known case of lepromatous leprosy with recurrent Erythema Nodosum Leprosum (ENL), for which he was on multi-drug therapy consisting of dapsone (100 mg daily), rifampacin (600 mg once in a month) and clofazimine (300 mg once in a month), along with systemic corticosteroids for three months. General physical examination showed single, soft fluctuant swelling on extensor aspect of right forearm measuring 4x3 cm [Table/Fig-1]. There was no history of trauma or any invasive procedure. Patient was non-diabetic and HIV seronegative. Other haematology and biochemical parameters were normal. With clinical diagnosis of lipoma, patient was referred for FNAC examination of the swelling.
Single, soft fluctuant swelling on extensor aspect of Rt. forearm measuring 4 x 3 cm (left);
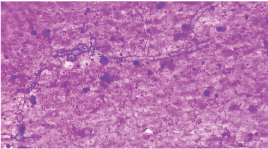
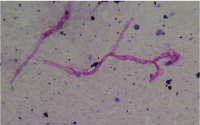
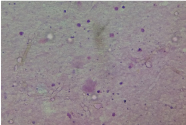
FNAC was done after informed written consent, and it yielded thick pus-like aspirate. Microscopic examination of aspirate showed many septate filamentous hyphae with acute angle branching in an inflammatory and necrotic background [Table/Fig-2]. Ziehl-Neelsen stain for acid fast bacilli was negative. Periodic Acid-Schiff (PAS) stain showed many septate filamentous hyphae with acute angle branching suggestive of Aspergillus [Table/Fig-3]. Cytological diagnosis offered was cutaneous aspergillosis. Abscess was drained and sent for microbiological study. A direct KOH mount showed thin septate hyphae with acute angle branching [Table/Fig-4]. Culture revealed greenish white cotton wool colonies after 48 hours of incubation at 37oC on Sabouraud’s dextrose agar, thus confirming the species as Aspergillus flavus.
Photomicrograph of aspirate showing many septate filamentous hyphae with acute angle branching in a inflammatory and necrotic background. (Giemsa 100X) (right).
Periodic acid-Schiff stain shows many septate filamentous hyphae with acute angle branching suggestive of Aspergillus (PAS 40X) (left);
Direct KOH mount shows thin septate hyphae with acute angle branching (40X) (right).
The patient was treated with voriconazole 300 mg twice daily for two months followed by 200 mg twice daily for next four months. There was good improvement in patient’s clinical condition on follow up for six months.
Discussion
Primary cutaneous aspergillosis is a rare entity, which may occur as either primary or secondary infection. Primary lesion occurs by direct inoculation of spores at site of injury and secondary lesion occurs due to haematogenous dissemination from primary focus [1]. Most common organisms are Aspergillus flavus, Aspergillus fumigatus and Aspergillus niger. It is commonly seen in patients suffering from malignancies, diabetes, in patients who are on long-term corticosteroids and immunocompromised state [2]. Cytological diagnosis is a well-known method for differentiation of infective lesions from neoplastic lesions and an important tool for the diagnosis of mycotic infections [3,4].
Cutaneous diseases with multiple aetiologies are commonly encountered now-a-days, both in developed and developing countries of the world. Mycotic infections due to opportunistic fungi have gained significance in recent years and are being reported with increasing frequency in many regions of the world including India [5]. Among such group of fungi, Aspergillus infections are most common. Aspergillus is ubiquitous fungi, found in soil, water and decaying vegetations [6]. The most common species in the world is Aspergillus fumigatus, followed by Aspergillus niger and flavus. In India, Aspergillus flavus is the most commonly encountered species in such cases [3]. The importance of this case lies in the fact that in a developing country like India, co-existence of leprosy and fungal infection may lead to diagnosis of only one entity, causing delay in initiation of proper treatment [6,7].
Aspergillosis is a primary pulmonary disease, it also affects naso-orbital area, central nervous system, heart, kidney, gastrointestinal tract and skin [6,7]. The route of contamination is haematogenous dissemination [7]. Cutaneous aspergilloses may occur as primary or secondary infection. Primary infection occurs at site of injury or near the site of intravenous catheter and occlusive dressings. Secondary skin lesion can be either blood borne or from contiguous spread from infected area [8].
Clinically, the lesions of cutaneous aspergillosis are characterized by violaceous macules, papules, subcutaneous nodules, haemorrhagic bullae, ulcerations with central necrosis or subcutaneous abscess [1]. Most of the cases have been reported in immunocompromised patients, HIV patients, newborns, burn patients, cancer patients and transplant recipients [9]. In present case patient presented with subcutaneous abscess and he was a known case of lepromatous leprosy with recurrent ENL for which he was on multi-drug therapy consisting of dapsone (100 mg daily), rifampacin (600 mg once in a month) and clofazimine (300 mg once in a month), along with systemic corticosteroids for three months.
Early and definitive diagnosis is mandatory to rule out other differential diagnosis like neoplasms, inflammatory lesions and to help clinicians for appropriate management of the patients. FNAC is a well established diagnostic technique to aid in early diagnosis of the lesion which can be managed conservatively and thus can prevent undue surgery [3].
Although imaging techniques like Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) can help establishing the diagnosis, but both often fail to differentiate infectious lesion from a neoplastic one and also, all the fungi do not grow on the culture media. Hence, morphology remains the mainstay in the diagnosis which can be known by FNAC procedure and by skin biopsy. On microscopy, Aspergillus is identified by its septate hyphae and an acute angle branching. Aspergillus can be differentiated from Mucor easily on the basis of morphological features as Mucor has broad, non-septate hyphae and right angle branching [3].
Primary cutaneous aspergillosis needs to be recognized early because of the differences in the features, management and prognosis from the secondary infection, which is associated with poorer prognosis and also any skin lesion in immunocompromised patient should be analysed immediately for early diagnosis of invasive aspergillosis [10]. Management is usually by topical and systemic antifungal agents like itraconazole, voriconazole, amphotericin B and caspofungin [9,10].
Conclusion
This case is being presented to increase the awareness of clinicians and pathologists that primary cutaneous aspergillosis could present as subcutaneous nodule, as in the present case it presented clinically as lipoma. This condition can be diagnosed accurately by FNAC, which is simple and inexpensive technique which will aid in correct diagnosis and management of the patient. Early diagnosis and awareness of multiple aetiologies for skin lesions will help in prompt and correct treatment.
[1]. Venugopal T, Venugopal P, Primary cutaneous aspergillosis from Tamilnadu diagnosed by fine needle aspiration cytologyMed Mycol Case Rep 2012 1:103-06. [Google Scholar]
[2]. Mohapatra S, Xess I, Swetha JV, Tanveer N, Asati D, Ramam M, Primary cutaneous aspergillosis due to aspergillus niger in an immunocompetent patientIndian J Med Microbiol 2009 27:367-70. [Google Scholar]
[3]. Sharma D, Mahajan N, Rao S, Khurana N, Jain S, Invasive maxillary aspergillosis masquerading as malignancy in two cases: Utility of cytology as a rapid diagnostic toolJ Cytol 2012 29:194-96. [Google Scholar]
[4]. Duraipandian J, Rengasamy G, Madasamy B, Kulanthaivelu A, Subramanian G, Subcutaneous aspergillosis with coexisting atypical mycobacterial infectionIndian J Pathol Microbiol 2010 53:359-60. [Google Scholar]
[5]. Dave P, Mahendra R, Mahendra P, Aetiologic significance of Aspergillus terreus in primary cutaneous mycosis of an agricultural workerMol Microbiol 2015 5:1-4. [Google Scholar]
[6]. Nasit JG, Sojitra N, Bhalra R, Dhruva G, Aspergillosis of bilateral breast and chest wall in an immunocompetent male masquerading as breast cancerInt J Health Allied Sci 2013 2:212-15. [Google Scholar]
[7]. Segundo JBA, Neto da Silva MAC, Filho WEM, Nascimento ACB, Vidal FCB, Bezerra GFB, Cerebral aspergillosis in a patient with leprosy and diabetes: a case reportBMC Res Notes 2014 7:689-93. [Google Scholar]
[8]. Sharma S, Yenigalla BM, Naidu SK, Pidakala P, Primary cutaneous aspergillosis due to Aspergillus tamarii in an immunocompetent hostBMJ Case Rep 2013 2013:010128 [Google Scholar]
[9]. Rabbani MZ, Amir M, Khan MY, Khan AS, Ali Z, Primary aspergillosis of cheek. A diagnostic dilemmaJ Pak Med Assoc 2007 57:613-15. [Google Scholar]
[10]. Bernardeschi C, Foulet F, Ingen-Housz-Oro S, Ortonne N, Sitbon K, Quereux G, Cutaneous invasive aspergillosis: retrospective multicenter study of the French invasive-aspergillosis registry and literature reviewMedicine 2015 94:1-8. [Google Scholar]