Massive Benign Phyllodes Tumour of Breast Complicating Pregnancy
Anji Reddy Kallam1, Vandana Kanumury2, Rama Murthy Korumilli3, Vahini Gudeli4, Havya Polavarapu5
1 Director, Department of Plastic Surgery, ASRAM Medical College, Eluru, Andhra Pradesh, India.
2 Head and Professor, Department of Obstetrics and Gynaecology, ASRAM Medical College, Eluru, Andhra Pradesh, India.
3 Head and Professor, Department of Pathology, ASRAM Medical College, Eluru, Andhra Pradesh, India.
4 Associate Professor, Department of Pathology, ASRAM Medical College, Eluru, Andhra Pradesh, India.
5 Postgraduate Student, Department of Obstetrics and Gynaecology, ASRAM Medical College, Eluru, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anji Reddy Kallam, Director, Department of Plastic Surgery, ASRAM Medical College, Eluru-534004, Andhra Pradesh, India.
E-mail: reddykanji@gmail.com
Phyllodes tumour of the breast, earlier called cystosarcomaphyllodes, is a rare fibroepithelial breast neoplasm that occurs in all age groups from adolescents to elderly. Phyllodes tumour occurring during pregnancy and associated with lactating breast is extremely rare. Giant phyllodes tumours or giant fibroadenomas are those measuring more than 10 cms in diameter and weighing more than 500 gm. Phyllodes tumour typically exhibits an exclusive intracanalicular growth pattern of fibroepithelial cells with classical, deep leaf-like stromal projections into dilated lumens from which its name “phyllodes” is derived. A 32-year-old primigravida at 38 weeks of gestation, presented with massive and heavy swelling of the left breast, growing over the last eight months. Physical examination revealed a massively enlarged left breast with palpable, firm, nodular mass measuring 10 x 20 cm and occupying whole of the left breast. A trucut biopsy demonstrated a fibroepithelial lesion suggestive of benign phyllodes tumour. Simple mastectomy was performed six days after the delivery of the baby by caesarean section. The histopathological report confirmed the diagnosis as benign phyllodes tumour with ductal hyperplasia and no atypia. We are reporting this case because of its massive size, associated with lactating breast and difficulty in histopathological differentiation from Giant fibroadenoma.
Benign disease of the breast, Fibroadenoma, Giant fibroadenoma, Lactating adenoma
Case Report
A 32-year-old female, primigravida, at 38 weeks of gestation, presented with a large swelling of the left breast growing for the last eight months. The mass was small in size when she first noticed eight months back and rapidly increased in size during the course of pregnancy. The mass was associated with severe discomfort because of its size and weight and was painful. There was no history of trauma, previous breast disease or family history of breast cancer.
Physical examination of the left breast revealed a massive swelling occupying all the quadrants of the breast, particularly huge in the medial upper and lower quadrants and stretching the overlying skin and displacing the nipple-areola complex towards the left lateral side. The skin was pigmented; dilated veins were seen with peau-de-orange appearance. There was local warmth. The swelling was nodular with stretching and hyper pigmentation of the overlying skin. The swelling was 10 x 20 cm in size, nodular surface and firm in consistency with areas of softness. It was mobile and was not fixed to the underlying tissues. Breast was lactating and milk secretion through the left nipple was observed [Table/Fig-1a,b].
(a) Preoperative appearance of both the breasts with swelling left breast; (b) Preoperative showing lactation and peau-de-orange of skin left breast.

There was no significant enlargement of axillary lymph nodes. The contralateral breast examination showed a small (1 x1 cm) firm, mobile mass in the lower outer quadrant of the breast. Right axilla was normal. Ultrasonographic examination showed large well defined solid, heterogenous, predominantly hypoechoic lobulated lesion with internal vascularity in the left breast and a small hypoechoic lesion in the right breast possibly fibroadenoma.
Ultrasound guided Trucut Biopsy was performed and the cytological study revealed a fibroepithelial lesion suggestive of benign phyllodes tumour.
Differential diagnosis of a benign phyllodes tumour, giant fibroadenoma and lactating adenoma were considered and because of the clinical features a provisional diagnosis of benign phyllodes tumour was thought of and planned for simple mastectomy.
She delivered a live healthy baby by elective caesarean section. After that lactation was initiated, the symptoms worsened with increased heaviness and tenderness over the left breast. The treatment options and timing of the operation were discussed and because of the diffuse nature of the lesion and large size, simple mastectomy was decided and was done within one week after delivery under general anaesthesia, through transverse elliptical incision. The nipple areola complex that was disease free, was harvested as full thickness graft and was transplanted at the dedicated site while doing the wound closure. This is done for psychological reasons for the patient and esthetic considerations. Wound was closed with 4/0 PDS subcuticular suture.
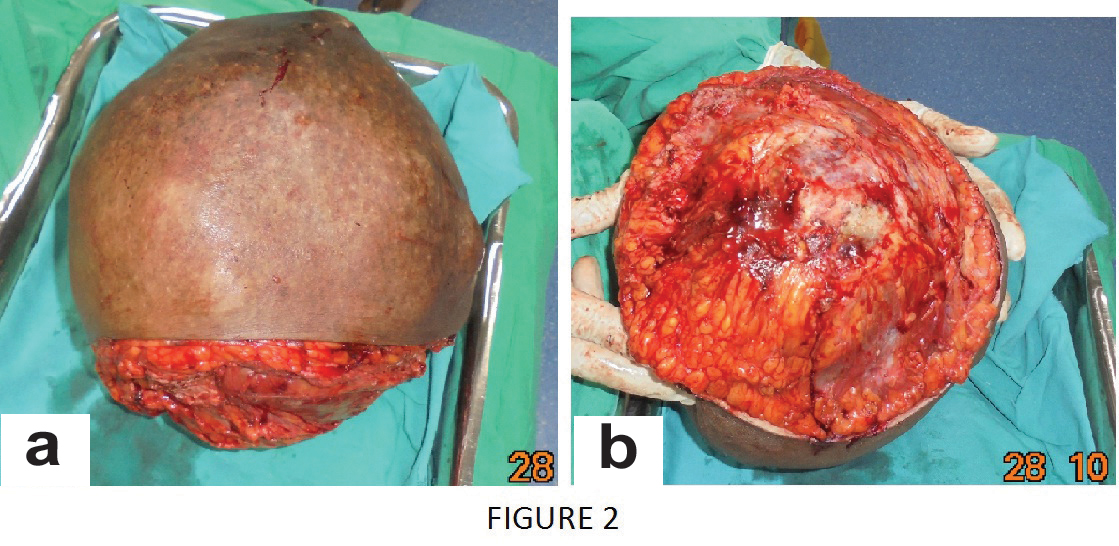
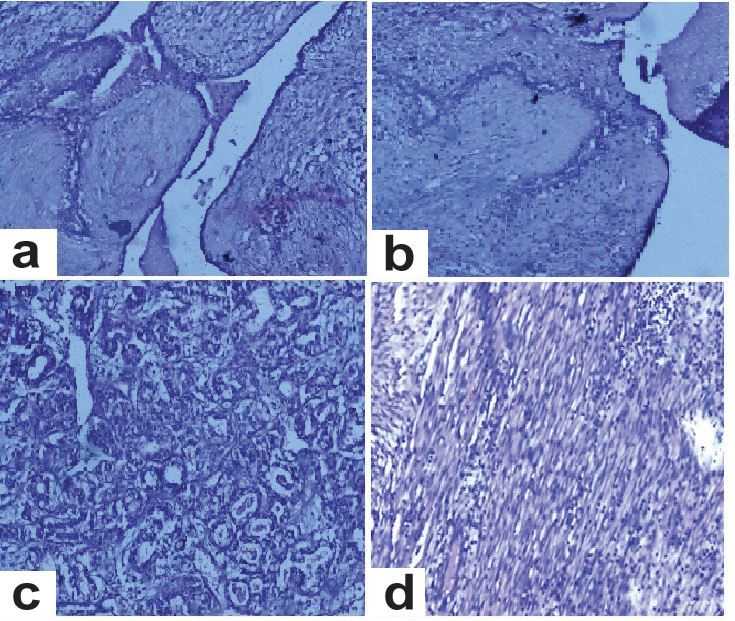
The excised specimen showed large rounded mass measuring 20 X 10 X 17 cm and weighing 4 kg [Table/Fig-2a,b]. Cut section of the mass showed well marked thick capsule, grey white, homogenous with focal yellow areas [Table/Fig-3]. Microscopically the tumour was composed of spindle cells with no mitotic activity and thrown into leafy pattern with areas of intracanalicular and pericanalicular pattern. Also seen were dilated ducts and multiple foci of ductal hyperplasia without atypia. Areas of extensive hemorrhage and infarction, necrosis were also noted, but there was no evidence of malignancy [Table/Fig-4a-d].
a) Gross specimen after simple mastectomy, measuring 20 x 10 x 17 cm and 4 kg in weight; b) Excised specimen-left breast, inner surface.
Cut section of the mastectomy specimen.

(a) H&E, X10 Histopathological examination-microphotograph showing stromal overgrowth with leafy arrangement; (b) H&E, X10 HPE-microphotograph showing stromal overgrowth and leafy appearance; (c) H&E, X40 HPE-microphotograph showing lactating adenoma with dilated ducts; (d) H&E, X100 HPE-microphotograph showing cellular stromal component with spindle cells.
Patient had an uneventful recovery and extremely comfortable after the surgery and was feeding the child from the right breast without any difficulty. She was discharged on 10th postoperative day with advise to come for checkup after four weeks [Table/Fig-5a,b]. She was comfortable and doing well after enquiries four weeks later.
(a) Post-op with nipple areola full thickness graft; (b) At the time of discharge on 10th postoperative day.

Discussion
Phyllodes tumours are rare fibroepithelial breast tumours that are capable of a diverse range of biological behaviour [1]. These tumours were originally called “Cystosarcoma Phyllodes” by Johannes Muller in 1838 [2]. They might behave similar to benign fibroadenomas or even can metastasize distantly [3]. However, the term is erroneous, since it is very rarely cystic and sarcomatous with metastases. The term ‘Phyllodes’ denotes the histological appearance of leaf-like papillary projections that denotes stromal proliferation [4,5].
Phyllodes tumours account for less than 0.5% of all breast neoplasms. Very few cases are reported in pregnancy [6,7]. Giant tumours are those more than 10 cm in diameter and more than 500 gm in weight. They account for nearly 20% of all phyllodes tumours [8].
Phyllodes tumour usually presents with a clinically benign swelling that may grow rapidly. Association of these tumours in pregnancy and lactation is unusual and a very few cases are reported in the literature [9]. Overlying skin is stretched, bluish discoloration and dilated veins are seen clinically. Axillary lymphadenopathy is usually not present even in large tumours [10,11]. Such tumours are not reported elsewhere in the body. Few cases are reported with similar histopathology in vulvar region most possibly from the ectopic mammary tissue. Depending upon the degree of stromal growth, stromal cellularity, cellular atypia and the nature of tumour borders, phyllodes tumours are classified as benign, borderline and malignant [12,13].
Wide excision with 1 cm margin is commonly recommended [14]. Simple mastectomy is indicated in large lesions involving most of the breast tissue [15,16].
Conclusion
It was very difficult for histopathologists to differentiate benign phyllodes tumour from giant fibroadenoma because of associated pregnancy and lactational changes in the mammary tissue, so careful inspection is needed while making a diagnosis.
[1]. Chaney AW, Pollack A, Mcneese MD, Zagars G K, Pisters PWT, Pollock RE, Primary treatment of cystosarcoma phyllodes of the breastCancer 2000 89:1502-11. [Google Scholar]
[2]. Calhoun K, Lawton TJ, Kim JN, Lehman CD, Anderson BO, In: Diseases of Breast, Harris J, Lippman ME, Osborne CK, Morrow M(Eds) 2010 4th edLippincott Williams & WilkinsChapter 65, p 781 [Google Scholar]
[3]. Murthy SS, Raju KVVN, Nair HG, Phyllodes tumour in lactating breastClinical Medicine Insights: Pathology 2016 9:13-17. [Google Scholar]
[4]. Islam S, Shah J, Harnarayan P, Naraynsingh V, The largest and neglected giant phyllodes tumor of the breast—a case report and literature reviewInt J Surg Case Rep 2016 26:96-100. [Google Scholar]
[5]. Rosen PP, Oberman HA, Tumours of the mammary gland 1993 Washington, DCArmed Forces Institute of Pathology:107-13. [Google Scholar]
[6]. Likhitmaskul T, Asanprakit W, Charoenthammaraksa S, Lohsiriwat V, Supaporn S, Vassanasiri W, Giant benign phyllodes tumour with lactating changes in pregnancy: a case reportGland Surg 2015 4(4):339-43. [Google Scholar]
[7]. Rowell MD, Perry RR, Hsiu JG, Barranco SC, Phyllodes tumoursAm J Surg 1993 165(3):376-79. [Google Scholar]
[8]. Aranda C, Sotelo M, Torres A, Zarate M, Phyllodes tumour and pregnancy. A report of a caseGinecol Obstet Mex 2005 73:387-92. [Google Scholar]
[9]. Liang MI, Ramaswamy B, Patterson CC, McKelvey MT, Gordillo G, Nuovo GJ, Giant breast tumours: Surgical management of phyllodes tumours, potential for reconstructive surgery and a review of literatureWorld J Surg Oncol 2008 6:117 [Google Scholar]
[10]. Calhoun KE, Allison KH, Kim JN, Rahbar H, Anderson BO, Phyllodes tumours. In J Harris, ME. Lippman, M Morrow, & CK. Osborne (Eds.)Diseases of the breast 2014 5th edition:826-837. [Google Scholar]
[11]. Vorherr H, Vorherr UF, Kutvirt DM, Key CR, Cystosarcomaphyllodes: epidemiology, pathohistology, pathobiology, diagnosis, therapy, and survival [review]Arch Gynecol 1985 236(3):173-81. [Google Scholar]
[12]. Telli ML, Horst KC, Guardino AE, Dirbas FM, Carlson RW, Phyllodes tumours of the breast: natural history, diagnosis, and treatmentJ Natl Compr Canc Netw 2007 5:324-30. [Google Scholar]
[13]. Blaker KM, Sahoo S, Schweichler MR, Chagpar AB, Malignant phyllodes tumour in pregnancyAm Surg 2010 76:302 [Google Scholar]
[14]. Lenhard MS, Kahlert S, Himsl I, Ditsch N, Untch M, Bauerfeind I, Phyllodestumour of the breast: clinical follow-up of 33 cases of this rare diseaseEur J Obstet Gynecol Reprod Biol 2008 138:217-21. [Google Scholar]
[15]. Salvadori B, Cusumano F, Del Bo R, Delledonne V, Grassi M, Rovini D, Surgical treatment of phyllodestumours of the breastCancer 1989 63:2532-36. [Google Scholar]
[16]. Ben Hassouna J, Damak T, Gamoudi A, Chargui R, Khomsi F, Mahjoub S, Phyllodes tumors of the breast: a case series of 106 patientsAm J Surg 2006 192(2):141-47. [Google Scholar]