Menorrhagia is a common problem in women of reproductive age group and 5% of women between 30 and 49 years of age group consult their general practitioner for this problem [1,2]. The aetiology can be local or systemic disorders but a specific cause is identified in less than 50% of the cases and in remaining cases dysfunctional uterine bleeding is diagnosed [2].
Menorrhagia occurring in adolescent age group and perimenopausal age group is chiefly due to anovulatory cycles. In perimenopausal age group, local pathology like leiomyomas can also contribute to menorrhagia [3].
Recently, bleeding disorders like von Willebrand Disease, single coagulation factor deficiencies particularly factor XI, VIII, Factor V and platelet function disorders have been found to be prevalent in patients presenting with menorrhagia [1,3-6].
The present study was taken up with an aim to assess the type and frequency of haemostatic disorders in adolescent, post adolescent and perimenopausal women presenting with unexplained menor-rhagia.
Materials and Methods
This was a prospective study of one year duration. It was carried out in Department of Pathology in collaboration with Department of Obstetric and Gynaecology, King George’s Medical University, Lucknow, India. The study population included women in age group 13 years to 55 years attending gynaecology unit with complaints of menorrhagia. A written informed consent was taken from all the patients. Women with endocrine disorders like thyroid disease, pelvic pathology like uterine leiomyomas, uterine polyps, gynaecological malignancy, intrauterine device were excluded from the study. Also, the women who had history of oral contraceptive pill use in previous one cycle, non-steroidal anti-inflammatory drugs, aspirin or use of drugs interfering with platelet functions in previous two weeks were excluded.
Detailed history was taken from all the patients including age at menarche, family history of bleeding disorder, easy bruising, nasal bleed, joint bleed, excessive bleeding after minor injury.
The selected patients provided a written informed consent and completed a Pictorial Blood Loss Assessment Chart (PBLAC) which is a semi quantitative test to determine the average blood loss during menstrual period [7]. Age matched women with normal menstrual history were taken as control.
Citrated blood sample was collected by venous puncture, both from cases and controls. The collected blood samples (9 part) was added to one part of 0.11 M trisodium citrate in polystyrene graduated tubes. Platelet poor or platelet rich plasma as per requirement for testing, were made according to standard protocol [8].
The screening investigations included complete blood count including platelet count and platelet morphology, measurement of Bleeding Time (BT) according to Modified Ivy’s method, Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT), Thrombin Time (TT) assay. These tests were done manually; PT was done using Thromboplastin reagent, aPTT was done using kaolin phospholipid solution and TT was done using thrombin reagent.
Specific factor analysis was done as and when required. Factor V, VII, VIII, IX, X, XI and XII were measured by specific factor deficient plasma on an automated analyser (Tulip Haemostar). von Willebrand factor antigen (vWF:Ag) was done by Enzyme Linked Immunosorbent Assay (ELISA). This facility is not available at our centre hence it was done from outside source.
Platelet aggregation tests using Adinosine Diphosphate (ADP) and Ristocetin was done in Chrono-log 4 channel optical lumi aggregometer.
Statistical Analysis
Statistical analysis was carried out using SPSS 16.0 version (Chicago, Inc., USA). The results are presented in mean±SD and percentages. The Chi-square test was used to compare dichotomous/categorical variables. The continuous parameters were compared by using one way analysis of variance (ANOVA) followed by Tukey’s multiple comparison tests among the groups. The unpaired t-test was used to compare the continuous variables between the groups. The p-value<0.05 was considered significant.
Institutional ethical clearance was obtained for this study.
Results
In time duration of one year 1100 women came to gynaecological emergency with complaints of menorrhagia. Out of them 104 women were included in the study after ruling out organic/hormonal causes.
Age of patients ranged from 13 years to 46 years. Mean age of patients was 26.2±8.6 years. More than one third of the patients were in the age group 20-30 years (46.2%) followed by less than 20 years (26.9%), 31-40 years (20.2%) and more than 40 years (6.7%).
The mean menarche age of patients was 11.6±0.86 years. Eighteen patients had menorrhagia since menarche. Seven patients had family history of abnormal bleeding.
Mean haemoglobin concentration and mean of Mean Corpuscular Volume (MCV) were 9.34±2.38 gm/dL and 80.20±11.29 fL respectively. Mild anaemia (haemoglobin concentration 10-12 gm/dL) was seen in 66.3% (n=69) patients, moderate anaemia (haemoglobin concentration 8-10 gm/dL) was seen in 22.3% (n=24) and severe anaemia (haemoglobin concentration less than 8 gm/dL) was seen in 10.6% (n=11) patients.
Iron deficiency anaemia was noted in 37.5% (n=39) patients, macrocytic anaemia was seen in 4.8% (n=5) patients.
The PBLAC score was more than 100 in all the 104 patients. In 64 (61.5%) patients the average duration of flow exceeded seven days. Eighty two patients (78.8%) gave history of passage of large sized blood clots and 61 (58.7%) gave history of episodes of flooding.
Out of 104 patients, 32 patients gave history of other bleeding tendencies associated with menorrhagia [Table/Fig-1]. Of these, epistaxis was most common followed by gum bleeding and excessive bleed from wound.
Other bleeding manifestations.
| Types of bleeding | Number of patients (n=32) | Percentage of total patients with bleeding tendencies (%) |
|---|
| Epistaxis | 15 | 46.9 |
| Gum Bleeding | 5 | 15.6 |
| Easy bruising | 1 | 3.1 |
| Purpura | 4 | 12.5 |
| Wound bleeding | 5 | 15.6 |
| Prolonged bleeding after tooth extraction | 1 | 3.1 |
| Ileo psoas abscess | 1 | 3.1 |
BT, PT, aPTT, TT and platelet counts of all the patients were done. [Table/Fig-2] shows the results of these screening tests.
Distribution of patients based on abnormal screening tests.
| Tests | Number | (%) |
|---|
| BT (Prolonged) | 23 | 22.1 |
| PT (Prolonged) | 2 | 1.92 |
| APTT (Prolonged) | 10 | 9.6 |
| Platelet count (<1lac) | 5 | 4.8 |
Based on the screening tests 81 patients were excluded from the study and 23 patients with systemic bleeding aetiology were subjected to further confirmatory tests. [Table/Fig-3] shows the distribution of various bleeding disorders in patients presenting with menorrhagia.
Distribution of the patients according to definitive diagnosis.
| Diagnosis | Number of patients (n=23) | Percentage (%) |
|---|
| vWD | 10 | 43.4 |
| ITP | 5 | 21.7 |
| Glanzmanns | 7 | 30.4 |
| BS | 1 | 4.3 |
(vWD – Von Willebrands Disease; ITP- immune thrombocytopenic purpura; I BS-Bernard- Soulier syndrome)
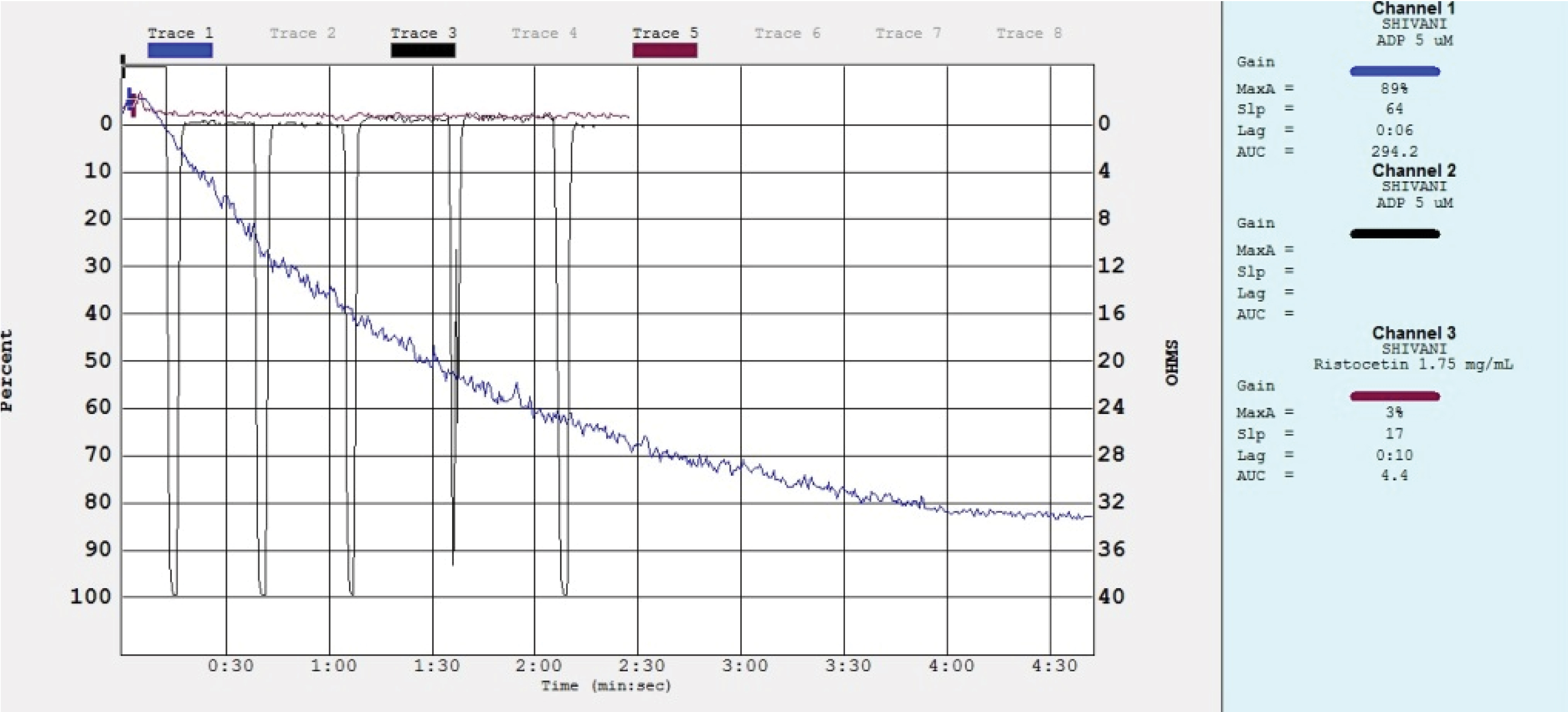
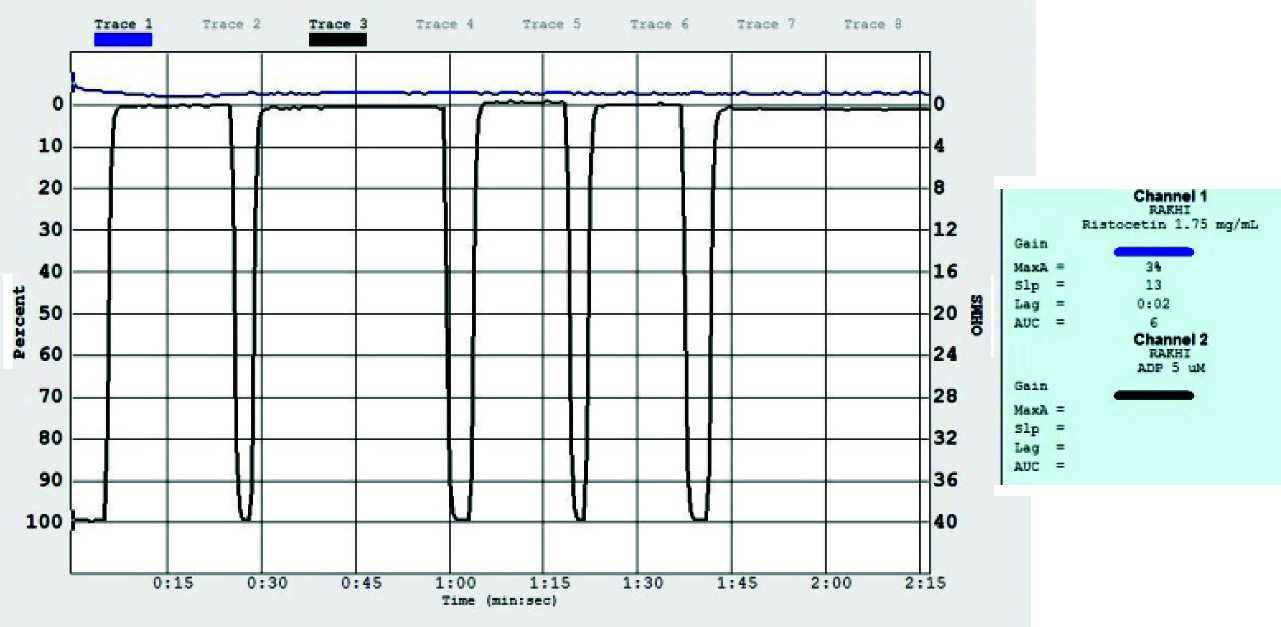
vWD was diagnosed in 10 patients. Eighty percent of these patients gave history of puberty onset menorrhagia. The mean value of haemoglobin in these patients was 6.9 gm/dL. Mean of the MCV was 68 fL. Platelets were adequate in number and normal in size. Nine patients had prolonged bleeding time. Average clot retraction at the end of one hour was 37.6%. aPTT was prolonged in all of these patients and showed full correction on mixing with factor IX deficient plasma. There was no correction with FVIII deficient plasma indicating deficiency of FVIIIc. Average vWF:Ag was 48.8 IU/dl. Aggregation studies showed normal aggregation curve with 5 µm ADP and reduced aggregation with 1.25 mg/ml ristocetin in nine patients, one patient showed absent platelet aggregation with ristocetin [Table/Fig-4].
Platelet aggregation studies in vWD showing normal aggregation with ADP (5 µm) and absent aggregation with ristocetin (1.25 mg/ml).
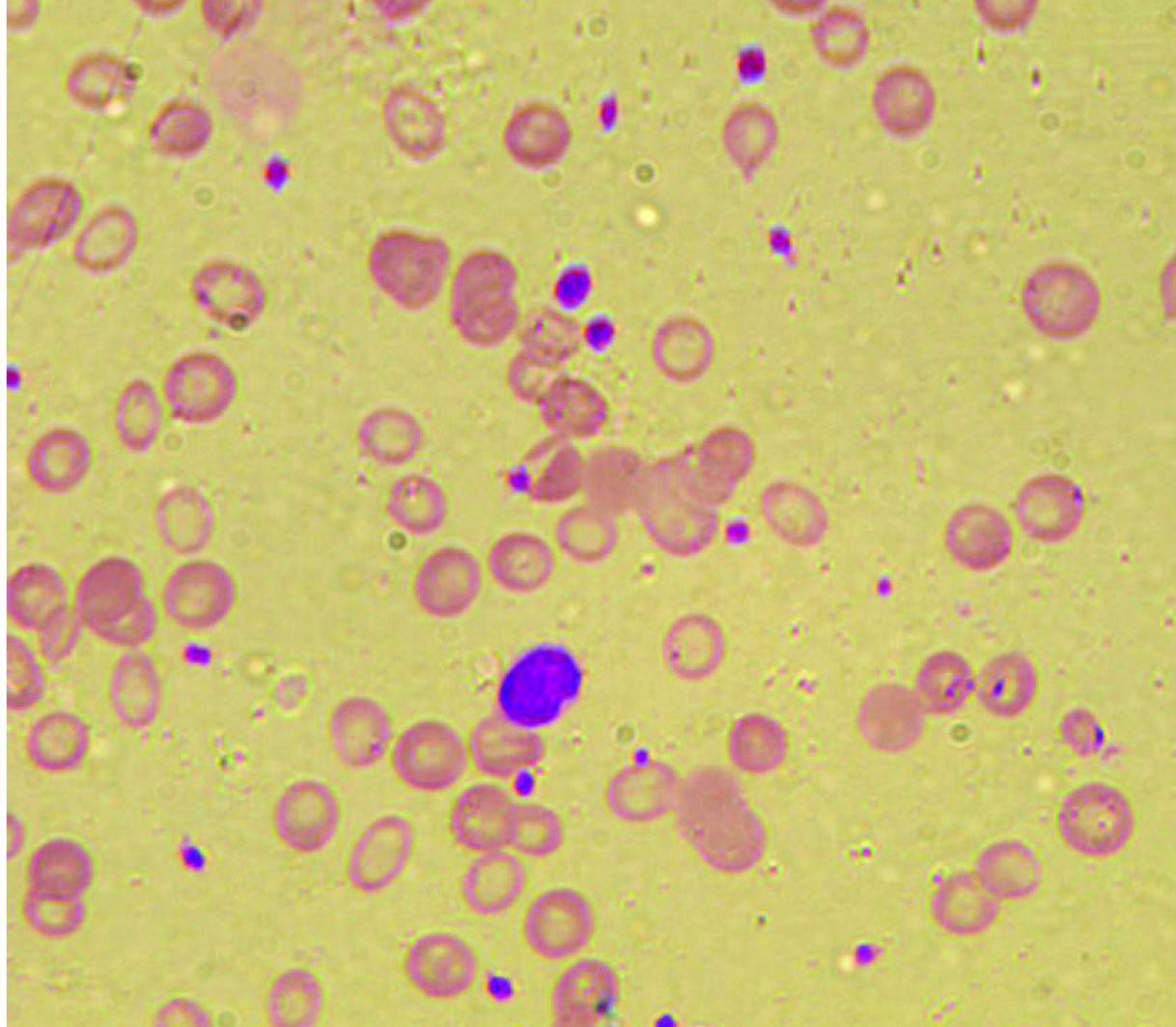
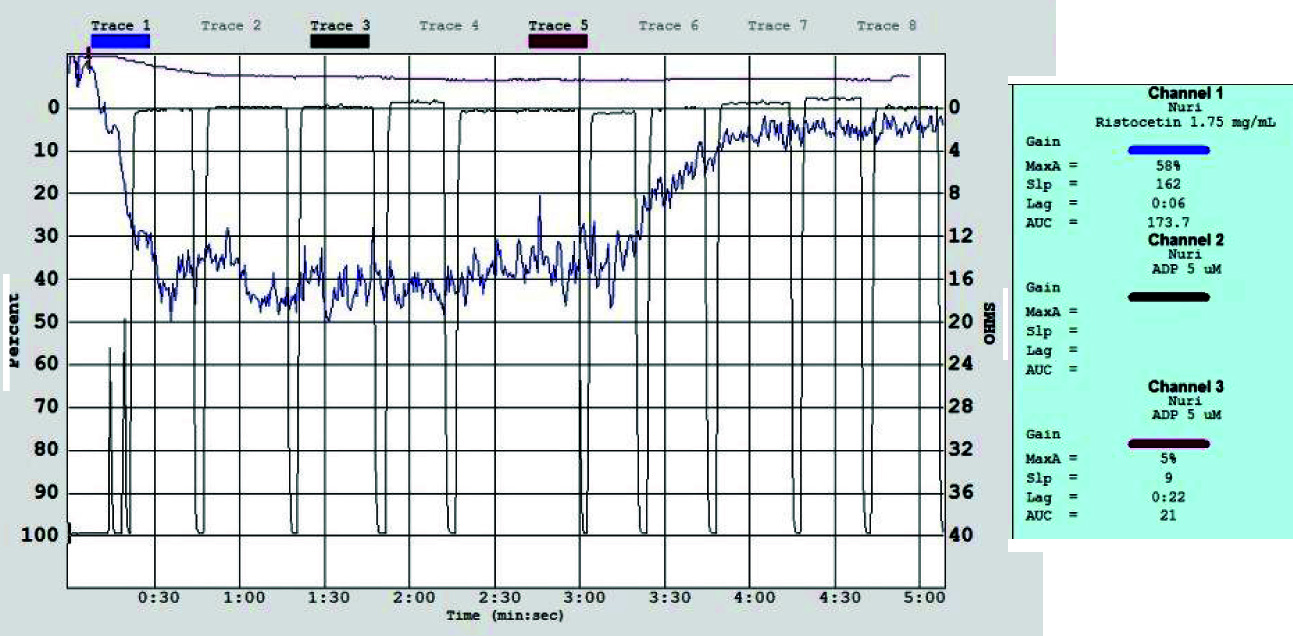
Glanzmann Thrombasthenia was the second most common haemostatic abnormality detected in our study group. Total of seven patients were diagnosed. Mean age of presentation was 19 years. Most of these patients presented with history of epistaxis. Mean PBLAC score was 341. Platelets were normal in number but peripheral smears made by fresh finger prick did not show any satisfactory platelet clumps [Table/Fig-5a]. Screening investigations revealed prolonged bleeding time and reduced clot retraction at the end of one hour. Aggregation studies revealed absent aggregation with 5 µm ADP and normal aggregation with 1.25 mg/ml ristocetin [Table/Fig-5b].
Peripheral blood smears made by finger prick from a patient with Glanzmanns disease showing absent platelet aggregation (Leishman stain 10X).
Platelet aggregation studies in patient with Glanzmanns disease showing absent aggregation with ADP (5 µm) and normal aggregation with ristocetin (1.25 mg/ml).
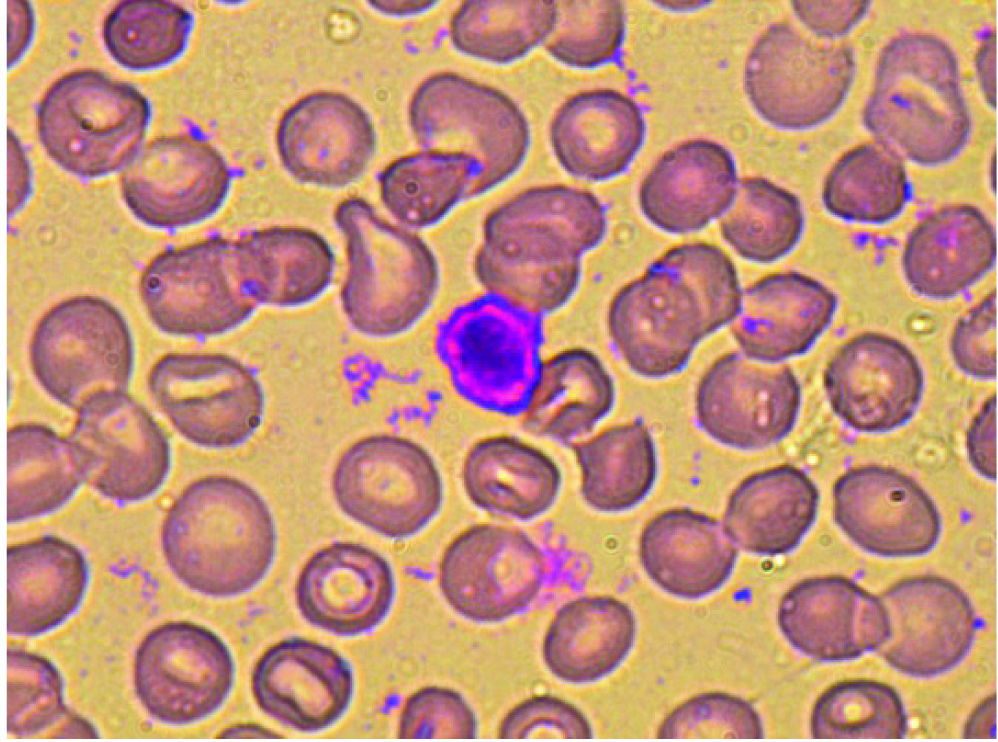
In our study group, one patient was diagnosed as Bernard-Soulier syndrome. She was 14 years, with history of puberty onset menorrhagia and mean PBLAC score of 172. Her haemoglobin was 8 gm/dL. Mean Platelet Volume (MPV) and Platelet Distribution Width (PDW) were raised. She had history of epistaxis since childhood. Screening investigations revealed a normal platelet count. Peripheral blood smear made from fresh finger prick showed presence of large sized platelets almost equal to size of RBC’s [Table/Fig-6a]. Bleeding time and APTT were in normal range. Aggregation studies with 1.25 mg/ml ristocetin showed reduced aggregation [Table/Fig-6b].
Freshly prepared peripheral blood smear showing “giant platelet”. (Leishman stain 100X).
Platelet aggregation in Bernard Souliers showing defective aggregation with ristocetin (1.25 mg/ml).
In our study group, we got five patients of immune thrombocytopenic purpura, presenting with menorrhagia. In these cases bone marrow aspiration showed increased number of non-functional megakaryocytes.
On comparing the parameters between two study groups i.e., patients with haemostatic defect and patients without haemostatic defect, we found a significant difference between haemoglobin levels, aPTT, PBLAC score, clot retraction, number of bleeding days and history of flooding [Table/Fig-7].
Haematological parameters between patients with and without well-established coexisting haemostatic defects
| Characteristics | Patients with haemostatic defect(n=23) | Patients without haemostatic defect (n=81) | p-value |
|---|
| Hb (gm/dl) | 7.92±2.34 | 9.78±2.13 | 0.001* |
| MCV | 79.18±12.16 | 81.71±11.30 | 0.52 |
| APTT | 37.29±11.64 | 26.35±2.32 | 0.001* |
| BT | 4.81±2.11 | 4.65±1.71 | 0.69 |
| PBLAC score | 276.52±122.02 | 147.81±55.91 | 0.001* |
| Aggregation ADP Ristocetin | 55.87±22.51 36.01±7.02 | 61.21±12.01 42.32±21.32 | 0.13 0.46 |
| Clot retraction (at end of one hour) | 43.81±11.10 | 64.01±11.34 | 0.001* |
| No. of bleeding days | 9.33±2.36 | 6.45±1.83 | 0.001* |
| Passage of clots+ | 19 | 63 | 0.61 |
| History of flooding+ | 21 | 40 | 0.001* |
indicates statistically significant.
(Hb- Haemoglobin; MCV- Mean Corpuscular Volume; aPTT-Activated Partial Thromboplastin Time; PBLAC-Pictorial Blood Loss Assessment Chart; BT- Bleeding Time; CR- Clot retraction)
Discussion
This study was an effort to characterize systemic haemostatic disorders in menorrhagic females presenting to gynaecological emergencies.
Bleeding disorders are frequent cause of menorrhagia in women from puberty age group to perimenopausal age group [3]. As per guidelines recommended by American College of Obstetricians and Gynecologists (ACOG), all the females presenting with menorrhagia should be screened for bleeding disorders [9]. Our study shows that 22% females had bleeding disorders.
Bleeding disorders could be the major cause of menorrhagia in adolescents [10]. In our study, mean age of patient diagnosed as vWD was 18 years, Glanzmann thrombasthenia was 19 years and Bernard – Soulier syndrome was 14 years, this is consistent with the data from literature [3].
Because there are no objective methods to measure the menstrual blood loss accurately we tried to correlate it with PBLAC. The PBLAC with a score of more than 100 is taken as equivalent to menstrual blood loss of more than 80 ml. The mean PBLAC score was significantly high in patients with haemostatic defect as compared to patients without haemostatic defect [Table/Fig-7]. These results matched the results found in studies of Shankar M et al., Philipp CS et al., Hutspardol S et al., [2,3,11].
In 61.5% of the menorrhagic patients the duration of menstrual bleeding was prolonged beyond a normal range of two to seven days and a history of passage of blood clots and flooding were also present. Number of bleeding days was significantly increased in patients with haemostatic defect as compared to patients without haemostatic defect [Table/Fig-7]. This inference is in accordance with the study of Edlund M et al., Claire S. Philipp et al., [12,13].
As reported by Kadir RA et al., a significant number of patients suspected of having systemic inherited or acquired bleeding disorder had a history of other associated bleeding tendencies most commonly mucosal bleeds like epistaxis (53.65%) and gum bleeding (17.9%) [1].
Prevalence of menorrhagia in vWD is 5%-36% [14]. In our study total of 10 patients were diagnosed to have vWD that constitutes 9.6% of all patients screened and 43.4% of those in which a specific diagnosis could be obtained. These patients presented with history of puberty onset menorrhagia, epistaxis, gum bleeding and prolonged bleeding from wounds and dental extraction. One patient also gave history of ileopsoas abscess. These are consistent with the data reported by Dilley A et al., and Lusher JM et al., [15,16]. Out of 10 cases seven patients had O blood group, three were non O groups. Our results are in concordance with Shankar M et al. This is because of decreased levels of von Willebrand factor antigen levels and von Willebrand factor functional activity in blood group O [2]. Almost 25% lower vWF antigenic level is noted in patients with blood group O compared to patients with other blood types [17]. Diagnosis of mild forms of vWD is difficult. Patients with vWF:Ag level of 30-50 IU/dL may need appropriate treatment to increase the levels during child birth or any other invasive procedure. Hence, it is important to correlate the cause and severity of bleeding with laboratory results [18].
As suggected by literature, 51% patients of Bernard Souliers syndrome and 13%-98% patients of Glanzmanns thrombasthenia present with menorrhagia. These patients usually present with severe nose and gum bleed [18]. Platelet function defect was found in eight patients in our study. Seven patients had Glanzmann-thrombasthenia and one patient had Bernard- Soulier syndrome. These patients had history of various mucocutaneous bleeding in addition to early onset menorrhagia. Hutspardol S et al., reported six cases of inherited bleeding disorder in their study. Three cases were of vWD, two of Glanzmann-thrombasthenia and one of Bernard-Soulier syndrome [11]. Whereas, Philipp CS et al., reported platelet function disorder to be more common cause of menorrhagia than vWD [3].
In our study, we came across five cases of immune thrombocytopenic purpura. In these cases diagnosis was confirmed on bone marrow aspirate which showed increased non functional megakaryocytes.
Limitation
This was a pilot study of one year duration. So the sample size was less. If this study is conducted for a long duration then we may get the accurate prevalence of bleeding disorder in women presenting with menorrhagia.
Conclusion
Our results demonstrate that undiagnosed haemostatic disorders are frequent cause of unexplained menorrhagia in significant number of women from adolescent age group to perimenopausal age.
Therefore, we suggest that after excluding pelvic pathology or any other underlying hormonal cause all women presenting with menorrhagia should be screened for haemostatic disorders.
Our study also emphasises on meticulous history taking, as a long history of menorrhagia, puberty onset menorrhagia, history of repeated epistaxis, mucocutaneous bleeding, bleeding after surgical procedures or tooth extraction suggest an underlying bleeding diathesis in these patients.
Women suspected of bleeding disorders should be offered appropriate diagnostic evaluation and counselling before attaining menarche and before planning pregnancy to prevent complications due to bleeding. Combined effort of a haemostasis expert and obstetrician is need of the hour.
(vWD – Von Willebrands Disease; ITP- immune thrombocytopenic purpura; I BS-Bernard- Soulier syndrome)
*indicates statistically significant.
(Hb- Haemoglobin; MCV- Mean Corpuscular Volume; aPTT-Activated Partial Thromboplastin Time; PBLAC-Pictorial Blood Loss Assessment Chart; BT- Bleeding Time; CR- Clot retraction)