A Case Report of Rare Carcinoma Ex Pleomorphic Adenoma of Submandibular Gland and its Detailed Description
Kirti Balkrishna Buva1, Ajinkya Amritrao Deshmukh2, Atul A. Deshmukh3
1 Assistant Professor, Department of Oral Pathology, Bharati Vidyapeeth Deemed University, Dental College and Hospital, Navi Mumbai, Maharashtra, India.
2 Post Graduate Student, Department of Oral Pathology, Bharati Vidyapeeth Deemed University, Dental College and Hospital, Pune, Maharashtra, India.
3 Director, Department of Oral and Maxilofacial Pathology, Center for Interdisciplinary Research, D.Y. Patil University, Nerul, Navi Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kirti Balkrishna Buva, Assistant Professor, Department of Oral Pathology, Bharati Vidyapeeth Deemed University, Dental College and Hospital, Navi Mumbai-400614, Maharashtra, India.
E-mail: drkirtibuva@gmail.com
A 65-year-old female patient reported with a chief complaint of swelling in the left lower region of the jaw since two years. On clinical examination, the swelling was present on the mandibular left posterior region and measuring approximately 6.2 cm antero-posteriorly × 6.2 cm mediolaterally × 8.7 cm superioinferiorly. Initially, it was non tender but eventually it became tender. Fine needle aspiration was done to rule out any salivary gland pathology and report obtained was carcinoma ex pleomorphic adenoma. Then, excisional biopsy was taken and tissue sent for histopathology. Histopathological diagnosis was benign adenoma with carcinoma. Later serial sections of tissue were studied and came to the conclusion of carcinoma ex pleomorphic adenoma which was non invasive type and showed bizarre cells with neoplastic changes. Benign part was composed of myxomatous area with partial capsule. Neoplastic cells showed invasion into capsule and few necrotic areas were also present. Overall interpretation was favoured Non invasive carcinoma ex pleomorphic adenoma. So here, we reported a case of Carcinoma ex Pleomorphic Adenoma (CAEXPA) which is a deadly and rare variant of salivary gland malignancy.
Mandible, Mixed tumour, Non invasive, Salivary gland malignancy
Case Report
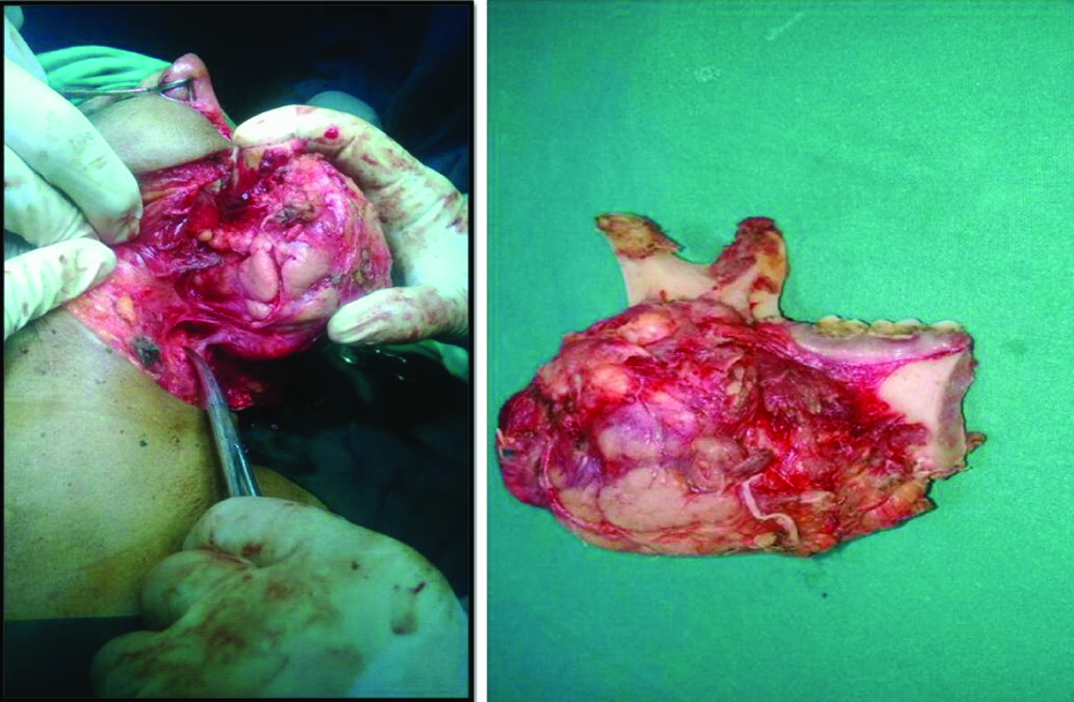
A 65-year-old female patient reported with a complaint of swelling on the left side of the face which is increasing in size. It was peanut size earlier but grew to the present size in 2-3 months. Extra oral examination revealed soft and fluctuant swelling on left side of the face. Extra orally it was approximately 6.2 cm anteroposteriorly × 6.2 cm mediolaterally × 8.7 cm superioinferiorly, extending superiorly from pinna of the ear to 2.5 cm below the lower border of the mandible and anteroposteriorly from pinna of the ear to 6.2 cm anteriorly. Swelling was firm and the overlying skin was normal. No elevation of temperature at the affected site and no pus discharge were seen [Table/Fig-1]. No intra oral findings were seen.
a) Intra operative view; b) Gross specimen.
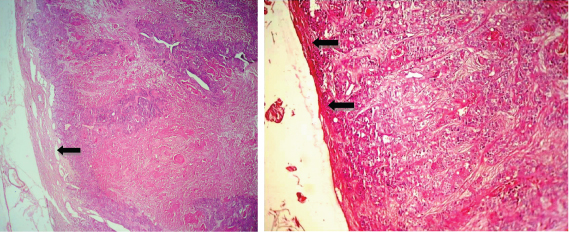
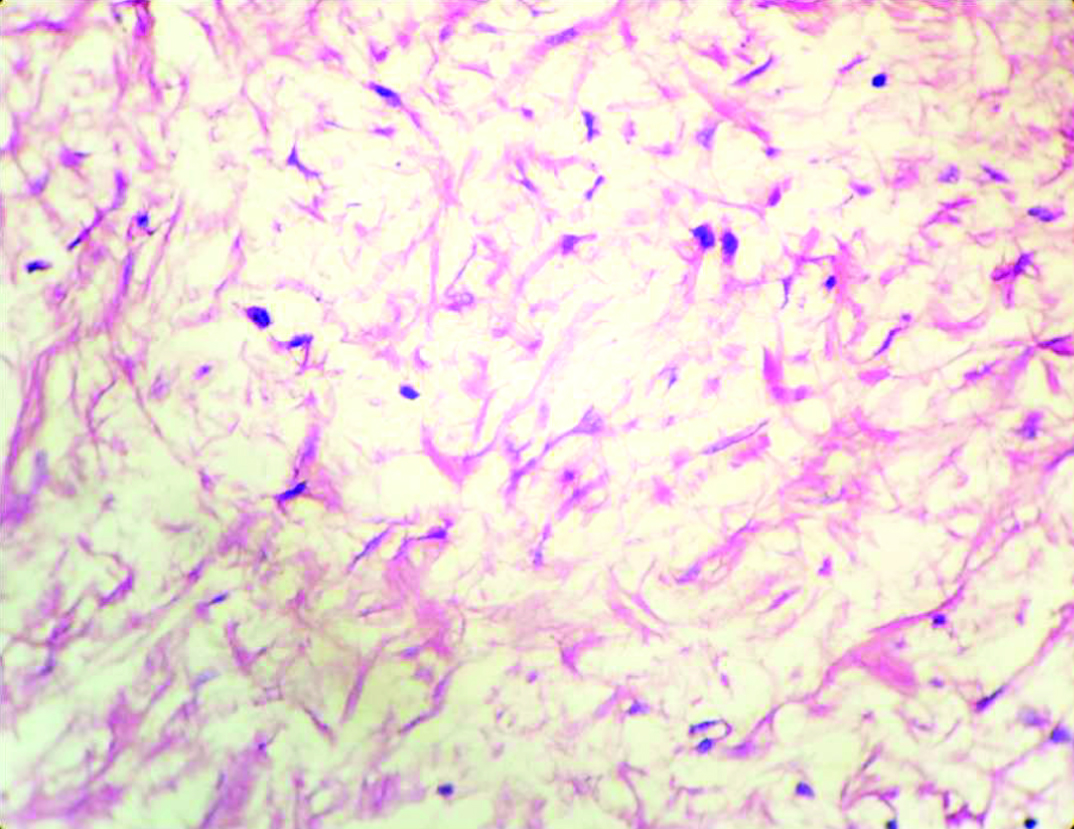
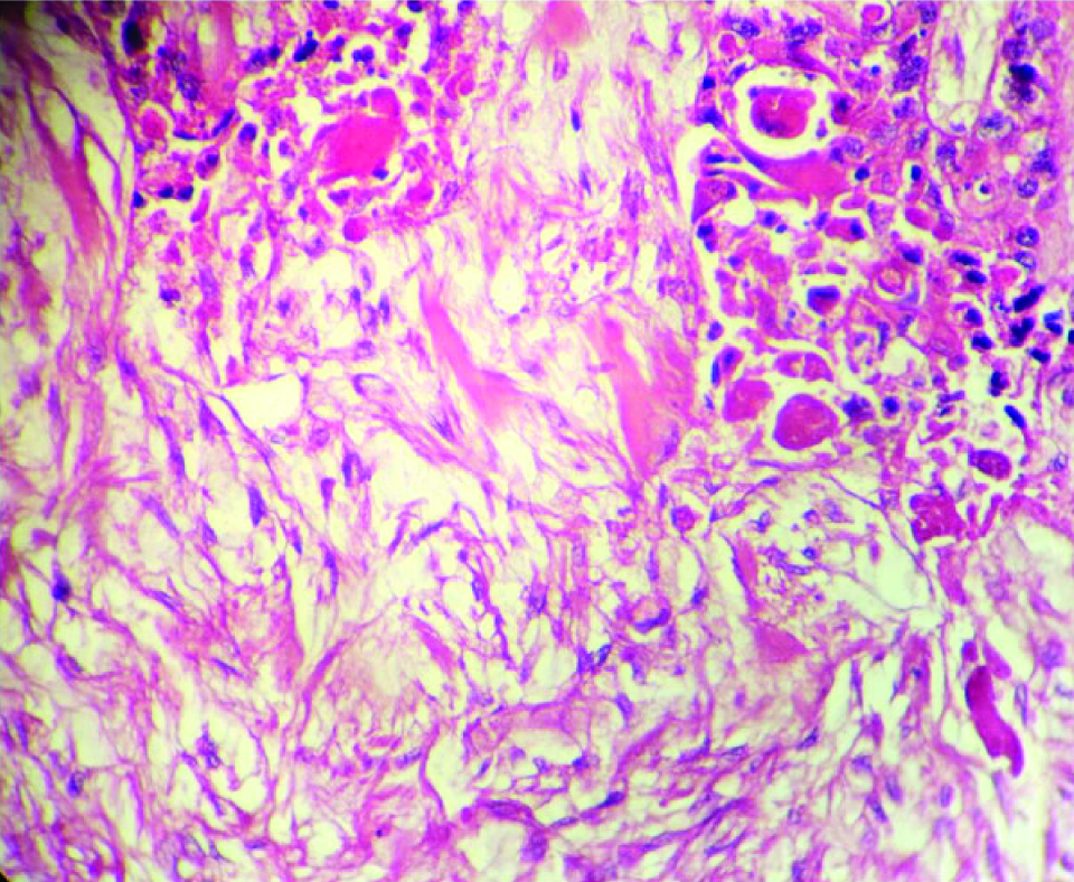
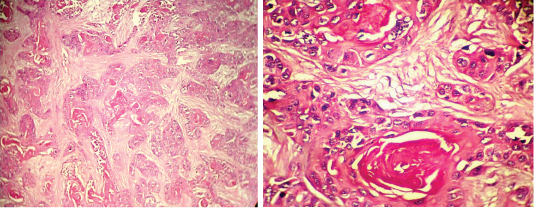
Fine Needle Aspiration Cytology (FNAC) was carried out and the report was CAEXPA. The whole lesion was excised and sent to histopathology laboratory. The histopathology report showed epithelium and connective tissue surrounded by a capsule. The capsule was composed of fibers interspersed with fibroblasts. The epithelium was arranged in the form of ducts, cords and sheets. The epithelial island was composed of squamous cells and many keratin pearls. Epithelium was dysplastic. Individual squamous cell showed increased nuclear cytoplasmic ratio, hyperchromatism, mitotic figures and pleomorphism of cell. Thick collagen bundles were seen. Abundant hyalinization of collagen fibers was seen. At many areas myxoid tissue was evident. Homogenous eosinophilic coagulum was also noted [Table/Fig-2,3,4,5,6 and 7].
a) In 4X magnification, arrow is suggestive of fibrous capsule; b) In 10X magnification, arrow shows nests of neoplastic cells infiltrating into the capsule.
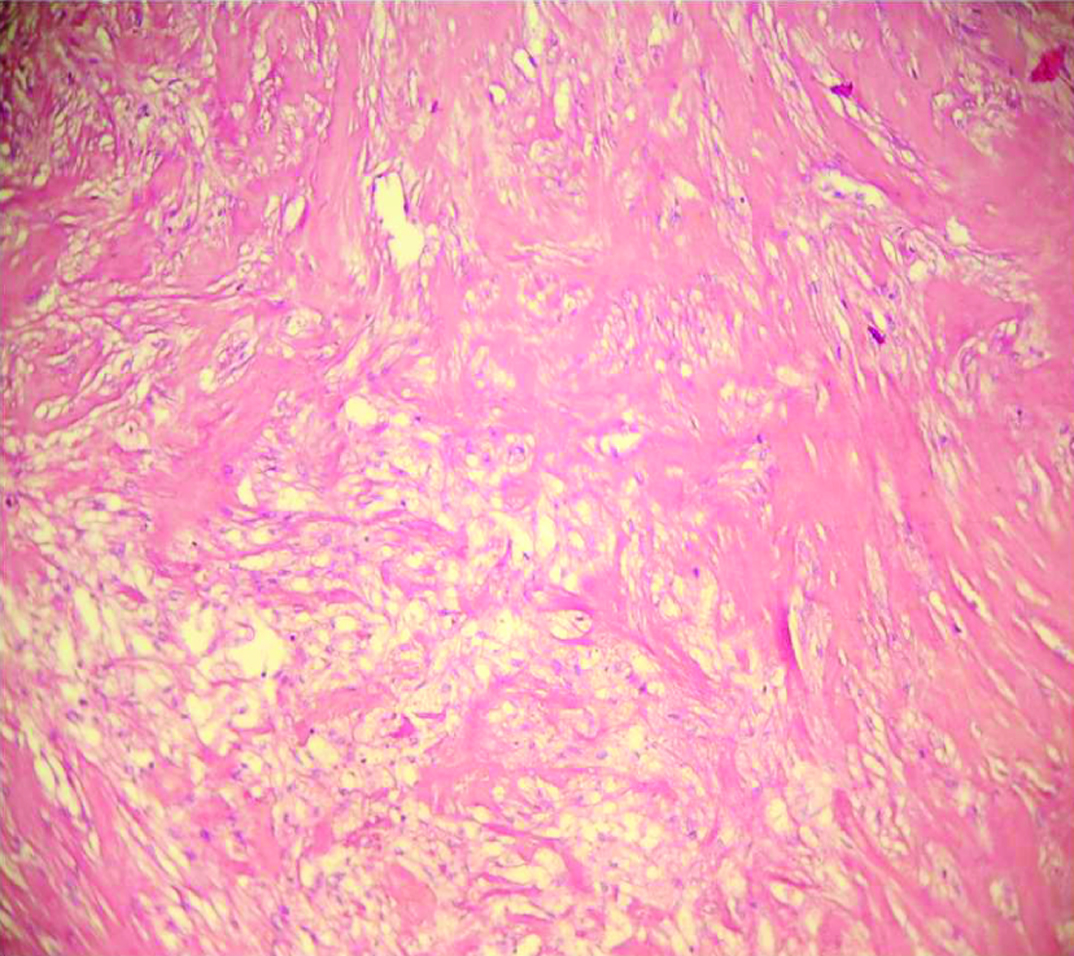
A 40X magnification showing myxoid tissue showing star shape cells mingling into the sparse connective tissue stroma.
A 40X magnification showing foci where benign and malignant part of same tumour representing mixed tumour.
A 10X magnification sowing dense hyalinization in connective tissue stroma.
a) A 4X magnification showing nests sheets and cord of anaplastic cells along with keratin pearl.
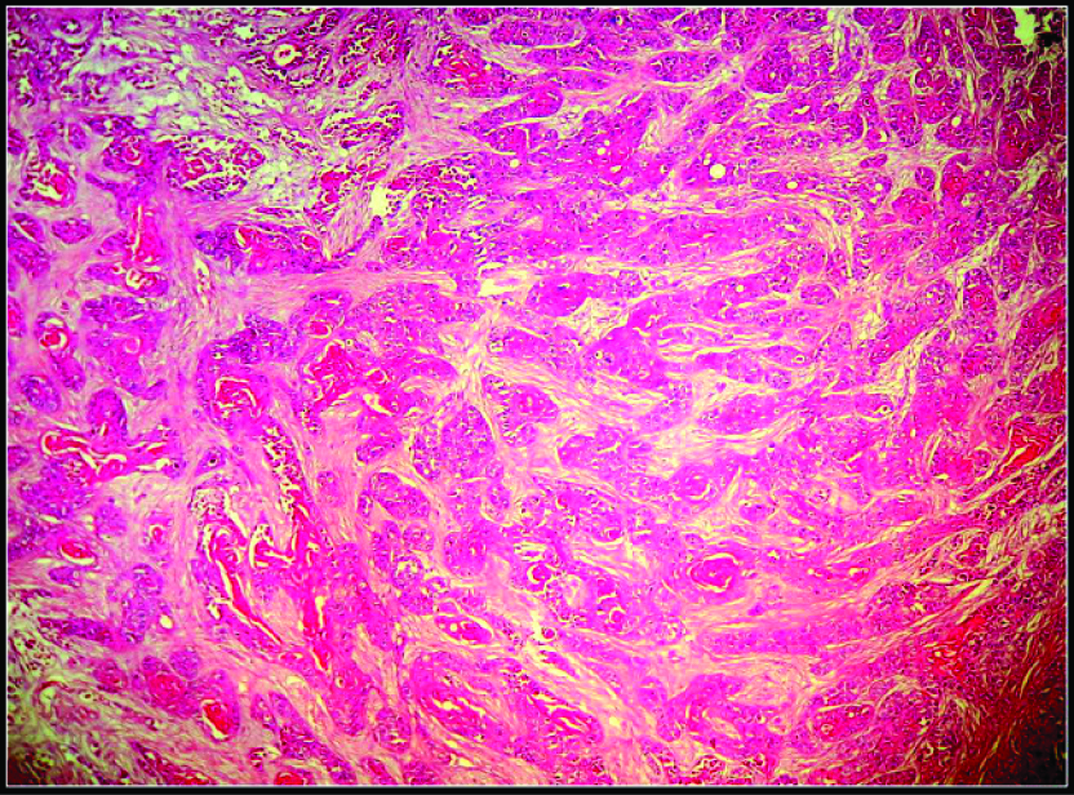
a) 10X magnification showing nests of squamous cells along with anaplastic changes and keratin pearls; b) 40X magnification showing Keratin Pearl.
The overall picture was suggestive of –
“Noninvasive Carcinoma ex Pleomorphic Adenoma”.
Discussion
CAEXPA is also known as carcinoma ex mixed tumour or pleomorphic adenoma, carcinoma in a mixed tumour or carcinoma arising from a mixed tumour and metastasizing pleomorphic adenoma [1,2]. CAEXPA is defined as a pleomorphic adenoma in which an epithelial malignancy is present [3]. In most of the cases of CAEXPA epithelial malignancy seen is adenocarcinoma (not otherwise specified) but other malignancy such as mucoepidermoid carcinoma, squamous cell carcinoma, adenosquamous cell carcinoma, Adenoid cystic carcinoma, epithelial myoepithelial carcinoma, sarcomatoid carcinoma, acinic cell carcinoma, clear cell carcinoma and myoepithelial carcinoma are also reported [4-6]. Malignant transformation may occur in a sequence manifested as:
Carcinoma in situ: In first phase carcinoma cells are replaced by the ductal luminal cells. Here Myoepithelial cell layer is intact, nonatypical and neoplastic in nature.
Intracapsular carcinoma/Noninvasive: Connective tissue invasion develops on further progression of the carcinoma but without breach of fibrous capsule of the former pleomorphic adenoma.
Invasive carcinoma: Extracapsular invasion is seen.
Microinvasive carcinoma: Extracapsular invasion is less than 5 mm.
Frank invasive carcinoma: Extracapsular invasion is beyond 5 mm [7,8].
The noninvasive carcinoma ex pleomorphic adenoma was introduced in 1977 by Livolsi V and Perzin K [9]. The concept of malignant tumour arising in mixed tumour that is Mixed Malignant Tumour (MMT) was developed by Livolsi and Perzin in 1977 [9] and it is supported by Spiro et al., but with the remark that there must be a possible de novo origin in cases where clinical history is missing or histological indications show preexisting salivary gland tumour [9].
CAEXPA accounts for 3.6% of all salivary tumours, 12% of all salivary malignancy, and 6.2% of all pleomorphic adenoma [3]. Most commonly CAEXPA is seen in parotid gland but sometimes it can be seen in submandibular gland, minor salivary glands and palate. CAEXPA shows a predilection for females than males. CAEXPA rarely seen below the age of 20 and commonly seen in sixth to seventh decade of life [3,5]. There are two clinical forms which are mentioned according to the function of time, first where the patient with benign mixed tumour consisting considerable period of time because of recurrence or no treatment, the second type with smaller number of patients without prior sequence. The second type shows the presence of carcinoma during its first surgical removal and a short history of less than one year. A case presented here shows the features of the second type [5].
Invasive CAEXPA shows uncircumscribed infiltrative margins. Malignant part shows variations of adenocarcinoma, squamous cell carcinoma or undifferentiated carcinoma. In poorly or undifferentiated carcinoma there is cellular and nuclear pleomorphism with prominent nucleoli, the difference in mitotic figures depends on the case. Infiltration of capsule till 8 mm shows a good prognosis. Necrosis, haemorrhagic areas and perineural and perivascular invasion are also seen. Whereas in non-invasive type tumour is circumscribed, the presence of benign part i.e., pleomorphic adenoma is rarely seen where repeated sectioning is needed. Cytological atypia is seen with increased cytoplasm, slight pleomorphism of nucleoli and prominent nucleoli is noted. Increased mitotic activity in atypical cells at the peripheral area or subcapsular area is seen. Luminal and nonluminal cells show irregular outline. An abundant amount of hyalinized stroma and acellular stroma is evident. Very little amount of myxoid area is observed. Generally carcinomatous part is adenocarcinoma with atypia and proliferation of atypical cells. Within capsule similar nodules of cells are seen. A mixture of cellular and acellular areas is seen in low foci. Calcification and ossification may also be seen sometimes [1].
So here is a case reported by us which is clinically second type with two year history and histologically non invasive carcinoma ex pleomorphic adenoma. This type of benign mixed tumours is rarely reported, so thorough knowledge of these lesions is needed [Table/Fig-8].
Cases reported and review of literature of non invasive carcinoma ex leomorphic adenoma in head and neck region.
| Author | Cases Reported |
|---|
| Brandwein M et al., [10] | Twelve cases reported. All were showing noninvasive or minimally invasive type of CAEXPA. Non invasive CAEXPA shows less malignant potential. Ploidy studies were done and those were not helpful in the prediction of tumour behaviour. After the follow up of 1.2 to 13 years, no recurrence or metastases was seen. |
| Lewis J et al., [11] | A pathologic analysis of 73 cases were done out of which only four were showing noninvasive type of CAEXPA. Prognostic factor of CAEXPA were analysed using immunostaining studies. Prognostic factors depend on tumour stage, grade and proportion of carcinoma, proliferation index and extent of invasion. Intracapsular cases were benign in nature. Noninvasive CAEXPA can be treated as common pleomorphic adenoma. |
| Felix A et al., [12] | A case of non invasive CAEXPA was reported in which ipsilateral cervical lymph nodes metastases were seen. P53 and c-erbB 2 was positive for malignant cells. The presence of metastases of malignant cells suggests tumour of a malignant in nature. |
| Di palma S et al., [13] | 11 cases of noninvasive CAEXPA was reported and studied for the HER-2/neu protein. Cells of noninvasive CAEXPA were positive for HER-2/neu and negative for maternal pleomorphic adenoma. They also stated HER-2/neu can be used as useful marker in the malignant transformation of pleomorphic adenoma. |
| Ethunandan M et al., [14] | Two cases were reported and rare feature was reported. Vascular invasion was seen in noninvasive CAEXPA. The connection between the benign vascular invasion and metastasizing pleomorphic adenoma is unknown. |
| Kunimura T et al., [15] | A case was reported, based on cases reported in past and the case mentioned in an article, a conclusion was drawn as the malignant transformation of pleomorphic adenoma through noninvasive CAEXPA reaches invasive CAEXPA. |
| Dandekar M et al., [16] | A single case was reported and was present on an unusual site of buccal space. Management of noninvasive CAEXPA becomes difficult in case of such an unusual site. It showed benign course with a malignant potential. |
| Mori T et al., [17] | Three cases were reported and total 14 cases (previous 11 cases were included) were studied for HER-2/neu protein out of which 12 showed positivity for HER-2/neu. HER-2/neu is an important marker to differentiate pleomorphic adenoma from noninvasive CAEXPA. |
| Matsushima M et al., [18] | The case reported in the submandibular area with the renal metastasis. The case report suggest of stages of malignant transformation of pleomorphic adenoma |
| Ismi O et al., [19] | A case reported in the submandibular region was originating from ectopic salivary gland. In the reported case, myoepithelial cells were showing malignant transformation which is only 19% of other CAEXPA cases. |
| Mohan S et al., [20] | An unusual case of noninvasive CAEXPA was reported with the finding of ossification in the tumour. Two theories were proposed to explain the presence of ossification, first theory was endochondral ossification, showing a cartilaginous precursor and second theory was due to direct myoepithelial cells in the tumours. Differential diagnosis included many tumours occurring in the parotid region. |
| Scognamiglio T et al., [21] | A case of noninvasive CAEXPA was reported and after Fine Needle Aspiration (FNA) the malignant part of CAEXPA was diagnosed as adenocarcinoma (Not otherwise specified). Sensitivity of FNA for CAEXPA is very less that is 29% which is of less importance for surgical planning. |
| Vahedi M et al., [22] | A case reported on buccal mucosa. Author also stated that the risk of malignancy is directly related to the duration of tumour. In case of small and noninvasive CAEXPA surgery is the only treatment of choice. |
Recent studies have shown that Carcinoma ex pleomorphic adenoma is a multi step carcinogenesis with the progressive loss of heterozygosity at the chromosome 8q, then12q and finally 17p [8].
Conclusion
A case reported here is a rare noninvasive carcinoma ex pleomorphic adenoma of the salivary gland. This noninvasive type of carcinoma ex pleomorphic adenoma show typical and characteristic clinical history of short duration. Usually, CAEXPA shows history of three to eleven years but here in our case it was since two years only. Not only clinically but histologically also it is a rare variant. It is a dreadful disease affecting salivary glands and can cause death if not diagnosed early. So it is very important that pathologist and surgeons should know this entity clinically and pathologically to avoid the confusion in diagnosis and treatment plan.
[1]. Irving Dardiclk, Colour Atlas/ Text of salivary gland tumours pathology 1996 Newyork:TokyoIgakushoin [Google Scholar]
[2]. Zhao J, Wang J, Yu C, Guo L, Wang K, Liang Z, Prognostic factors affecting the clinical outcome of carcinoma ex pleomorphic adenoma in the major salivary glandWorld Journal of Surgical Oncology 2013 11(1):180 [Google Scholar]
[3]. Gnepp D, Diagnostic surgical pathology of the head and neck 2009 1st edPhiladelphia, PASaunders/Elsevier [Google Scholar]
[4]. DR G. Malignant mixed tumours of the salivary glands: A reviewPathology Annual 1993 28(Pt 1):279-328. [Google Scholar]
[5]. Ellis GAuclair P, Tumours of the salivary glands 2008 1st edWashington D.CAmerican Registry of Pathology [Google Scholar]
[6]. Mariano FV, Noronha ALF, Gondak RO, de AM Altemani AM, de Almeida OP, Kowalski LP, Carcinoma ex pleomorphic adenoma in a Brazilian population: Clinico pathological analysis of 38 casesInternational Journal of Oral and Maxillofacial Surgery 2013 42(6):685-92. [Google Scholar]
[7]. Fletcher C, Diagnostic histopathology of tumours 2013 1st edPhiladelphia, PASaunders/Elsevier [Google Scholar]
[8]. Antony J, gopalan V, Smith R, Lam A, Carcinoma ex pleomorphic adenoma: A comprehensive review of clinical, pathological and molecular dataHead and Neck Pathology 2011 6(1):1-9. [Google Scholar]
[9]. Livolsi V, Perzin K, Malignant mixed tumours arising in salivary glands. I. Carcinomas arising in benign mixed tumours: A clinicopathologic studyCancer 1977 39(5):2209-30. [Google Scholar]
[10]. Brandwein M, Huvos A, Dardick I, Thomas M, Theise N, Noninvasive and minimally invasive carcinoma ex mixed tumourOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 1996 81(6):655-64. [Google Scholar]
[11]. Lewis J, Olsen K, Sebo T, Carcinoma ex pleomorphic adenoma: Pathologic analysis of 73 casesHuman Pathology 2001 32(6):596-604. [Google Scholar]
[12]. Felix A, Rosa-Santos J, Mendonça M, Torrinha F, Soares J, Intracapsular carcinoma ex pleomorphic adenoma. Report of a case with unusual metastatic behaviourOral Oncology 2002 38(1):107-110. [Google Scholar]
[13]. Di Palma S, Skalova A, Vanieek T, Simpson R, Starek I, Leivo I, Non invasive (intracapsular) carcinoma ex pleomorphic adenoma: Recognition of focal carcinoma by HER-2/neu and MIB1 immunohistochemistryHistopathology 2005 46(2):144-52. [Google Scholar]
[14]. Ethunandan M, Witton R, Hoffman G, Spedding A, Brennan P, Atypical features in pleomorphic adenoma—a clinicopathologic study and implications for managementInternational Journal of Oral and Maxillofacial Surgery 2006 35(7):608-12. [Google Scholar]
[15]. Kunimura T, Noninvasive carcinoma ex pleomorphic adenoma of the parotid glandOtolaryngology-Head and Neck Surgery 2007 137(4):687-88. [Google Scholar]
[16]. Dandekar M, Chaukar D, Kane S, Juvekar S, D’Cruz A, Intracapsular carcinoma ex pleomorphic adenoma in the buccal space: Management dilemmaInternational Journal of Head and Neck Surgery 2010 1(1):21-24. [Google Scholar]
[17]. Mori T, Kunimura T, Saito K, Date H, Arima S, Matsuo K, Three cases of noninvasive carcinoma ex pleomorphic adenoma of the parotid gland and a literature survey focusing on their clinicopathologic featuresThe Showa University Journal of Medical Sciences 2010 22(2):127-34. [Google Scholar]
[18]. Matsushima M, Ohara R, Ishida M, Kanao K, Shimokawa R, Nakajima Y, Carcinoma ex pleomorphic adenoma of the submandibular gland with renal metastases composed exclusively of metastasizing pleomorphic adenomaInternational Cancer Conference Journal 2012 1(2):116-20. [Google Scholar]
[19]. Ismi O, Vayısoglu Y, Bozdogan Arpaci R, Eti C, Pütürgeli T, Gorur K, Carcinoma ex pleomorphic adenoma originating from ectopic salivary gland in the neck region: Case reportGland Surgery 2016 4(6):567-71. [Google Scholar]
[20]. Mohan S, Puram S, Yarlagadda B, Nosé V, Deschler D, Ossifying parotid carcinoma ex pleomorphic adenomaCase Reports in Otolaryngology 2015 2015:1-4. [Google Scholar]
[21]. Scognamiglio T, Kuhel W, Tabbara S, Rezaei M, Hoda R, Joshi R, Noninvasive carcinoma ex pleomorphic adenoma of the parotid gland: A difficult diagnosis on fine needle aspirationCytoJournal 2015 12(1):7 [Google Scholar]
[22]. Vahedi M, Reza Jamalpour M, Hashemi A, Ronasi N, Abdolkarimpour Z, Carcinoma ex pleomorphic adenoma in the buccal minor salivary gland: A rare case reportScholars Academic Journal of Biosciences (SAJB) 2016 4(8):696-99. [Google Scholar]