A number of congenital and acquired dermatological diseases are known to follow lines of Blaschko. Lichen Planus (LP), commonly acquired inflammatory dermatosis, presents with various morphological forms but Blaschkoian variant is very less published in literature. We herein report a case series of six patients of various age groups with Blaschkoian LP, without any underlying predisposing factors. All these cases presented with asymptomatic to mildly pruritic, violaceous to hyperpigmented papules and plaques following the Blaschko lines. In all the patients, lesions responded well to topical steroids and oral antihistamines, leading to gradual resolution of lesions with post-inflammatory hyperpigmentation. Blaschkoian LP is not a rare condition and may remain under reported because of its insignificant clinical features especially the absence of pruritus. Thus, the physician should always keep this entity in mind while considering the lesions following lines of blaschko.
Lines of Blaschko, Post inflammatory hyperpigmentation, Topical steroids
Case Series
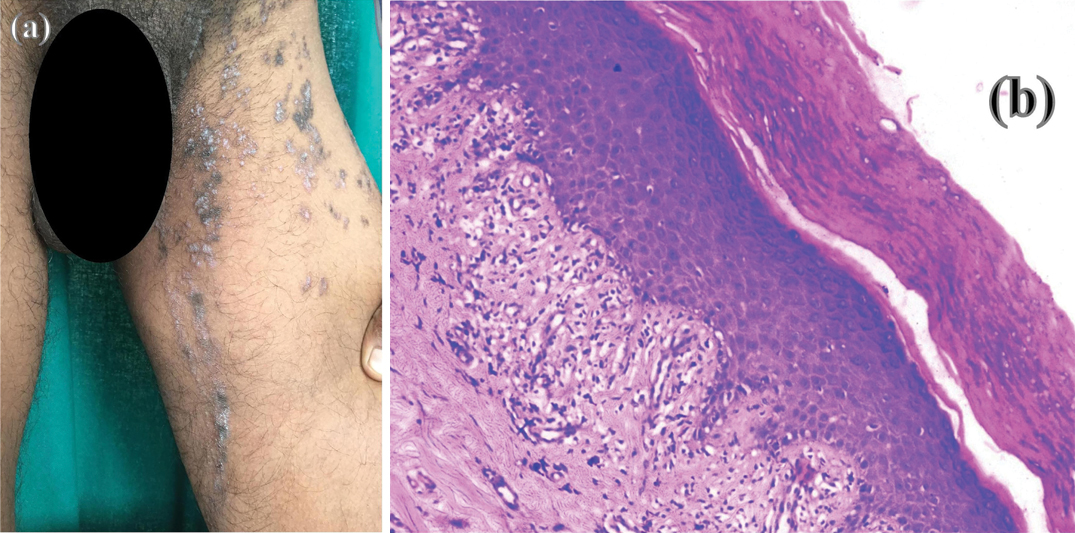
Case 1: An18-year-old male presented with a history of asymptomatic raised purple lesions on left half of body involving lower extremities, trunk and external genitalia since one year without any history of waxing and waning. Cutaneous examination showed violaceous papules and plaques associated with mild scaling over the plaques [Table/Fig-1]. The lesions were following lines of Blaschko on left side of thigh, leg and scrotum.
(a) Violaceous papules and plaques distributed along lines of blaschko on left thigh; (b) Histopathological examination showing typical features of LP (compact orthokeratosis, hypergranulosis, irregular acanthosis with basal cell vacuolization and band like lymphocytic infiltration at Dermoepidermal junction (DEJ) (H&E stain, 10x).
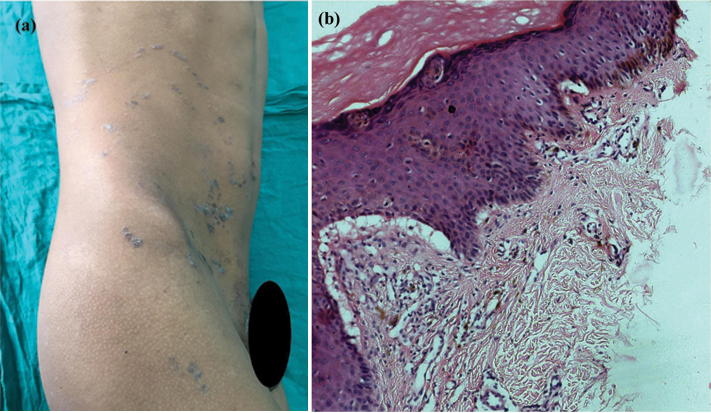
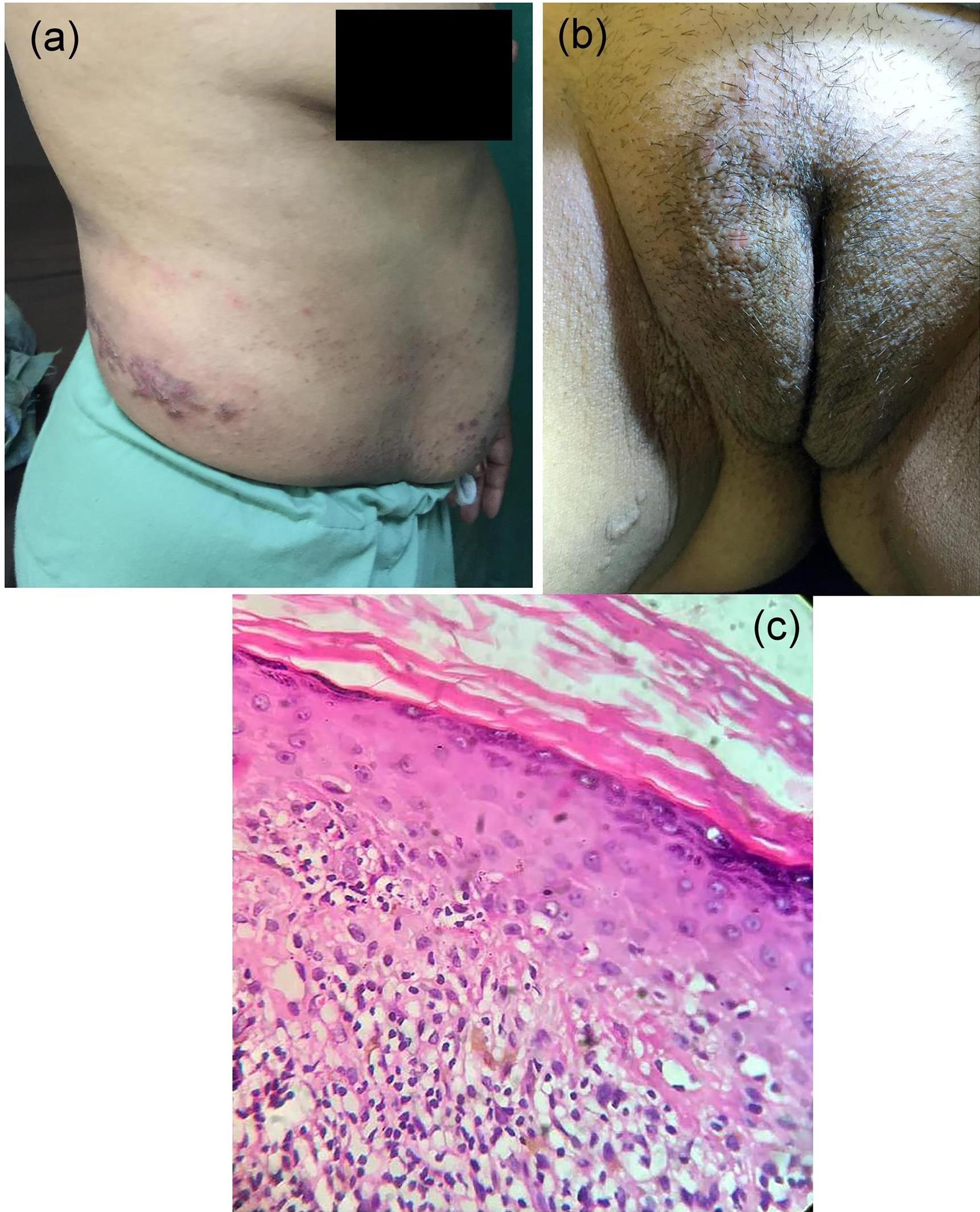
Case 2: A 15-year-old male presented with a history of raised lesions over the abdomen and right thigh since two years which were associated with mild pruritus. Patients did not give any history of drug intake or any topical application. On cutaneous examination, violaceous polygonal papules and plaques following the S-shape pattern on the right side of abdomen and linear pattern of Blaschko lines on the right upper thigh were present [Table/Fig-2].
(a) Violaceous papules and plaques distributed along Blaschko lines unilaterally on the right side of abdomen, thigh and genital; (b) Histopathological examination showed compact orthokeratosis, hypergranulosis, irregular acanthosis, max joseph space, lymphocytic infiltrate at DEJ with melanin incontinence. (H&E stain, 10x).
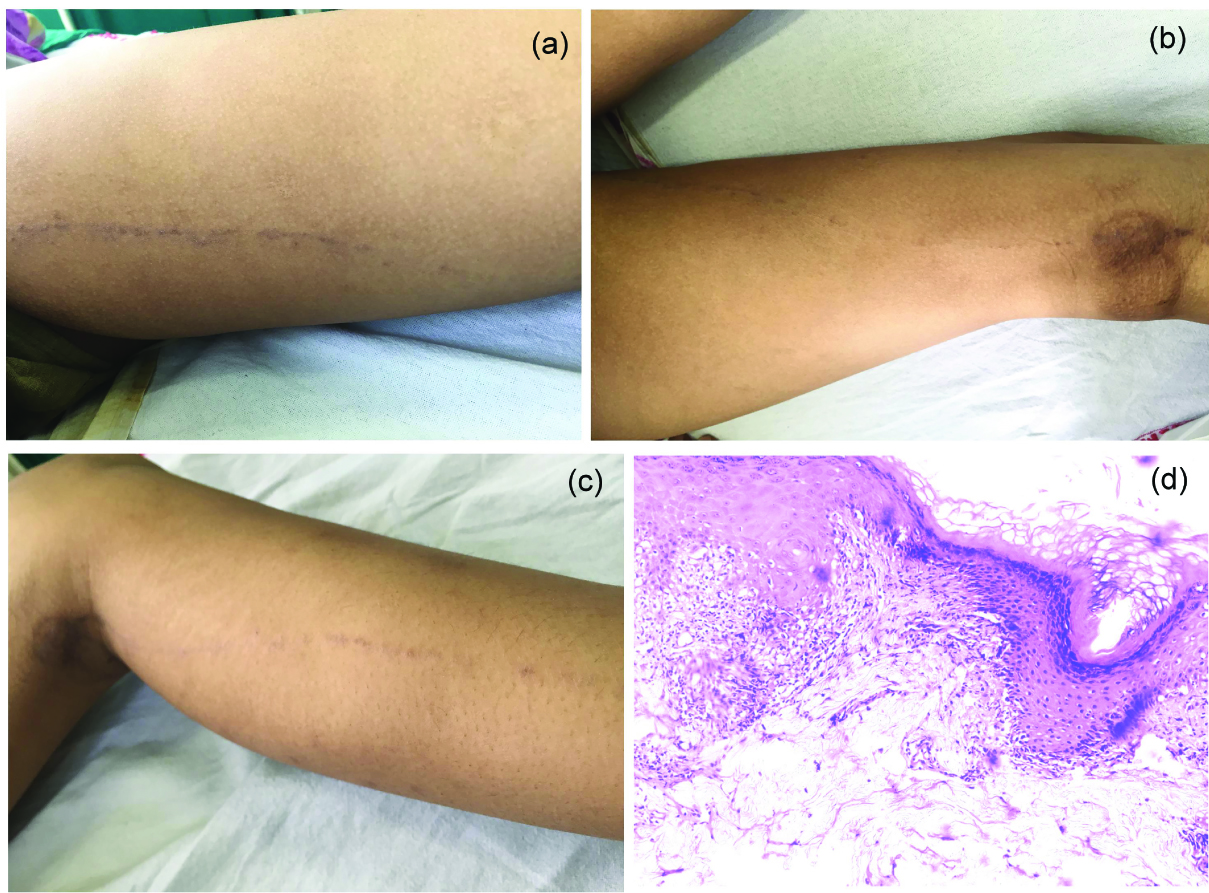
Case 3: A 10-year-old female presented with asymptomatic raised dark lesions over left thigh extending up to the ankle since 6 months. Dermatological examination revealed presence of multiple hyperpigmented to violaceous papules over medial side of left thigh, extending to the posterior aspect of leg up to the medial side of left ankle along the line of Blaschko [Table/Fig-3]. A differential diagnosis of LP and lichenoid disorders were kept initially and a skin biopsy was done. But none of the lichenoid disorders follow the lines of Blaschko. Furthermore, histopathological examination revealed acanthosis, hypergranulosis, basal cell vacuolization with band like lichenoid infiltrate in the papillary dermis (Haematoxylin & Eosin stain, 10x). Thus, the presence of predominantly lymphocytic infiltrate with absence of other type of cells namely, eosinophils, neutrophils, mast cells, histiocytes and parakeratosis on histopathology favoured the diagnosis of LP instead of lichenoid dermatosis.
(a-c) Violaceous macules and papules on the left thighs and extending down the posterior aspect of left leg; (d) Histopathological examination showed acanthosis, hypergranulosis, basal cell vacuolization with band like lichenoid infiltrate in the papillary dermis. (H&E stain, 10x).
Case 4: A 25-year-old female came with the history of multiple mildly pruritic, violaceous raised lesions over right lower limb since one and half years. On dermatological examination, multiple violaceous polygonal papules were present over right lower limb along the lines of Blaschko [Table/Fig-4].
(a) Violaceous to hyperpigemented papules on the anterior aspect of right leg following the blaschko lines; (b) Histopathological examination showing orthokeratosis, max-joseph space and lymphocytic infiltrate in the papillary dermis. (H&E stain, 10x).
Case 5: A 53-year-old female patient presented with history of mildly itchy red to violaceous raised skin lesions on right side of abdomen and genitalia since one year. On cutaneous examination there were multiple violaceous to erythematous papules coalescing to form plaques on right side of the back and abdomen in an S-shaped pattern and linear fashion on the right upper thigh & mons pubis following the Blaschko lines with sharp demarcation at midline. It was also extending to the right antecubital fossa, elbow and chest [Table/Fig-5].
(a) Violaceous papules coalescing to form plaques present on right side of abdomen following the S-shape pattern; (b) Similar violaceous papules were present unilaterally on the right side of thigh and mons pubis following the linear pattern of blaschko lines; (c) Histopathological examination showing hyperkeratosis, hypergranulosis, acanthosis, melanin incontinence with basal cell vacuolization and lymphocytic infiltrate at DEJ. (H&E stain, 10x).
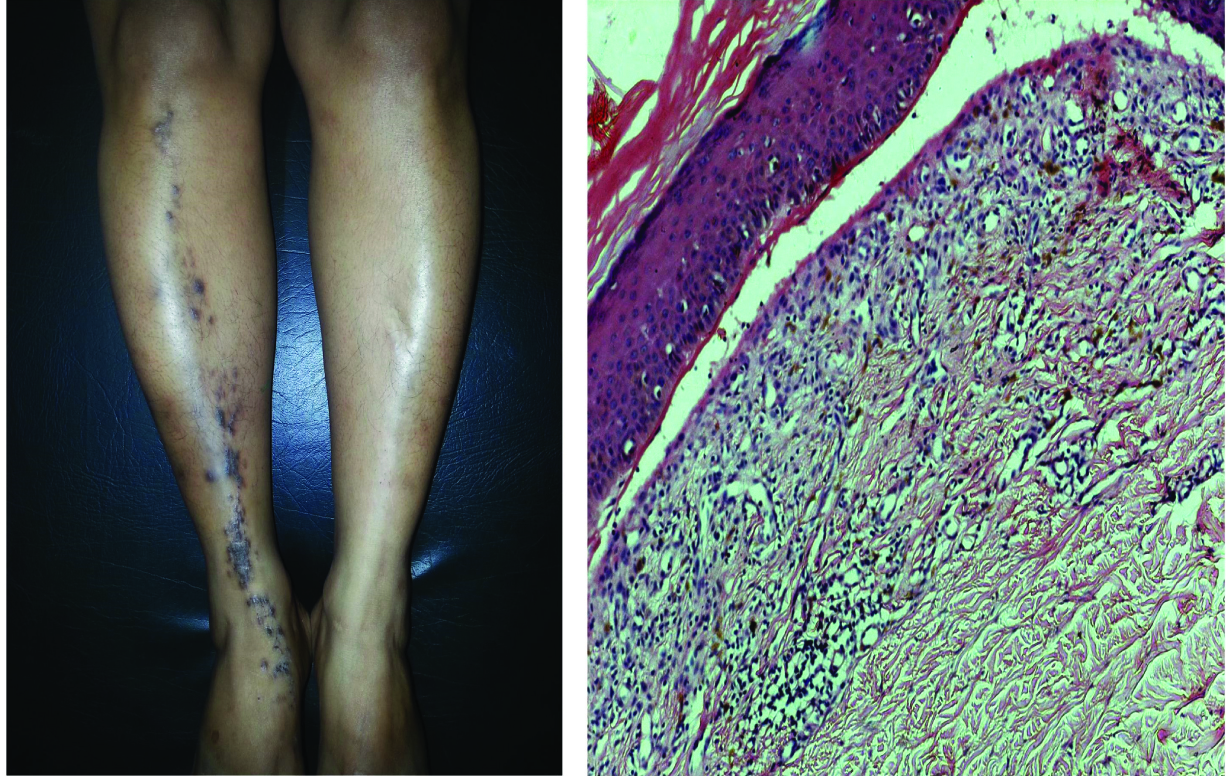
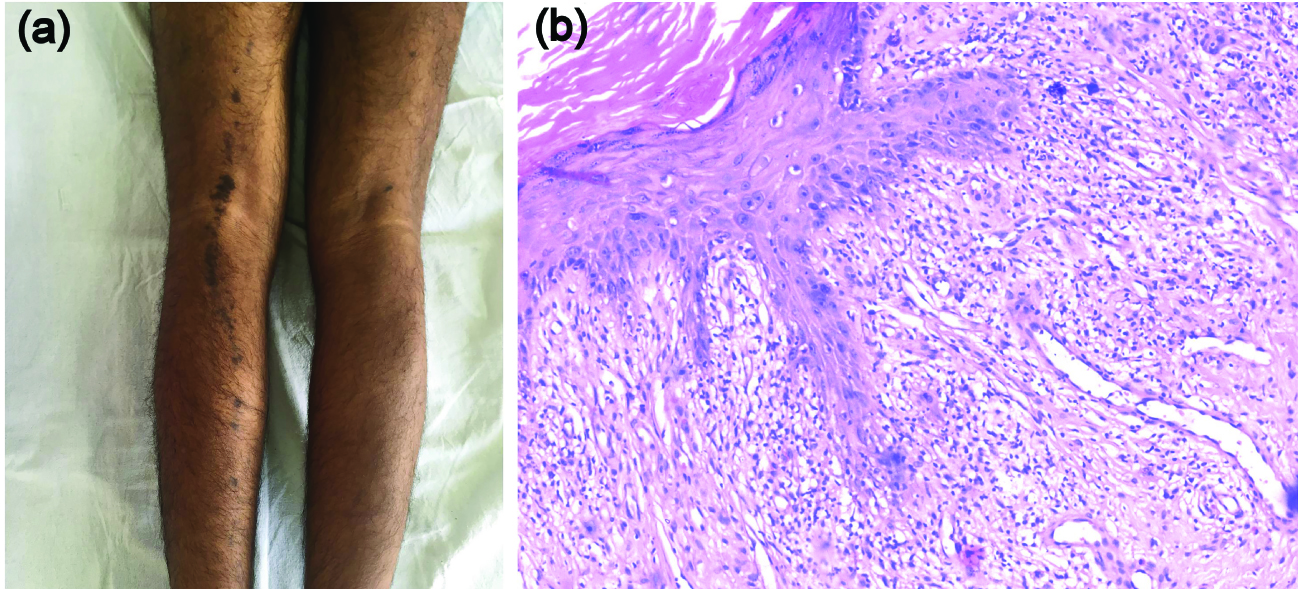
Case 6: A 20-year-old male patient came with the history of asymptomatic dark coloured raised lesions on back side of left leg since one year. On dermatological examination there were multiple hyperpigmented papules and plaques on the posterior aspect of left leg following the lines of Blaschko [Table/Fig-6].
(a) Violaceous to hyperpigmented papules and plaques present posterior surface of left leg in a linear pattern of blaschko lines; (b) Photomicrograph showing orthokeratosis, hypergranulosis, acanthosis, basal cell vacuolization and dense band like lymphocytic infiltrate. (H&E stain, 10x).
In all the cases, the family history and past history was insignificant. There was no history of preceding infection, topical application, trauma, drug intake or any dermatological disease in either of the cases. In addition, there was no history of waxing and waning in any of the cases. In all the cases, no abnormalities were found on general physical examination. Rest of the cutaneous examination including scalp, nail and mucous membranes were insignificant. All the patients underwent routine laboratory tests which were normal including serology for hepatitis B and C. Skin biopsy was also done in all the cases from the representative papular lesions. Histopathological features in almost all the cases revealed orthokeratosis, hypergranulosis, acanthosis, basal cell vacuolization and dense band like lymphocytic infiltrate with Haematoxylin & Eosin stain under 10X magnification. In case 2 and 3 histology also showed max joseph space. All these features were consistent with the diagnosis of LP. All the patients were started on topical steroids i.e., 0.1% mometasone cream twice daily with tablet levocetirizine 5 mg once a day. This produced a symptomatic and clinical improvement within a month, healing with post-inflammatory hyperpigmentation.
Discussion
LP is an acquired inflammatory dermatosis, of which several clinical variants have been described according to the morphology and distribution of the lesions. Various types of LP have been described in the literature, which include hypertropic, atrophic, actinic, guttate, erosive, follicular, zosteriform, etc., Linear Lichen Planus (LLP) is a variant of LP, which accounts for 0.24–0.62% of all cases of LP. It is mainly diagnosed in children and adolescents, with an estimated incidence at 9–11.4% of all cases of LP in this group [1]. Two types of LLP have been described in the literature: one that follows the lines of Blaschko also called as Blaschkoian LP and one secondary to koebnerization. Blaschkoian LP is described rare in the literature [2,3], but probably it is underdiagnosed, as it is usually asymptomatic or associated with mild pruritus and variable clinical features.
Lesions of Blaschkoian LP run along Blaschko lines which pursue a V-shape over upper spine, S-shape on abdomen, an inverted U-shape from the breast onto the upper arms and linear patterns down the front and back of lower extremities and less well defined on head and neck. These never cross midline [4]. The concept of Blaschko lines was given by Alfred Blaschko in 1901 [2]. These lines do not follow vascular, lymphatic or nervous pathways but are due to genetic mosaicism resulting from either lyonization (1 out of two X chromosomes in women get inactivated randomly) or somatic postzygotic mosaicism [4]. They were previously thought to signify koebner’s phenomenon but curvature of the lesions was against this hypothesis [3]. No exact cause of Blaschkoian LP (BLP) has been elucidated but one hypothesis states that it is an idiopathic acquired inflammation of Blaschko lines (blaschkitis) without any underlying isomorphism [2].
A review of English literature was done for linear LP which follows the lines of Blaschko in the pubmed and is shown in [Table/Fig-7] [1-3,5-12]. As highlighted in the table, in our case series of six patients, the age group ranged from 10-53 years, and predominantly affected the adolescent patients. On scanning the literature, there is only one case series of three children with Blaschkoian LP and one case report. Rest of the reported cases is in adult age group. In our case series, there is only one case of childhood Blaschkoian LP. Thus, there is paucity of cases of childhood Blaschkoian LP in the Indian literature.
Cases of unilateral LP following lines of Blaschko in English literature (Based on Pubmed search) [1-3,5-12].
| Author’s name | Number of patients | Sites affected | Age/ Sex | Precipitating factors | Treatment |
|---|
| 1. | Sharma R et al., [5] | 2(patient A and B) | Left side of the body | A: 54 yr/ FB: 45 yr/M | Nil | Oral prednisolone 40 mg/day for 10 days was given and the lesions flattened with hyperpigmentation. The dose of prednisolone was gradually tapered over the next 3 months. No recurrence of lesions was seen during a follow-up period of 10 months after stopping the treatment. |
| 2. | Klein HA et al., [6] | 1 | Right side of chest, arm, back, flank, and leg | 32 yr/ F | Nil | A 3 weeks course of oral prednisolone 40 mg with clinical and symptomatic improvement, after which steroids were tapered over a few weeks |
| 3. | Ber Rahman Set al., [2] | 1 | Right side of the body | 30 yrs/ M | Nil | Topical steroids and antihistaminics were given |
| 4. | Gupta S et al., [7] | 1 | Left side of the trunk, flank and back | 34 yrs/ M | Nil | Topical steroids and oral antihistaminics and lesions healed with hyperpigmentation |
| 5. | Lade NR et al., [8] | 1 | Left side of chest lower abdomen, back and pelvic area | 32 yrs/F | Nil | Oral prednisolone 0.5 mg/kg, which was tapered over a month. The papules completely subsided, and healed with pigmentation |
| 6. | Yayla D et al., [3] | 2 (patient A & B) | A: Right armB: Left half of body | A: 50 yr/MB: 71 yr/F | A: NilB: might be secondary to olanzapine | A & B: Patients were treated with topical corticosteroids and antihistamines; lesions healed with PIH† |
| 7. | Michalska-Bańkowska A et al., [1] | 1 | A: left side of body | A:29 yr/F | May by following trauma or oral telmisartan | Treated with topical steroids and emollients |
| [although Michalska-Bańkowska et al., had included 3 cases but we only took 1 case, as rest others were bilateral in distribution] |
| 8. | Present study | 6 | Involve various parts of the body | Range from 10-53 years | Nil | All the patients were treated with topical steroids and oral antihistamines and lesions healed with PIH. |
| Children |
| 1. | Kabbash C et al., [9] | 3 (patient A & B) | A: From midback extending on the dorsal area of handB:left abdomen | A-12 yr /FB-13 yr /M | Nil | A: Started on potent steroidsB: Started on topical clobetasol propionate |
| [although Kabbash et al., had presented details of 3 patients but we only took 2 patients as one patient has bilateral involvement] |
| 2. | Horowitz MRet al., [10] | 1 | Right side of abdominal region, buttocks and thigh | 2 yr and 8 months / F | Nil | Patient was treated with topicalsteroids, with good response which heal wit residual hyperchromic stains |
| Pregnant Female |
| 1. | Krasowska Det al., [11] | 1 | Right upper limb,the outside of the right thigh, right side of the chest and epigastrium | 33 yr/ F | Nil | Patient was given cimetidine (2×400 mg) for 10 weeks combined with topical fluticasone propionate. After 2.5 months of treatment, the rash flattened and improved, although it heal with PIH |
| 2. | Kumar S et al., [12] | 1 | Left side of the body | 24 year pregnant female | Nil | Not available |
*Yr: Year, M: Male, F: Female, †PIH: Post inflammatory hyperpigmentation.
In our patients, males outnumbered the females, which is in concordance with the earlier reports. Trunk and extremities was the most common site affected in various case reports and is in concordance with our case series. According to Michalska-Bankowska et al., mechanical injury, surgery or telmisartan could be the predisposing factors in their cases [1]. Similarly, Yayla et al., had also described olanzapine as the inflicting cause of LP in their 2nd case [3]. But no predisposing factors could be identified in our case series and in various earlier case reports. Usually Blaschkoian LP is idiopathic but it may be associated with underlying cause, hence evaluation of underlying predisposing factors is mandatory. In our case series, patients responded very well to topical steroids and antihistaminic but in various case reports they required oral steroids which may be due to extensive involvement of LP in their patients. Thus, large multicentric reports are suggested to exactly delineate the epidemiology, clinical features and course of this entity. Ours is a preliminary effort in this direction.
Conclusion
Thus, we conclude that Blaschkoian LP is not so rare condition. It usually follows a benign course without any grim sequel. The treating dermatologist must be aware of this variant and it should be considered as differential diagnosis while dealing with conditions following the lines of Blaschko.
*Yr: Year, M: Male, F: Female,
†PIH: Post inflammatory hyperpigmentation.
[1]. Michalska-Bańkowska A, Skrzypek-Salamon A, Lis-Święty A, Linear lichen planus along the lines of Blaschko in three adult women: gene- environment interactionsClin Dysmorphol 2015 24:166-69. [Google Scholar]
[2]. Ber Rahman S, Ul Bari A, Mumtaz N, Unilaternal blaschkoid lichen planus involving the entire half of the body, a unique presentationDermatol Online J 2007 13(3):36 [Google Scholar]
[3]. Yayla D, Cakmak SK, Oguz ID, Gonul M, Ozhamam E, Colak A, Two cases of unilateral lichen planus following the lines of blaschkoAnn Dermatol 2014 26:636-38. [Google Scholar]
[4]. Tagra S, Talwar AK, Walia RS, Lines of blaschkoIndian J Dermatol Venereol Leprol 2005 71:57-59. [Google Scholar]
[5]. Sharma R, Maheshwari V, Chandra M, Unilateral multiple linear lichen planus along the line of Blaschko: A report of two casesIndian J Dermatol Venereol Leprol 1999 65:225-26. [Google Scholar]
[6]. Klein HA, Krathen RA, Hsu S, Widespread Blaschkoid lichen planusDermatol Online J 2006 12:17 [Google Scholar]
[7]. Gupta S, Gupta S, Thomas M, Mahendrea A, Unilateral lichen planus along the lines of Blaschko: a rare presentationActa Medica Indonesiana 2012 44:163-64. [Google Scholar]
[8]. Lade NR, Saoji V, Singh A, Blaschkoid lichen planus: not a koebner phenomenonDermatol Online J 2013 19:17 [Google Scholar]
[9]. Kabbash C, Laude TA, Weinberg JM, Silverberg NB, Lichen planus in the lines of BlaschkoPediatr Dermatol 2002 19:541-45. [Google Scholar]
[10]. Horowitz MR, Vidal Mde L, Resende MO, Teixeira MA, Cavalcanti SM, Alencar ER, Linear lichen planus in children—case reportAn Bras Dermatol 2013 88:139-42. [Google Scholar]
[11]. Krasowska D, Pietrzak A, Lecewicz-Toruń B, Unilateral multiple linear lichen planus following the Blaschko lines recurring after deliveriesDermatology 2001 202:340 [Google Scholar]
[12]. Kumar S, Okade R, Rahman YA, Unilateral Blaschkoid lichen planus in successive pregnanciesDermatol Reports 2011 3:35 [Google Scholar]