Shoulder pain is the third most common cause of musculoskeletal pain after low back pain and knee pain, and can result in considerable morbidity with diminished quality of life [1]. Amongst patients with shoulder pain, rotator cuff disorders are most frequently implicated, being present in upto 86% of patients. Imaging is necessary to determine the exact cause of shoulder pain so as to institute appropriate therapy. Various imaging modalities that can be used to evaluate shoulder pathologies include plain radiographs, contrast arthrography, computed tomography, ultrasonography and magnetic resonance imaging.
Currently, arthroscopy is considered the “reference standard” for the diagnosis of shoulder pathologies. However, arthroscopy is an invasive procedure that requires hospitalisation and anaesthesia, and carries a small risk of complications such as infection, damage to adjacent structures such as brachial plexus, as well as anaesthesia related complications [2].
MRI with its excellent soft tissue resolution and multiplanar imaging capabilities has now emerged as the investigation of choice in the preoperative evaluation of rotator cuff diseases [3]. MRI provides useful information about tear dimension, tear depth, tendon retraction, which can influence treatment decision. In addition, MRI also provides information about tendon retraction, muscle atrophy, fatty degeneration and coracoacromial impingement, which may have important prognostic implications [4]. However, MRI has certain disadvantages such as being less widely available, and is contraindicated in patients with cardiac pacemakers, certain metallic implants and in claustrophobic patients.
The purpose of this study was to study the efficacy of routine MRI in the diagnosis and characterisation of rotator cuff tears and to correlate the findings with arthroscopy so as to evaluate the accuracy of MRI in the diagnosis of rotator cuff tears.
Materials and Methods
This prospective study was carried out in the Department of Radiodiagnosis, AJ Institute of Medical Sciences, Mangalore, Karnataka, India, between July 2014 and August 2016. During this study period, a total of 82 patients were diagnosed with rotator cuff injury on MRI. Out of these, 23 patients did not undergo arthroscopy and were excluded from this study. They include 10 patients with tendinosis, six patients with intrasubstance tears, and seven patients with minor surface tears. Fourteen patients were lost to follow up after MRI and were also excluded. The remaining 45 patients underwent arthroscopic evaluation at our institution, and form the subjects of this study. Other exclusion criteria included patients with a previous history of surgery or prosthesis in the shoulder, patients with pacemakers or metal implants in the body, claustrophobic patients and patients unwilling to participate in the study. The study was approved by our Institutional Ethics Committee and informed consent was obtained from all patients.
All patients were evaluated on a superconducting 1.5-T Siemens Magnetom Avanto MR unit, using a surface coil. Our protocol for MR evaluation of the rotator cuff includes a T1W and T2W fast spin echo sequence in the axial, coronal oblique and sagittal oblique planes, as well as a Fat Saturated Proton Density (FSPD) sequence in the three planes. The imaging parameters for T1W and T2W sequence was a TR/TE of 420/11 and 3500/70 respectively, while the FSPD sequence was obtained with a TR/TE of 2650/30. All images were acquired with a slice thickness of 3 mm, an interslice gap of 1 mm, field of view of 160 mm and a matrix size of 256 x 128.
Rotator cuff tears detected on MRI were classified as full thickness or partial thickness tears. Partial thickness tears were further classified as articular surface or bursal surface depending on whether the undersurface or superior surface was involved. Tears involving the substance of the tendon (intrasubstance tears) were not considered in this study since they are most often not detected on arthroscopy. The size and depth of the tears were assessed. Involvement of adjacent structures such as biceps tendon was assessed. Presence of ancillary findings such as joint effusion, bursal fluid or bone changes was noted. All 45 patients underwent arthroscopic evaluation of the shoulder joint.
Statistical Analysis
The data was entered into Microsoft Excel spreadsheet, and a descriptive analysis was carried out. SPSS software (version 16) was used for all calculations. Chi-square test was used to assess for significance of association between two variables. Kappa statistics was used to test the level of agreement between MRI and arthroscopic findings. A p < 0.05 was considered as statistically significant. The sensitivity, specificity, positive and negative predictive value and accuracy of MRI in the diagnosis of rotator cuff tears were evaluated using arthroscopic findings as standard reference.
Results
A total of 45 patients who were evaluated with both MRI and arthroscopy for rotator cuff tears, were included in this study. There were 27 males and 18 females, suggesting a male predominance of 1.5:1. The youngest patient was 22 years and the oldest was 74 years with a mean age of 50.39±12.66 years. Majority of rotator cuff tears were observed in patients above 40 years of age, which included 35 of the 45 patients (78%). Right sided dominance was seen in 41 out of 45 patients (91%) and left sided dominance was seen in 9%. Pain was the most common presenting complaint which was seen in 40/45 patients (88.8%), followed by diminished range of movement, which was seen in 19/45 patients (42.2%). A history of trauma was elicited in 12 patients (26.6%).
Out of the 45 patients, 26 patients were diagnosed with full thickness tears and 19 patients were diagnosed with partial thickness tears on MRI. The partial tears included 15 with articular surface tears and four with bursal surface tears. In comparison, arthroscopy revealed 29 patients with full thickness tears and 15 patients with partial thickness tear (12 articular surface tear and three bursal surface tear). One patient who was diagnosed with articular surface partial thickness tear on MRI did not show any tear on arthroscopy, but showed only an inflammed tendon [Table/Fig-1]. The most commonly involved tendon was supraspinatus tendon which was involved in all 45 patients (100%), followed by infraspinatus tendon involvement in 11 (24.4%) patients, subscapularis tendon involvement in nine (20%) patients. There was no patient with teres minor tear in this study.
Distribution of patients with full and partial thickness tears on MRI and arthroscopy.
| Full thickness | Partial thickness | Normal | Total |
|---|
| MRI | 26 | 19 | -- | 45 |
| Arthroscopy | 29 | 15 | 1 | 45 |
Thus, MRI was able to correctly diagnose full thickness tears in 26/29 cases, giving a sensitivity of 89.6%, specificity of 100%, positive predictive value of 100% and negative predictive value of 83.3%. For partial thickness tears, MRI showed a sensitivity of 100%, specificity of 86.6%, and positive predictive value of 78.9% and negative predictive value of 100%. The accuracy was 93.1% for full thickness tears and 91.1% for partial thickness tears [Table/Fig-2]. The p-value was less than 0.01 for both full and partial thickness tears. The kappa value was also calculated and was found to be 0.85 for full thickness tears and 0.81 for partial thickness tears, suggesting very good level of agreement between MRI and arthroscopy in the diagnosis of rotator cuff tears. The most sensitive finding in full thickness tears was the presence of fluid signal intensity in the location of the rotator cuff on PD fat saturated images.
Correlation of MRI findings with arthroscopy.
| n = 45 | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy | p-value | Kappa coefficient |
|---|
| Full thickness tears | 89.6 | 100 | 100 | 83.3 | 93.1 | <0.01 | 0.85 |
| Partial thickness tears | 100 | 86.6 | 78.9 | 100 | 91.1 | <0.01 | 0.81 |
(Chi-square test and Cohen’s Kappa test were used to calculate p-value and kappa coefficient)
Certain ancillary findings that were detected in our study are shown in [Table/Fig-3]. Fluid in the Subacromial-Subdeltoid (SASD) bursa was the commonest finding and was seen in 25 (55.5%) patients, while fluid in the subcoracoid bursa was seen in 23 (51%) patients and joint effusion was seen in 19 (42%) patients. Acromio-Clavicular (AC) joint arthrosis was seen in 12 (26.6%) patients. Other additional findings which we encountered were greater tubercle fracture in two (4%) patients, Hill Sachs/Bankart’s lesion in one (2%) and labral tear in one (2%) patients.
Ancillary MRI findings in patients with rotator cuff tears.
| Findings | Frequency | Percentage |
|---|
| SASD bursal effusion | 25 | 55.5% |
| SC bursal effusion | 23 | 51% |
| Joint effusion | 19 | 42% |
| AC joint arthrosis | 12 | 26.6% |
| Fracture greater tubercle | 2 | 4% |
| Hill Sach’s and Bankart | 1 | 2% |
| Labral tear | 1 | 2% |
SASD – subacromial subdeltoid. SC – subcoracoid. AC – acromio-clavicular.
Discussion
The rotator cuff injury was more common in males than females in our study with a ratio of 1.5:1. The right shoulder and dominant arm were more commonly affected than the left shoulder and non dominant arm. Majority of the rotator cuff tears (78%) were seen in patients above the age of 40. Thus the risk factors for rotator cuff injuries in our study were male gender, right shoulder and dominant arm, and advancing age. Our findings compare favourably with Yamamoto A et al., who reported that rotator cuff tears were more commonly associated with elderly age, male population and affected the dominant arm [5]. Advancing age causes tendons to degenerate which in turn predisposes to tears, occurring most commonly after the fourth decade and increasing linearly thereafter.
In our study, full thickness tears were seen in 29/45 (64.4%) patients and partial thickness tears were seen in 15/45 (33.3%) patients, using arthroscopic diagnosis as the reference. The most commonly involved tendon was the supraspinatus (100%), followed by infraspinatus (25%), subscapularis (20.45%) and teres minor (0%). One patient who had a clinical and MRI diagnosis of partial thickness articular surface tear showed an inflammed tendon with associated bursitis on arthroscopic evaluation, and no evidence of tear. MRI revealed a focal signal change along the articular aspect of the rotator cuff with fluid in the SASD bursa. It is likely that the signal changes of focal tendinitis were overdiagnosed as a partial tear on MRI, and that the patient’s symptomatology were due to associated bursitis.
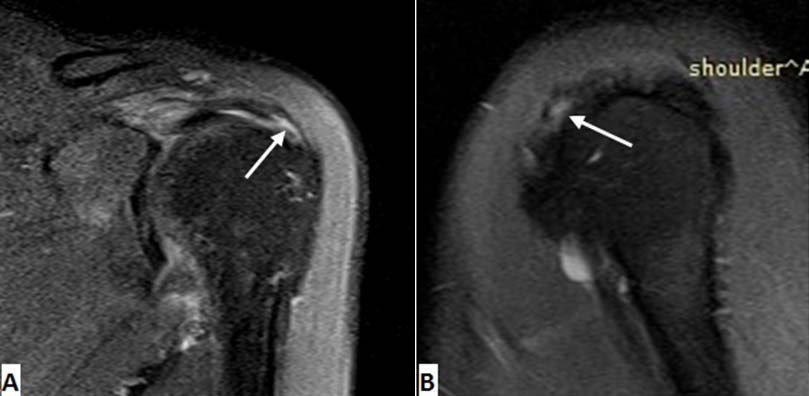
On MRI, the characteristic appearance of a full thickness rotator cuff tear is a focal discontinuity in the tendon extending from the articular to the bursal surface [Table/Fig-4]. This appears as fluid signal intensity on T2W images. In about 10% of cases, the region of tendon discontinuity may be seen as a region of low signal intensity on T2W images due to chronic scarring [6]. Fluid is also seen in the SASD bursa and in the joint space. Secondary signs of cuff tear such as tendon retraction, superior translation of humeral head and muscle atrophy may sometimes be the only indication of a full thickness tear.
Full thickness tears of supraspinatus tendon. FS PD image (a) and T2W FS image (b) Showing discontinuity of supraspinatus tendon which is seen as fluid signal intensity (arrows).

Partial thickness tears were less common than full thickness tears in our study, and were seen in 15/45 (33.3%) cases in our study. Among the partial thickness tears, articular surface tear was seen in 12 patients and bursal surface tears were seen in three patients. These findings are in agreement with other studies which have also shown a more common occurrence of articular surface tears in comparison to bursal surface tears [3,4].
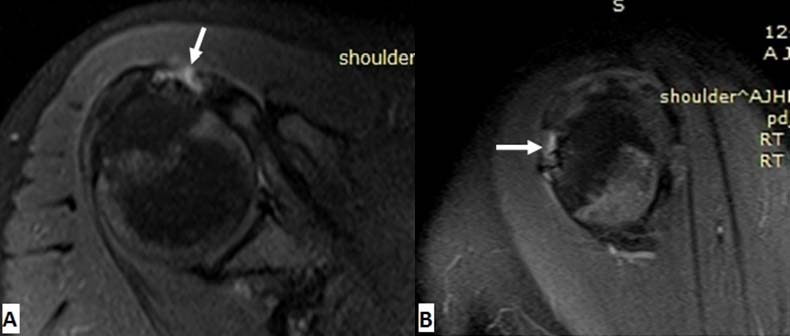
Partial thickness tears are seen on MRI as a focal region of fiber discontinuity filled with fluid signal demonstrated on T2W images [Table/Fig-5, 6]. Fat suppressed sequences may increase the lesion conspicuity by better demonstrating the fluid filled tendon defect [6]. Besides tendon defect, additional findings may include surface fraying or changes in tendon calliber.
FSPD coronal (a) and sagittal (b) images showing partial thickness articular surface tear of supraspinatus tendon (arrows).
PD FS axial (a) and sagittal (b) MR images showing partial thickness tear of distal subscapularis tendon (arrows).
Our study showed a high sensitivity, specificity and positive predictive value for the MRI detection of rotator cuff tears, when correlated with arthroscopy. The accuracy of MRI for the detection of full thickness tears was 93.1% and 91.1% for partial thickness tears. The sensitivity and specificity was 89.6% and 100% for full thickness tears, and 100% and 86.6% for partial thickness tears. The p-value was <0.01 for both full thickness and partial thickness tears suggesting a very strong presumption. The kappa coefficient was also very high for both full thickness and partial thickness tears, suggesting very good agreement between MRI findings and arthroscopy in the diagnosis of rotator cuff tears.
Our results are consistent with literature, with most studies reporting sensitivities and specificities ranging from 85% to 100% for the MRI diagnosis of rotator cuff tears [7]. In a large meta analysis compiled in 2009, de Jesus JO et al., reported a pooled MRI sensitivity and specificity of 92.1% and 92.9% for full thickness tears, and for partial thickness tears of 63.6% and 91.7% [8].
Thus, our study demonstrates that MRI is accurate in the detection of rotator cuff tears and determining the tear extent (full or partial thickness), which may have important implications in guiding treatment decisions. Davidson JF et al., reported that in patients with full thickness tears, the use of preoperative MRI can help in determining the rotator cuff tear pattern, plan the likely method of repair and offer some prognostic information to the patient [9]. Similarly, patients with partial thickness tears involving less than 50% of the tendon thickness may be given an initial trial of conservative management, while most surgeons will consider surgical repair in partial tears involving more than 50% of tendon thickness [10].
Among the associated findings, fluid in the SASD bursa was the most common finding, and was seen in both complete and partial tears [Table/Fig-3]. Fluid in the SASD bursa was seen in 55.5% of patients, while subcoracoid bursal effusion was seen in 51% of patients and joint effusion was seen in 42% of patients. Hollister MS et al., concluded that the finding of fluid in the SASD bursa, especially when combined with joint effusion is highly specific and has a high positive predictive value for the presence of rotator cuff tear [11].
AC joint arthrosis is also a common associated finding in patients with rotator cuff tears and was seen in 12 of the 45 patients in our study. The mean age of patients with AC joint arthrosis in our study was 50.9 years (± 13.09), and nine of the 12 (75%) patients were above 40 years of age. These findings are consistent with the literature, suggesting that increasing age is associated with hypertrophic AC joint arthrosis, which in turn predisposes to rotator cuff tears [12].
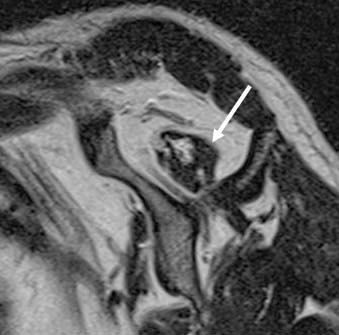
Another important associated finding with rotator cuff tear is muscle atrophy [Table/Fig-7]. As the ability of muscles to contract is lost due to atrophy, recognition of this important finding is important to predict the return of function after surgery. MRI is helpful in this regard as it can quantify the degree of muscle atrophy by assessing the occupancy ratio of the supraspinatus muscle in the supraspinatus fossa. Goutallier D et al., reported that the presence of fatty degeneration often has a significant correlation with suboptimal return of shoulder function following surgery as well as a higher risk of tear recurrence [13].
T2W sagittal image through the supraspinatus fossa showing atrophy of supraspinatus muscle belly (arrow).
Few other associated findings that were seen on MRI included subchondral cysts at the humeral head or greater tubercle, fracture of the greater tubercle, marrow oedema, Hill-Sachs and Bankart’s lesion and labral tears [Table/Fig-3]. Thus, MRI gives the most complete information about the tendon structure and possible associated disease in the shoulder joint, which may influence therapeutic decision making.
Limitation
There were certain limitations in this study. There was an unavoidable patient selection bias in this study since we included only those patients who were sufficiently symptomatic to be considered for arthroscopic shoulder surgery. This might have resulted in an overestimation of the diagnostic efficacy. Hence, it would be ideal if these findings were confirmed in a larger study with a broader range of patients. Second, as arthroscopy is an operator dependant method. Thus, misinterpretation during arthroscopy could represent a probable source of error.
Conclusion
Our study demonstrates a high sensitivity and specificity for the MRI diagnosis of both partial and full thickness rotator cuff tears and good correlation with arthroscopic findings. Arthroscopy remains the gold standard for diagnosis of rotator cuff injuries, but may not be practical in all patients. Thus, MRI offers an excellent non-invasive technique which can be used to triage patients with suspected rotator cuff injuries. MRI gives detailed information about tear size and extent, as well as providing important information about tendon retraction, muscle atrophy and fatty degeneration, all of which helps the surgeon in better planning the type of surgery and offer some prognostic information to the patient.
(Chi-square test and Cohen’s Kappa test were used to calculate p-value and kappa coefficient)
SASD – subacromial subdeltoid. SC – subcoracoid. AC – acromio-clavicular.