Case Report
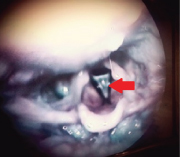
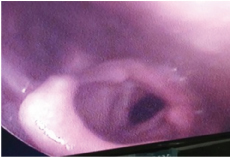
A10-year-old male child who was being treated for refractory bronchial asthma was referred to our out-patient department with complaints of breathlessness, which used to aggravate on exertion and subtle voice change which was noticed by the mother from past four to five years. There was no history of any trauma, infection or intubation. A fiberoptic laryngoscopy was done which showed a thin laryngeal web occupying 50 to 75% of the lumen [Table/Fig-1].
Cohen’s type III, thin, anterior glottic web diagnosed with fiberoptic laryngoscopy;
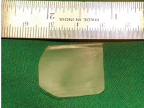
A Computed Tomography (CT) of the neck was done to assess the thickness of the web [Table/Fig-2]. It showed no subglottic extension. Patient was planned for excision of the web and placement of the silicone keel under general anaesthesia after informed written consent.
Coronal CT neck showing the glottic web.

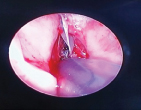
We fabricated our own laryngeal keel, making the best out of disposable cardiac catheters, silicone sheet (6″x8″x0.05″) and silicone glue. An adequate length of a hollow tubing (cardiac catheter) was cut. Placing the catheter in the centre, the entire thin silicone sheet was folded upon itself and glued together with the help of the silicone glue avoiding any air bubbles. The hollow catheter thus formed one edge of the folded sheet [Table/Fig-3].
Keel-folded silicone sheet with catheter at one edge;
The patient was intubated with relatively smaller endotracheal tube, inserted atraumatically through the available airway. Microlaryngoscopy was performed to confirm the findings. The web was lysed endoscopically using a sickle knife. Haemostasis was achieved with adrenaline soaked patties.
Topical application of Mitomycin-C (0.4 mg/ml) was done for 2 min, after which the site was irrigated with normal saline and aspirated.
The keel placement was done by the Dedo’s technique [1]. In this technique:
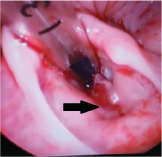
(1) Two 18 G needles (which are generally used in the blood transfusion set) were placed through the cricothyroid membrane and the thyrohyoid membrane in the midline, under endoscopic visualization [Table/Fig-4].
18G needles above and below the level of the vocal cords with prolene thread through them.;

(2) A prolene 1-0 suture was inserted through the needle placed in the cricothyroid membrane and brought out through the oral cavity. The fashioned keel was threaded over this prolene into place [Table/Fig-5].

(3) Then the same end of the suture was endoscopically inserted into the tip of the upper needle (the one in the thyrohyoid membrane) and brought out externally.
(4) Both the needles were then removed.
(5) The keel was secured in place by taking multiple knots over a button, externally on the neck [Table/Fig-6,7].
Keel inserted after excision of the web by cold dissection.
Prolene tied over a button to secure the keel in place.

The postoperative period was uneventful. Patient was kept on a course of augmentin 600 mg, pantocid 40 mg and a tapering dose of intravenous dexamethasone 4 mg for one week and then discharged.
On follow up fiberoptic laryngoscopy, after four weeks, he had minimal granulation tissue at the site where the prolene suture was tied [Table/Fig-8]. The keel was then removed endoscopically and a sofradex ointment was applied over the granulations. Patient was given a full course of dexamethasone in a tapering fashion for a month after the keel removal.
Granulations externally and at the anterior commissure at four weeks post-op;
The patient was relieved of his breathlessness but there was no major change in the quality of his voice. A fiberoptic laryngoscopy was again performed after one month of keel removal to check postoperative status [Table/Fig-9].
Post-operative view after one month of keel removal.
Discussion
The first case of a laryngeal web was described by Fleischmann in 1820 after performing autopsy on a 27-day-old infant [1]. In 1869, Zurhelle described the first living case, diagnosed by indirect laryngoscopy, in an 11-year-old boy who presented with voice anomaly [1].
Congenital laryngeal web constitutes 5% of all congenital laryngeal anomalies [2]. Most congenital webs present either at birth or in the first few months of life. Very rarely the web may present itself even in an older age group. Our patient presented with respiratory difficulty and voice change at 10 years of age however cases with more severe respiratory distress are diagnosed sooner.
A congenital laryngeal web is a rare anomaly which results from incomplete recanalization of primitive larynx during the 10th week of embryogenesis. Congenital anterior laryngeal web is one part of the spectrum of this developmental defect—the most important being laryngeal atresia [1].
Acquired lesions are more common, which may be due to inflammation caused by an infective aetiology. However, today, the main causes are iatrogenic, after intralaryngeal surgeries or a post-traumatic intubation [3].
These webs are usually found involving the anterior glottis; the larger ones also extend into the subglottis, however, sometimes, the thinner and the larger ones may be found limited only to the glottis [Table/Fig-1]. The symptoms may range from dysphonia, hoarseness, and stridor to airway obstruction [4]. Sometimes, the dysphonia goes unnoticed when subtle, and patient presents only with breathlessness, as in our case, which was initially misdiagnosed as refractory bronchial asthma.
Laryngeal web may masquerade as bronchial asthma [5] as was seen in our patient. These patients don’t respond to bronchodilators and anti-inflammatory therapy and have features of upper respiratory tract obstruction. Other differential diagnosis includes tracheal webs, tracheomalacia, tracheal stenosis, leiomyoma of trachea and functional disorder of larynx.
Although in some cases the web is found isolated, in others, it is associated with congenital defects; chromosomal (22q11 deletion) and cardiovascular anomalies [6-8].
The initial evaluation in a suspected case of a laryngeal web consists of:
(1) defining whether web is present and, if so, whether it is congenital or acquired.
(2) looking for associated anomalies.
(3) determining the best surgical and anaesthetic options for reconstruction.
When a laryngeal web is suspected, an initial evaluation by fiberoptic laryngoscopy is essential. During the fiberoptic examination, the thickness of the web, vocal cord mobility, size of the subglottic lumen, swallowing, and presence of posterior cleft in the interarytenoid region should be included. The nasal surface of the soft palate for submucosal cleft and abnormal pulsations of medialized internal carotids also should be sought for. These findings may be observed in children with chromosome 22q11 deletion (velo-cardio-facial syndrome and DiGeorge’s syndrome).
Though, we had done a CT scan for our patient, imaging may not always be required. It mainly helps in assessing the degree of subglottic stenosis and is particularly useful in children with complete atresia. It can provide information about the length and degree of stenosis along with assessment of the rest of the lower airway. However, imaging should not replace direct visual analysis, as it cannot evaluate the airway mucosa and the degree of inflammation.
Cohen’s and Benjamin’s staging of webs is currently used.
Cohen’s classification [9] defines type I to IV, based on the degree of glottic narrowing as follows:
Type I - anterior webs involving 35% or less of the glottis and are free of subglottic extension;
Type II - these webs involve 35 -50% of the glottis;
Type III - these webs involve 50-75% of the glottis and are usually thicker anteriorly and thinner posteriorly;
Type IV - these webs occupy 75-90% of the airway, they are uniformly thick with subglottic extension. Vocal cords may not be identifiable;
Types II and III may have subglottic extension. But our patient had an isolated thin type III web.
Benjamin’s classification has four degrees: glottic webs, subglottic webs, congenital interarytenoid fixation, and supraglottic webs [1]. The two classifications can be concurrently used to define a lesion.
Depending on the severity of the web, there are three options for management: (1) Observation: It is a good option for an incidental, small anterior web without any respiratory or voice problems; (2) Endoscopic management: It is ideal for thin webs without any subglottic extension; (3) Open approach: Thick webs with subglottic extension, associated with subglottic stenosis or laryngeal cleft require an open approach.
Our patient was managed via the endoscopic approach. Though we used cold instruments like sickle knife for lysis of the web, a CO2 laser is actually a better option. The CO2 laser cuts precisely, it ablates tissue with minimal surrounding damage and bleeding. An alternative flexible delivery system is now available instead of the optical one.
Traditionally, keel placement to prevent recurrence of the web has been performed through an external approach [1]. But now, this can routinely be done by an endoscopic approach in appropriately selected cases.
Open approaches have some disadvantages such as necessitating tracheotomy and at least two separate external procedures. Endoscopic methods have several advantages such as absence of an external wound, and minimal damage to normal voice and deglutition function following surgery.
Milczuk HA et al., have mentioned that the failure of endoscopic treatment is due to the presence of ‘hard’ or‘cartilaginous’ subglottic component [4]. Hence case selection for a particular approach is of utmost importance.
Unfortunately, despite excellent anatomical results, the results of voice improvement are unpredictable and often poor inspite of fine surgical techniques and rehabilitation.
Conclusion
Treatment of anterior glottic web remains a therapeutic challenge and no single approach is satisfactory. It may be suggested that the described technique of self-made keel placement can be safely used in management of thin anterior glottic web, as a first-line therapy. Also it may be used in cases with recurrent web formation. It is an easy, cost-effective, minimally invasive technique to manage thin anterior glottic webs in non-affording patients presenting at government setups, where specialized equipment may not always be available.
[1]. Nicollas R, Triglia JM, The anterior laryngeal websOtolaryngologic Clinics of North America 2008 41(5):877-88. [Google Scholar]
[2]. Amir M, Youssef T, Congenital glottic web: management and anatomical observationThe Clinical Respiratory Journal 2010 4(4):202-07. [Google Scholar]
[3]. Holland BW, Koufman JA, Postma GN, McGuirt WF, Laryngopharyngeal reflux and laryngeal web formation in patients with pediatric recurrent respiratory papillomasThe Laryngoscope 2002 112(11):1926-29. [Google Scholar]
[4]. Milczuk HA, Smith JD, Everts EC, Congenital laryngeal webs: surgical management and clinical embryologyInternational Journal of Pediatric Otorhinolaryngology 2000 52(1):1-9. [Google Scholar]
[5]. Linna O, Hyrynkangas K, Lanning P, Nieminen P, Central airways stenosis in school-aged children: differential diagnosis from asthmaActa Paediatrica 2002 91(4):399-402. [Google Scholar]
[6]. Siggers BR, Ross O, Randall C, Connett G, A rare cause of upper airway obstruction in a 5-year-old girl: a laryngeal webPediatric Anesthesia 2003 13(8):722-24. [Google Scholar]
[7]. McElhinney DB, Jacobs I, McDonald-McGinn DM, Zackai EH, Goldmuntz E, Chromosomal and cardiovascular anomalies associated with congenital laryngeal webInternational Journal of Pediatric Otorhinolaryngology 2002 66(1):23-27. [Google Scholar]
[8]. Fokstuen S, Bottani A, Medeiros PF, Antonarakis SE, Stoll C, Schinzel A, Laryngeal atresia type III (glottic web) with 22q11. 2 microdeletion: report of three patientsAmerican Journal of Medical Genetics Part A 1997 70(2):130-33. [Google Scholar]
[9]. Cohen SR, Congenital glottic webs in children: a retrospective review of 51 patientsAnnals of Otology, Rhinology & Laryngology 1985 94(6_suppl):2-16. [Google Scholar]