Leriche Syndrome: Acute Onset Painful Paraplegia of Vascular Origin with Catastrophic Consequences
Sampathkumar Mahadevappa Mahendrakar1, Harpreet Singh Sandhu2, Azizullah Hafizullah Khan3, Yunus Shafi Loya4
1 Intensivist, Department of Intensive Care, Prince Aly Khan Hospital, Nesbit Road, Mazgaon, Mumbai, Maharashtra, India.
2 FNB Trainee, Department of Intensive Care, Prince Aly Khan Hospital, Nesbit Road, Mazgaon, Mumbai, Maharashtra, India.
3 Director, Department of Intensive Care, Prince Aly Khan Hospital, Nesbit Road, Mazgaon, Mumbai, Maharashtra, India.
4 Consulting Cardiologist, Department of Cardiology, Prince Aly Khan Hospital, Nesbit Road, Mazgaon, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sampathkumar Mahadevappa Mahendrakar, 8, Prasanna, A wing, 2nd Floor, Nesbit Road, Mazgaon, Mumbai-400010, Maharashtra, India.
E-mail: drsampatkumar@gmail.com
Acute Aorto-Iliac Occlusive Disease (AIOD) is a rare clinical entity which when presents with buttock claudication, erectile dysfunction and absent femoral pulses is termed as Leriche syndrome. A 59-year-old male patient with past history of smoking and dyslipidaemia presented with acute onset lower back pain, paraplegia, intense lower limb pain and was initially evaluated for compressive myelopathy. On further clinical examination there were absent femoral pulses and Computed Tomography (CT) aortogram was done which confirmed the diagnosis of diffuse AIOD. Clinically, it is often challenging to differentiate between vascular or neurogenic origin of acute onset painful paraplegia. A high index of suspicion and careful clinical examination is therefore essential to avoid misdiagnosis of a major vascular event which can result in significant morbidity and mortality.
Aorto-iliac occlusive disease, Atherosclerosis, Erectile dysfunction
Case Report
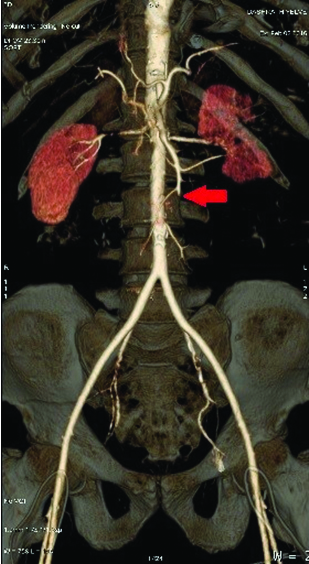
A 59-year-old male patient was admitted to Emergency Room with acute onset of lower backache, bilateral lower limb weakness, intense pain, and paraesthesia with inability to walk for preceding six hours with no history of trauma. He was a reformed smoker with a sedentary life style as a carom player and had dyslipidaemia but was not on any medications. After initial evaluation a Magnetic Resonance Imaging (MRI) of the lumbosacral spine was done which showed no evidence of compressive myelopathy. Shortly afterwards he developed dyspnoea and excruciating bilateral lower limb pain for which he was transferred to our Intensive Care Unit (ICU) for further management. Careful prodding revealed that patient had an unevaluated bilateral intermittent lower limb pain on exertion since last six months. On clinical examination patient had body mass index of 27.68 kg/m2. Heart Rate (HR) of 140/minute, non invasive blood pressure of 150/90 mmHg with absent bilateral femoral and distal lower limb pulsations while other pulsations were normal. Patient had a Respiratory Rate (RR) of 34/minute with orthopnoea, bilateral basal crepitations and 95% Oxygen Saturation (SpO2) on four litres oxygen by facemask. Both the lower limbs were cold with motor power of 0/5 at bilateral hip joints and distally with absent deep tendon reflexes but a detailed neurological exam could not be performed. Electrocardiogram showed sinus tachycardia with ST segment depression in inferolateral leads. Bedside two-dimensional echocardiogram showed global hypokinesia with left ventricular ejection fraction of 25% with a normal sized right atria and right ventricle. Routine blood investigations showed mild leucocytosis with a normal haemoglobin, renal and liver function tests. Cardiac biomarkers Creatine Kinase (CK-MB): 29.2 ng/ml. Troponin-I: 1.2 ng/ml, Brain Natriuretic Peptide (BNP): 1230 pg/ml and D-Dimer: 3590 ng/ml were elevated. He was stabilized with non invasive ventilation, antiplatelets, statins, loop diuretics, Low Molecular Weight Heparin (LMWH) and intravenous nitroglycerine. An urgent CT aortogram was done which showed complete occlusion of infra renal aorta, proximal segment of both common iliac arteries and origin of internal mesenteric artery with partial thrombosis of mid-distal segment of both common iliac, external iliac, internal iliac and both common femoral arteries along with bilateral wedge renal and splenic infarct [Table/Fig-1,2].
CT aortogram showing complete occlusion of infra-renal aorta and both common iliac arteries (red arrow) (left);

CT aortogram showing complete occlusion of infra-renal aorta and both common iliac arteries (red arrow) (right).

In view of acute onset atherosclerotic long segment thrombus, surgical intervention was planned. The patient underwent emergency bilateral trans-femoral embolectomy and about 20 cm long thrombus with diffuse atherosclerosis was removed [Table/Fig-3]. Postoperatively patient was shifted back to ICU and examination showed warm and re-perfused bilateral lower limbs with definite distal pulses but persistent motor and sensory loss. Antiplatelets and LMWH were continued along with Inj. piperacillin-tazobactum 4.5 gm intravenously in thrice daily dosing. Adequate hydration, urine output was maintained postoperatively. Repeat CT angiogram was done which showed fully re-canalised aorto-iliac and femoral flow but complete occlusion of Superior Mesenteric Artery (SMA), 7.5 cm distal to its origin [Table/Fig-4]. Therapeutic doses of anticoagulants were continued and patient was weaned off mechanical ventilation two days post embolectomy. He was subsequently discharged from ICU on seventh postoperative day on antiplatelets and oral anticoagulants. His clinical condition improved gradually but his overall condition remains dismal in view of persistent paraparesis.
Surgically extracted long segment thrombus.

Postoperative CT-aortogram showing fully re-canalised flow in infrarenal aorta and common iliac arteries but occluded SMA (red arrow).
Discussion
Atherosclerosis involving aorto-iliac segments is commonly a chronic condition presenting with lower limb claudication. Major risk factors are dyslipidaemia, male gender, smoking, diabetes mellitus, and hypertension. AIOD is a rare clinical entity which when presenting with buttock claudication, erectile dysfunction and absent femoral pulses is termed as Leriche syndrome [1]. Acute paraplegia due to reduced blood flow of artery of Adamkiewicz’s causing spinal cord ischemia is a known complication in Leriche syndrome [2]. Clinically it is often challenging to differentiate between vascular or neurogenic origin of acute onset painful paraplegia. A high index of suspicion and careful clinical examination is therefore essential to avoid misdiagnosis of a major vascular event which can result in significant morbidity and mortality [3].
Painful paraplegia is a frequently encountered clinical syndrome with trauma and spinal cord compression as a common aetiology. Atherosclerosis is a complex degenerative disease with multiple risk factors including hypertension, hyperlipidaemia, hyperglycaemia, cigarette smoking, hyper-homocysteinemia [4]. Sudden critical limb ischemia due to atherosclerosis of aorto-iliac segments is a rare entity in which multiple arterial segments are involved and carries a high risk of morbidity and mortality [3,5]. Cigarette smoking and hypercholesterolemia are more commonly seen with AIOD than in patients with infra inguinal thrombosis [6].
Our patient had an underlying untreated dyslipidaemia and history of smoking with unevaluated intermittent claudication. Patient developed acute onset dyspnoea requiring ICU admission for acute coronary syndrome which has a high incidence in patients with peripheral arterial disease [7]. The absent femoral pulses on clinical examination clinched the diagnosis of vascular origin of paraplegia in this case. Urgent CT-aortogram confirmed the diagnosis and helped in decision making for appropriate management [8]. Management strategies for such patients include anticoagulants, thrombolysis, embolectomy, endovascular techniques and extra-anatomical bypass with varying degrees of success [9]. Although, prompt surgical embolectomy was done, but the AIOD was associated with widespread thrombotic catastrophe involving coronary arteries and SMA in this case.
AIOD might have different presentations in patients ranging from erectile dysfunction and paraplegia to sudden multisystem vaso-occlusive catastrophe [10-13]. The sudden onset paraparesis with diffuse atherosclerotic involvement of coronary and splanchnic circulation due to long segment thrombus occluding aorta complicated management in this case. AIOD could have been diagnosed earlier if careful examination of peripheral pulses and bilateral lower limbs had been done in initial evaluation of paraplegia. Thrombolysis and endovascular repair was not preferred as initial management strategy due to diffuse long segment nature of AIOD.
Conclusion
Through this case report we would like to emphasize the need for careful history seeking risk factors and clinical examination in the cases of acute onset paraplegia especially of distal lower pulses. Acute AIOD should be considered as close differential diagnosis of acute onset paraplegia and help sought with imaging techniques whenever in doubt in view of its high morbidity and mortality.
[1]. Leriche R, Morel A, The syndrome of thrombotic obliteration of the aortic bifurcationAnn Surg 1948 127:193-206. [Google Scholar]
[2]. Zankl AR, Blessing E, Volz HC, Krumsdorf U, Katus HA, Andrassy M, Neurological symptoms in acute Leriche’s syndromeClin Res Cardiol 2010 99:459-62. [Google Scholar]
[3]. Surowiec SM, Isiklar H, Sreeram S, Weiss VJ, Lumsden AB, Acute occlusion of the abdominal aortaAm J Surg 1998 176:193-97. [Google Scholar]
[4]. vanRooy M-J, Pretorius E, Obesity, hypertension and hypercholesterolemia as risk factors for atherosclerosis leading to ischemic eventsCurr Med Chem 2014 21:2121-29. [Google Scholar]
[5]. Dossa CD, Shepard AD, Reddy DJ, Jones CM, Elliott JP, Smith RF, Acute aortic occlusion. A 40-year experienceArch Surg 1994 129:603-08. [Google Scholar]
[6]. Rueda CA, Nehler MR, Perry DJ, McLafferty RB, Casserly IP, Hiatt WR, Patterns of artery disease in 450 patients undergoing revascularization for critical limb ischemia: implications for clinical trial designJ Vasc Surg 2008 47:995-1000. [Google Scholar]
[7]. Das JR, Eberhardt RT, Contemporary risk assessment and cardiovascular outcomes in peripheral arterial diseaseCardiovasc Hematol Disord Drug Targets 2013 13:185-96. [Google Scholar]
[8]. Budovec JJ, Pollema M, Grogan M, Update on multidetector computed tomography angiography of the abdominal aortaRadiol Clin North Am 2010 48:283-309. [Google Scholar]
[9]. Indes JE, Pfaff MJ, Farrokhyar F, Brown H, Hashim P, Cheung K, Clinical outcomes of 5358 patients undergoing direct open bypass or endovascular treatment for aortoiliac occlusive disease: a systematic review and meta-analysisJ Endovasc Ther 2013 20:443-55. [Google Scholar]
[10]. Lee W-J, Cheng Y-Z, Lin H-J, Leriche syndromeInt J Emerg Med 2008 1(3):223-23. [Google Scholar]
[11]. Liao SL, Luthra M, Rogers KM, Leriche syndromeJournal of the American College of Cardiology 2009 54(19):e11 [Google Scholar]
[12]. Frederick M, Newman J, Kohlwes J, Leriche syndromeJ Gen Intern Med 2010 25(10):1102-04. [Google Scholar]
[13]. McCoy CE, Patierno S, Lotfipour S, Leriche syndrome presenting with multisystem vaso-occlusive catastropheWest J Emerg Med 2015 16(4):583-86. [Google Scholar]