Upper Gastrointestinal Bleeding Due to Idiopathic Oesophageal Ulceration in the Era of HAART: A Vanishing yet Pernicious Aetiology
Sofia Nigar1, Tagore Sunkara2, Mel A Ona3, Vinaya Gaduputi4, Madhavi Reddy5
1 Fellow, Department of Gastroenterology, The Brooklyn Hospital Center, Brooklyn, New York, USA.
2 Fellow, Department of Gastroenterology, The Brooklyn Hospital Center, Brooklyn, New York, USA.
3 Fellow, Department of Gastroenterology, The Brooklyn Hospital Center, Brooklyn, New York, USA.
4 Attending Physician, Department of Gastroenterology, SBH Health System, Bronx, New York, USA.
5 Attending Physician, Department of Gastroenterology, The Brooklyn Hospital Center, Brooklyn, New York, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tagore Sunkara, 240 Willoughby St, 16G, Brooklyn, New York, USA.
E-mail: tagoresunkara@hotmail.com
Oesophageal ulcers are a rare cause of upper Gastrointestinal Bleeding (GIB). In patients with Acquired Immune Deficiency Syndrome (AIDS), oesophageal diseases including oesophageal ulcers are very common. Idiopathic Oesophageal Ulcers (IOU) comprises a subgroup of oesophageal ulcers with no identifiable cause. IOU mainly present as odynophagia, retrosternal chest pain, decreased oral intake, and weight loss. Upper GIB is a rare presentation. In the era of Highly Active Anti Retroviral Therapy (HAART), with improvement in CD4 count, this entity is almost forgotten.
Acquired immune deficiency syndrome, Anti retroviral therapy, Human immunodeficiency virus, Ulcer
Case Report
A 49-year-old man with AIDS and coronary artery disease (non compliant with HAART, aspirin and clopidogrel) presented to the hospital with right-sided chest pain, epigastric pain, and right upper quadrant abdominal pain. Vitals on admission were stable with blood pressure of 110/67 mmHg, pulse of 79, respiratory rate of 18/min and 100% oxygen saturation on room air. Patient had a pertinent history of admission to another institution a week earlier for odynophagia for which he had undergone an Esophagogastroduodenoscopy (EGD) that showed multiple non bleeding ulcers in the middle third of the oesophagus and one superficial pyloric ulcer. Patient was started on proton pump inhibitor therapy. Histology was negative for any infectious aetiology. Patient subsequently had also developed unstable angina necessitating an urgent left heart catheterization with placement of a drug eluting stent.
Patient during this index presentation reported to have been non compliant with HAART medications over the preceding three months. Physical examination revealed a soft abdomen with tenderness in the epigastric and right upper quadrant regions. Patient was noted to have mild normocytic, normochromic anemia with a haemoglobin level of 10.4 gm/dl. His CD4 count was <20 cells/mcL (normal range: 490-1740 cells/mcL) and viral load was 47784 copies/ml. Acute coronary syndromes were ruled out.
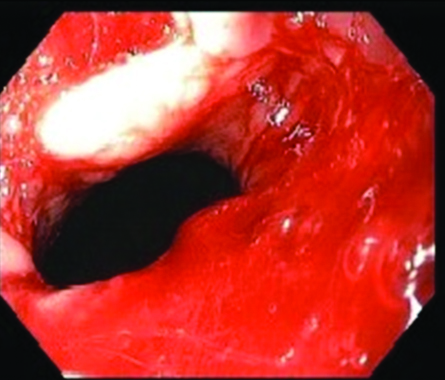
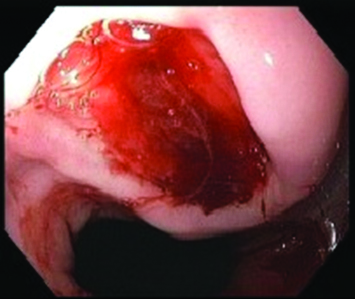
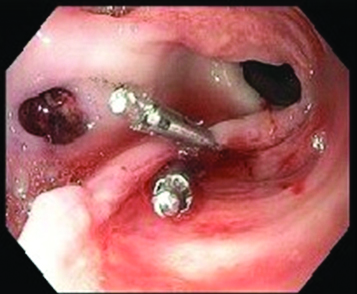
While in hospital, patient developed hematemesis with a drop in hemoglobin to 7.9 gm/dl. A diagnostic EGD showed multiple oesophageal ulcers with a single actively bleeding ulcer [Table/Fig-1,2]. Hemostasis was achieved with injection of 1:10000 dilute epinephrine, thermal therapy with heater probe and application of two resolution clips [Table/Fig-3]. Patient was continued on acid-suppression therapy and was also started on sucralfate. Patient resumed HAART medications and was counseled to remain adherent to it. The patient clinically improved and was subsequently discharged. Patient was seen in the gastroenterology clinic as a follow up case two weeks after discharge from the hospital. Patient denied any further complaints of chest pain, abdominal pain, nausea, vomiting, hematemesis, dysphagia or odynophagia since discharge. Patient claimed, he has been compliant with HAART, aspirin and clopidogrel. Patient is scheduled for a repeat EGD eight weeks from the index EGD.
Active bleeding seen in the oesophagus.
Oesophageal ulcer with oozing of blood. (All Image left to right).
Hemostasis achieved with resolution clips.
Discussion
One of the common cause for oesophageal diseases in Persons with AIDS (PWA) is oesophageal ulcerations. Oesophageal ulcerations can be caused from infections, tumors, medications or during HIV seroconversion, IOU is diagnosed when all known causes of oesophageal ulcerations are excluded. These ulcers can be single or multiple in number and vary in depth. Steroids have been the preferred treatment but complete healing has been seen with initiation of HAART. They rarely cause serious complications like upper GIB, oesophageal perforations or rupture. We herein describe a rare case of IOU presenting as hematemesis in the era of HAART.
Symptoms from oesophageal diseases are common in PWA. Forty percent of PWA has oesophageal diseases [1], and the most common cause is candida infection [2]. Majority of patients with oesophageal symptoms who fail anti fungal treatment have oesophageal ulcers. Oesophageal ulcers in PWA can be caused by various aetiological agents including Cytomegalovirus (CMV), Herpes Simplex Virus (HSV), kaposi’s sarcoma, lymphoma and medications. Oesophageal ulcers have also been reported during HIV seroconversion.
IOUs are diagnoses of exclusion, when routine tests and endoscopy with histology rule out other possible aetiologies. Patients with IOU often present with odynophagia, retrosternal chest pain, decreased oral intake and weight loss. Upper GIB, oesophageal perforation or rarely, oesophageal rupture may be the presenting symptom. Wilcox CM et al., showed that these ulcers have a heterogeneous appearance on endoscopy [3]. They present as a single or multiple ulcers in the mid to distal oesophagus, with about a third measuring ≤1 cm and about a third being giant ulcers measuring ≥2 cm in size. The ulcers are usually of shallow to intermediate depth. Few cases of IOU with undermined epithelium, leading to mucosal bridges have also been described [3,4]. Histologically, these ulcers are lined by granulation tissue, with acute and chronic inflammatory cells, including eosinophils. The ulcers can also extend into the muscle layer. The pathophysiology of the IOU is not fully understood. The presence of HIV in these ulcers has been documented. Inflammatory infiltration and apoptotic cells were found in these ulcers and HIV induced apoptosis of oesophageal mucosa appears to play a role in the pathogenesis of IOU [5,6].
Steroids have historically been the treatment of choice [4]. Oral prednisone has been used with success. Intralesional steroids have been shown to cause rapid improvement in symptoms within hours; however, symptoms tend to recur in few days requiring repeat therapy. Intravenous steroids are comparable to oral steroids in providing symptomatic improvement over short-term (36-48 hours), but long term relief is better achieved with a tapering course of oral steroids. However, complications such as Cytomegalo virus (CMV) gastritis and oesophagitis, pneumocystis pneumonia, and tuberculosis, have been reported after the use of steroids for treatment of IOU.
Thalidomide has also been reported as an effective and well tolerated alternative treatment for IOU [7]. Misoprostol, when used as a suspension in viscous lidocaine, has shown rapid symptom improvement in two to three days, with subsequent mucosal healing [8]. More recently, the healing of IOU has been achieved with HAART alone [9-11]. The finding of HIV in these ulcers and HIV-induced apoptosis as a possible mechanism involved in their development, lends theoretical support to the use of HAART in the treatment of IOU. This option is also more attractive given the many complications associated with use of steroids. In a study by Kotler DP et al., the mean CD4 count associated with IOU was 54 cells/mcL of blood [4].
Conclusion
With the advent of HAART and improvement in CD4 counts, the incidence of IOU has declined substantially. Whether this diagnosis is relevant in patients with immunocompromised states from other causes, such as stem cell or renal transplantation, is yet to be determined. Nevertheless, the clinician must be familiar with this entity, in order to facilitate timely diagnosis and treatment.
[1]. Laine L, Bonacini M, Esophageal disease in human immunodeficiency virus infectionArch Intern Med 1994 154(14):1577-82. [Google Scholar]
[2]. Varsky CG, Yahni VD, Freire MC, Patrizio E, Balbo V, Benetucci J, Esophageal pathology in patients with the AIDS virus. Etiology and diagnosisActa Gastroenterol Latinoam 1991 21(2):67-83. [Google Scholar]
[3]. Wilcox CM, Straub RF, Alexander LN, Clark WS, Etiology of esophageal disease in human immunodeficiency virus-infected patients who fail antifungal therapyAm J Med 1996 101(6):599-604. [Google Scholar]
[4]. Kotler DP, Reka S, Orenstein JM, Fox CH, Chronic idiopathic esophageal ulceration in the acquired immunodeficiency syndrome. Characterization and treatment with corticosteroidsJ Clin Gastroenterol 1992 15(4):284-90. [Google Scholar]
[5]. Lv B, Cheng X, Gao J, Zhao H, Chen L, Wang L, Human immunodeficiency virus (HIV) is highly associated with giant idiopathic esophageal ulcers in acquired immunodeficiency syndrome (AIDS) patientsAm J Transl Res 2016 8(10):4464-71. [Google Scholar]
[6]. Houghton JM, Korah RM, Kim KH, Small MB, A role for apoptosis in the pathogenesis of AIDS-related idiopathic esophageal ulcersJ Infect Dis 1997 175(5):1216-19. [Google Scholar]
[7]. Louvel D, Musso S, Métivier S, Croizet O, Rouquet RM, Massipet P, Idiopathic esophageal ulceration associated with human immunodeficiency virus infection: efficacy of thalidomide treatmentEndoscopy 1996 28(5):471-72. [Google Scholar]
[8]. Adeoti AG, Vega KJ, Dajani EZ, Trotman BW, Kloser PC, Idiopathic esophageal ulceration in acquired immunodeficiency syndrome: successful treatment with misoprostol and viscous lidocaineAm J Gastroenterol 1998 93(11):2069-74. [Google Scholar]
[9]. Hamada Y, Nagata N, Honda H, Teruya K, Gatanaga H, Kikuchi Y, Idiopathic oropharyngeal and esophageal ulcers related to HIV infection successfully treated with antiretroviral therapy aloneIntern Med 2013 52(3):393-95. [Google Scholar]
[10]. Bromberg DJ, Gill JA, Idiopathic esophageal ulcers in AIDS completely healed with highly active anti-retroviral therapyACG Case Rep J 2015 2(3):127-28. [Google Scholar]
[11]. Nishijima T, Tsukada K, Nagata N, Watanabe K, Teruya K, Gatanaga H, Antiretroviral therapy alone resulted in successful resolution of large idiopathic esophageal ulcers in a patient with acute retroviral syndromeAIDS 2011 25(13):1677-79. [Google Scholar]