Periarthritis (PA) shoulder is characterised by insidious onset, progressive pain and loss of active and passive mobility in the glenohumeral joint [1]. The annual incidence of PA is between 3%-5% in the general population and as high as 20% among individuals with diabetes [2]. It usually develops between the ages of 40 to 70 years [1]. The underlying pathology is soft tissue fibrosis and inflammation of the rotator interval, capsule and ligaments [3]. There has been an acknowledgement of the absence of a specific definition and of diagnostic criteria for PA which both the British Elbow and Shoulder Society and American Shoulder and Elbow Surgeons have endeavoured to rectify [4,5].
A plethora of treatment options have been recommended which include benign neglect, oral corticosteroids, intra-articular injection of corticosteroids, intra-articular injection of hyaluronic acid, physical therapy exercises, deep heat modalities, manipulation under anesthesia, hydrodilation, arthroscopic release but the best treatment is still subjected to debate [6,7]. Ultrasonic therapy is used as an intervention for its physiological effects which include augmentation of blood flow, increased capillary permeability and tissue metabolism, enhancement of tissue extensibility, elevation of pain threshold, and alteration of neuromuscular activity leading to muscle relaxation [8]. The application of intra-articular corticosteroid injection is one of the commonly used approaches in PA shoulder [9]. PRP has emerged as a new technology which is believed to stimulate revascularization of soft tissue and increase the concentration of growth factors to improve and accelerate tendon healing. It is defined as a sample of autologous blood with concentrations of platelets above baseline values [10]. Given this background of inconclusive evidence for treatment modalities and recent introduction of PRP as a biological agent promoting healing, there is a need to examine the role of PRP and compare its efficacy with steroid injections and ultrasonic therapy.
Materials and Methods
This was a randomised comparative study conducted at a tertiary care hospital (Safdarjang Hospital, New Delhi) in an urban set up from September 2011 to January 2013. The study project was approved by the Hospital’s Ethics Committee. This study was conducted with the internal resources of the department without any external funding.
The inclusion criteria were age over 18 years, shoulder pain for at least one month associated with more than one-third loss of active shoulder flexion, abduction and external rotation, normal antero-posterior radiographs of the glenohumeral joint in neutral rotation, willingness to participate in study and forgo any other concomitant treatment modality. The exclusion criteria were unwillingness to participate in the study, intrinsic glenohumeral pathology, history of shoulder trauma/surgery, clinical evidence of complex regional pain syndrome, history of injection in the involved shoulder joint during the preceding six months or non-steroidal anti-inflammatory drugs intake in last seven days, patients with haematological disorders or on antiplatelet or anticoagulant therapy, patients with chronic diseases and pregnancy or breastfeeding.
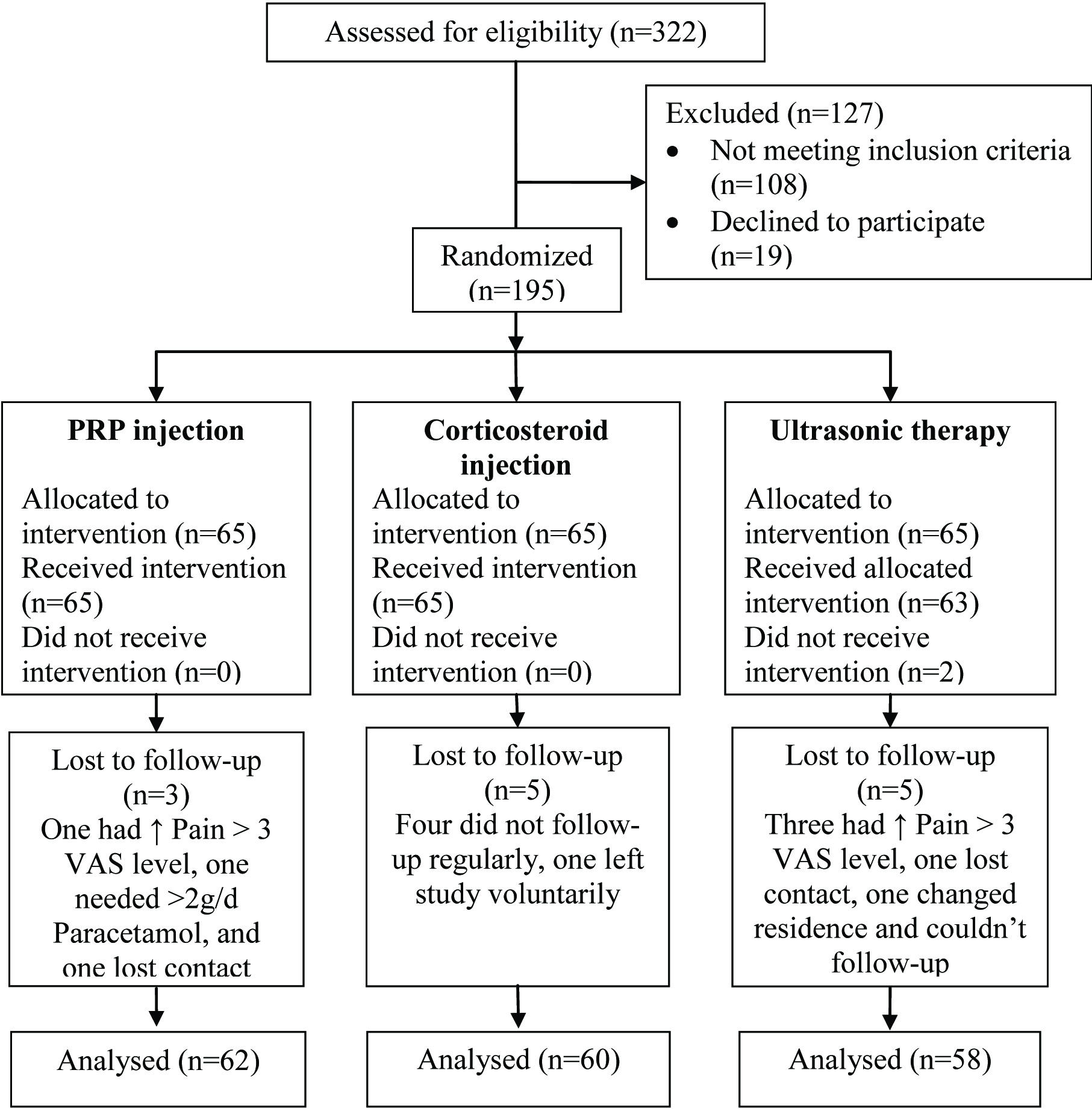
A total of 195 subjects fulfilling the inclusion/exclusion criterion and willing to participate in the study were randomised into three groups (A, B and C) using computer generated random number table. All subjects were given the participant information sheet which had information regarding the study including withdrawal rights and informed consent was obtained.
Subjects in Group A and B received one intra-articular injection of 2 ml of PRP and 2 ml (80 mg) of methylprednisolone acetate respectively by anterior approach. Asepsis was maintained throughout the procedure. Adverse effects were noted during each injection procedure. After injection, subjects were sent home with instructions to limit the movement of the shoulder joint for at least 48 hours and to use cold compress and paracetamol as rescue medication for pain. After two days exercises were started. Patients in Group C received seven minutes of ultrasonic therapy (1.5 W/ cm2, 1 MHz, continuous mode) on alternate days for 14 days and exercises were started from first day. All participants (Groups A, B and C) were taught a 10 minute exercise therapy program comprising of pendulum exercise, stretching, active assisted and active range of motion exercises for shoulder flexion, abduction, external and internal rotation. They were instructed to perform exercises twice daily at home. Gentle and short duration of exercise were advised to maintain adherence and compliance was checked by weekly telephonic calls. After baseline evaluation and intervention, all subjects were followed up at 3, 6 and 12 weeks. All examinations were performed by a blinded assessor who was also a physiatrist and subjects were instructed not to reveal any details about their treatment to the assessor. Primary outcome measure used was improvement in active range of motion (assessed using clinical goniometer) and secondary outcome measures used were Visual Analogue Scale (VAS) for pain and a shortened version of Disabilities of the Arm, Shoulder and Hand (QuickDASH) for function [11]. The end points of the study included occurrence of one of the following: completion of 12 weeks follow up, increase in pain by three levels on VAS and subject not willing to continue in the study or had to take tablet paracetamol more than 2 gm/day on three days/week for more than two weeks.
The process of PRP preparation was finalised after consultation with Departments of Biochemistry and Haematology. Sterile nature of the preparation was verified by culture at Department of Microbiology.
Statistical Analysis
The data was managed using Microsoft Excel and analysed using STATA (Version 9) for Windows. Chi-square test was used for comparison of binomial variables. All continuous data were expressed as mean and standard deviation of mean. Within each group, change in the mean values of continuous variables with time was compared using repeated measure analysis of variance (ANOVA) test. One way ANOVA was applied to compare mean values between the groups for each domain of continuous variables and post-hoc tests (Bonferroni correction) were used to determine significant difference between each of the groups. Results were considered significant at 5% level of significance, i.e., p<0.05.
Results
A total of 322 subjects with complaints of shoulder pain associated with restriction of motion were assessed for eligibility. A total of 195 subjects were found eligible and randomised to three groups of 65 each [Table/Fig-1]. Two participants in group C did not receive complete session of ultrasonic therapy. Thirteen participants (three in Group A; five in Group B and C) were lost to follow up. Analysis of 180 subjects (86 males; 94 females) who completed the study was done.
Baseline demographic and clinical characteristics of each group are given in [Table/Fig-2]. No significant differences were observed between the groups in terms of mean age, sex distribution, involvement of dominant side, duration of symptoms and shoulder range of motion in all planes except extension. During the study, no major complications were observed in subjects who received intra-articular injections. Self limiting post injection pain (less than three levels in VAS) was observed in one subject in PRP group and two in steroid group.
Patient demographics and baseline characteristics.
| PRP (n=62) | Steroid (n=60) | Ultrasonic (n=58) | p-value |
|---|
| Sex, n (%) |
| Male | 34 (54.8) | 29 (48.3) | 23 (39.7) | 0.249 |
| Female | 28 (45.2) | 31 (51.7) | 35 (60.3) |
| Age, years |
| Mean (SD) | 51.9 (10.1) | 52.7 (8.6) | 51.2 (11.7) | 0.723 |
| (Range) | (30-72) | (37-72) | (27-75) |
| Side involved, n (%) |
| Dominant | 36 (58.1) | 34 (56.7) | 36 (62.1) | 0.826 |
| Non-dominant | 26 (41.9) | 26 (43.3) | 22 (37.9) |
| Duration of symptoms, months |
| Mean (SD) | 4.1 (2.5) | 5.2 (2.8) | 4.7 (2.1) | 0.059 |
| Abduction, Mean (SD) |
| Active | 90.1 (19.0) | 90.6 (17.6) | 88.5 (14.9) | 0.800 |
| Passive | 95.9 (19.5) | 96.2 (17.1) | 95.2 (12.1) | 0.943 |
| Flexion, Mean (SD) |
| Active | 95.5 (21.0) | 96.7 (19.7) | 97.2 (16.7) | 0.878 |
| Passive | 102.3 (19.7) | 102.6 (18.6) | 102.5 (17.4) | 0.995 |
| Ext Rot, Mean (SD) |
| Active | 34.5 (19.0) | 34.4 (15.9) | 33.9 (15.6) | 0.982 |
| Passive | 38.2 (18.9) | 38.0 (16.1) | 38.0 (16.3) | 0.997 |
| Int Rot, Mean (SD) |
| Active | 21.9 (14.1) | 21.8 (12.8) | 21.3 (10.2) | 0.832 |
| Passive | 26.5 (14.4) | 26.7 (15.4) | 28.0 (15.9) | 0.800 |
| Extension, Mean (SD) |
| Active | 35.8 (8.9) | 32.0 (10.4) | 28.6 (9.6) | <0.001* |
| Passive | 41.0 (9.4) | 37.0 (11.4) | 32.4 (9.6) | <0.001* |
Ext Rot: External Rotation; Int Rot: Internal Rotation
Statistical test: Sex and Side involved-Chi-square test;
Age, Duration of symptoms, Abduction, Flexion, Ext Rot, Int Rot, Extension - One way ANOVA with Bonferroni correction
Within groups, there was significant improvement in the mean active range of shoulder abduction, flexion, external rotation and internal rotation at each follow up interval in all the groups when compared to the baseline. PRP treatment resulted in significant improvement over steroid injection and ultrasonic therapy in the mean active range of shoulder abduction, flexion, external rotation and internal rotation at 12 weeks and not at earlier periods of assessment [Table/Fig-3]. Steroid injection resulted in significant improvement over ultrasonic therapy in the mean active range of shoulder abduction, flexion and internal rotation at 12 weeks but not in external rotation. Since, there were significant differences in the mean active range of extension even at baseline, no meaningful conclusions could be made with regard to differences between the three groups at any follow up interval. Analysis of passive range of shoulder motion showed improvements similar to active motion, with significant improvement seen at 12 weeks [Table/Fig-4].
Active range of motion of shoulder in degrees {Mean (SD)} in the three study groups at baseline, 3 weeks, 6 weeks and 12 weeks.
| | PRP (n=62) | Steroid (n=60) | Ultrasonic (n=58) | p-value |
|---|
| Abduction | Baseline | 90.1 (19.0) | 90.6 (17.6) | 88.5 (14.9) | 0.800 |
| 3 weeks | 107.1 (18.6) | 104.8 (16.9) | 103.6 (13.1) | 0.499 |
| 6 weeks | 124.1 (20.8) | 121.6 (17.0) | 117.6 (15.8) | 0.141 |
| 12 weeks | 142.3 (22.9) | 129.7 (21.8) | 117.3 (16.0) | <0.001* |
| Flexion | Baseline | 95.5 (21.0) | 96.7 (19.7) | 97.2 (16.7) | 0.878 |
| 3 weeks | 111.3 (13.9) | 112.0 (16.9) | 112.2 (15.3) | 0.939 |
| 6 weeks | 128.7 (12.5) | 126.3 (16.0) | 124.7 (15.8) | 0.322 |
| 12 weeks | 145.5 (13.5) | 133.1 (18.5) | 124.8 (15.2) | <0.001* |
| External Rotation | Baseline | 34.5 (19.0) | 34.4 (15.9) | 33.9 (15.6) | 0.982 |
| 3 weeks | 49.4 (16.1) | 48.1 (17.1) | 47.6 (16.7) | 0.834 |
| 6 weeks | 65.2 (14.3) | 61.8 (15.7) | 60.6 (15.9) | 0.236 |
| 12 weeks | 80.2 (13.8) | 71.4 (18.3) | 65.0 (18.6) | <0.001* |
| Internal Rotation | Baseline | 21.9 (14.1) | 21.8 (12.8) | 21.4 (10.2) | 0.973 |
| 3 weeks | 33.8 (14.3) | 34.1 (13.5) | 33.5 (10.1) | 0.973 |
| 6 weeks | 46.4 (12.3) | 45.3 (12.3) | 43.9 (11.5) | 0.549 |
| 12 weeks | 57.5 (10.7) | 50.2 (13.4) | 45.6 (13.8) | <0.001* |
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group
Passive range of motion of shoulder in degrees {Mean (SD)} in the three study groups at baseline, 3 weeks, 6 weeks and 12 weeks.
| | PRP (n=62) | Steroid (n=60) | Ultrasonic (n=58) | p-value |
|---|
| Abduction | Baseline | 95.9 (19.5) | 96.2 (17.1) | 95.2 (12.1) | 0.943 |
| 3 weeks | 112.8 (18.4) | 110.7 (16.2) | 109.4 (12.8) | 0.498 |
| 6 weeks | 130.6 (19.9) | 127.3 (16.7) | 123.5 (16.2) | 0.098 |
| 12 weeks | 148.3 (21.5) | 135.9 (21.1) | 123.9 (16.2) | <0.001* |
| Flexion | Baseline | 102.3 (19.7) | 102.6 (18.6) | 102.5 (17.4) | 0.995 |
| 3 weeks | 117.6 (13.1) | 118.0 (16.9) | 118.9 (15.9) | 0.881 |
| 6 weeks | 134.8 (11.6) | 131.4 (15.4) | 129.7 (15.6) | 0.141 |
| 12 weeks | 151.2 (12.2) | 138.0 (17.5) | 129.3 (14.7) | <0.001* |
| External Rotation | Baseline | 38.2 (18.9) | 38.0 (16.1) | 38.0 (16.3) | 0.997 |
| 3 weeks | 53.9 (15.7) | 52.3 (16.6) | 52.8 (16.6) | 0.865 |
| 6 weeks | 69.7 (14.1) | 66.3 (15.4) | 65.6 (16.3) | 0.295 |
| 12 weeks | 85.9 (12.8) | 76.5 (17.8) | 69.7 (18.4) | <0.001* |
| Internal Rotation | Baseline | 26.5 (14.4) | 26.7 (15.4) | 28.0 (15.9) | 0.832 |
| 3 weeks | 38.9 (14.1) | 38.9 (12.5) | 38.7 (10.1) | 0.995 |
| 6 weeks | 50.8 (11.2) | 49.3 (11.5) | 48.4 (11.3) | 0.489 |
| 12 weeks | 60.4 (8.5) | 53.9 (12.6) | 49.1 (13.4) | <0.001* |
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group
VAS and QuickDASH scores showed a similar trend as in range of motion [Table/Fig-5] with significant improvement at each follow up interval in all the groups when compared to baseline and significant difference between the three groups at six and 12 weeks follow up. Post-hoc test with Bonferroni correction however showed that at six weeks significant improvement was seen only between PRP and ultrasonic group.
Visual Analogue Scale (VAS) and QuickDASH values in the three study groups at baseline, 3 weeks, 6 weeks and 12 weeks.
| Baseline | 3 weeks | 6 weeks | 12 weeks |
|---|
| VAS | QuickDASH | vas | QuickDASH | VAS | QuickDASH | VAS | QuickDASH |
|---|
| PRP (n=62) | 8.4±1.4 | 83.5±14.3 | 6.4±1.6 | 63.7±16.4 | 4.2±1.9 | 41.6±18.7 | 1.9±1.8 | 18.7±18.2 |
| Steroid (n=60) | 8.6±1.4 | 85.7±14.3 | 6.4±1.5 | 64.3±14.8 | 4.6±1.5 | 45.7±15.4 | 3.4±2.2 | 34.0±22.0 |
| Ultrasonic (n=58) | 8.9±1.4 | 88.6±13.6 | 6.6±1.4 | 65.9±14.0 | 4.9±1.4 | 48.9±13.6 | 4.5±2.0 | 45.2±20.0 |
| p-value | 0.144 | 0.144 | 0.723 | 0.723 | 0.045* | 0.045* | <0.001* | <0.001* |
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group
Discussion
Age of participants in the study was in range of 29-75 years with mean of 51.9±10.1 and similar trend has been reported in literature [1]. In this study, PA was seen more in females (52.2%) than males and this is similar to previous studies [12]. There was higher prevalence in the involvement of dominant side (106, 58.9%) as compared to the non dominant side; though, majority of available literature shows a higher prevalence of involvement of non dominant side [1]. In this study, PRP treatment resulted in statistically significant improvements over corticosteroid and ultrasonic therapy in active as well as passive range of motion of shoulder, pain (VAS) and function (QuickDASH) at 12 weeks. At six weeks, PRP treatment resulted in statistically significant improvements over ultrasonic therapy in VAS and QuickDASH. No major adverse effects were observed. However, it must be borne in mind that all the intervention groups were instructed to perform home based exercise therapy.
The uniqueness of this study was the group receiving PRP which was prepared using a simple technique and comparison of its outcome with conventionally used therapeutic strategies. Total number of platelets in PRP preparation was 6.1±1.6 times higher than whole blood values. Our study demonstrates that PRP can be prepared by a simple technique and is better than steroid and ultrasonic therapy in relieving pain, improving range of motion and function. Evidence for use of PRP in clinical conditions is growing [13,14] and our study adds to the pool of this growing literature. Subjects receiving steroid injections showed improvement in range of motion, pain and function and similar improvement has been reported in previous studies [15]. Systematic review by Griesser MJ et al. showed significant but transient improvement in abduction and forward elevation and significant short as well as long term diminution of pain measured by VAS and Shoulder Pain and Disability Index (SPADI) [15]. In our study, improvement of range of motion is seen in abduction, forward elevation (flexion) and rotation. Similar improvement in motion has also been reported in other studies [16-18]. Role of ultrasonic therapy in PA shoulder is still ambiguous [19] and in our study subjects who received ultrasonic therapy had improvement in outcome parameters but significantly less than PRP and steroid injection groups. Also, these subjects had to visit the hospital on alternate days for two weeks to receive ultrasonic therapy, whereas in other groups subjects visited the hospital only once for intervention.
Strengths of study include randomisation to eliminate selection bias and support the internal validity of the study, assessment of range of motion with goniometer, which has high intratester reliability [20], and assessment of outcome by a blinded investigator to minimise bias.
Limitation
However, there are several limitation to the present study. No cost analysis was done in the study. Our study included patients from all stages of PA and further studies are warranted to compare effectiveness at different stages of PA. Also, the effect of single injection versus series of injection needs to be assessed as multiple injections were not given. There is an incomplete understanding of the natural history of PA shoulder and hence long term studies (52 weeks or more) are necessary to truly understand how intervention affects course of disease. Our study duration was limited to only 12 weeks, so long term efficacy is not known. Further, role of musculoskeletal US guided injections could be a scope for future studies.
Conclusion
This study highlights the growing importance of PRP in chronic musculoskeletal conditions like PA shoulder, especially in clinical scenarios where steroid is contraindicated or refused by the patient. In our study, single injection of PRP resulted in significant improvement in range of shoulder motion, pain and function than steroid or ultrasonic therapy in patients with PA shoulder.
Ext Rot: External Rotation; Int Rot: Internal Rotation
Statistical test: Sex and Side involved-Chi-square test;
Age, Duration of symptoms, Abduction, Flexion, Ext Rot, Int Rot, Extension - One way ANOVA with Bonferroni correction
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group
Statistical test: One way ANOVA with Bonferroni correction between groups and repeated ANOVA within group