Sturge Weber Syndrome: A Case Study
Mahesh Neerupakam1, Podduturi Sanjay Reddy2, Beeraboina Anand Babu3, Guttikonda Vamsi Krishna4
1 Reader, Department of Oral Medicine and Radiology, Lenora Institute of Dental Sciences, Rajanagaram, Rajahmundry, Andhra Pradesh, India.
2 Professor, Department of Oral Medicine and Radiology, Lenora Institute of Dental Sciences, Rajanagaram, Rajahmundry, Andhra Pradesh, India.
3 Senior Lecturer, Department of Oral Medicine and Radiology, Lenora Institute of Dental Sciences, Rajanagaram, Rajahmundry, Andhra Pradesh, India.
4 Postgraduate Student, Department of Oral Medicine and Radiology, Lenora Institute of Dental Sciences, Rajanagaram, Rajahmundry, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mahesh Neerupakam, Reader, Department of Oral Medicine and Radiology, Lenora Institute of Dental Sciences, Rajanagaram, Rajahmundry-533294, Andhra Pradesh, India.
E-mail: dr.mahesh26@gmail.com
The aim of this case review was to touch upon the various clinical presentations and diagnostic features of Sturge-Weber syndrome (SWS) as seen in the dental/medical practice. Sturge-Weber syndrome is a rare congenital disorder that belongs to a group of disorders collectively known as the phakomatoses. The characteristic pathological elements of the disease include leptomeninges angioma extending out to cerebral cortex with angiomatous lesions on the same side and unilateral facial nevus that affects trigeminal nerve division. The classic oral lesions involve haemangiomatous gingival lesion limited on the same side of upper or lower jaw. An 18-year-old female patient reported to the Department of Oral Medicine and Radiology with oral manifestations of SWS. The evaluation of the patient, radiological findings as well as the management is discussed in this case report. It is important for the dental physician to be aware of the non-oral manifestations of SWS in order to identify and manage it appropriately. The challenge here is to see the oral manifestation as part of the syndrome and not as an isolated oral condition. Early diagnosis and appropriate treatment plan is imperative to prevent development of complications.
Gingival hyperplasia, Phakomatoses, Port-wine stain
Case Report
An 18-year-old female patient presented to the Oral Medicine and Radiology department with the primary complaint of swollen and bleeding gums in upper right maxillary region from the past one year. Patient gave a history of under-going surgery for glaucoma of right eye at the age of three months and was under medication for the same till date. She also gave a history of having seizures at young age which were transient and decreased with age.
Extra oral examination was positive for presence of Port Wine Satin (PWS) on the right side of face along the ophthalmic and maxillary divisions of trigeminal nerve, involving lips and vermilion border of lips of the same side [Table/Fig-1]. Examination of eye showed enlarged globe of right eye with bluish discoloration of bulbar conjunctiva, decreased vision and glaucoma [Table/Fig-2].
Port wine stain on the right side of face.

Enlarged right eye lobe with bluish discoloration of bulbar conjunctiva.

Intraoral examination showed hyperplasia of right side gingiva, including interdental, marginal and attached gingiva extending from anterior to posterior region. Palatal ecchymosis was also present [Table/Fig-3,4]. The clinical picture and examination pointed to SWS and further investigations were done to confirm the same.
Gingival hyperplasia on the right side.


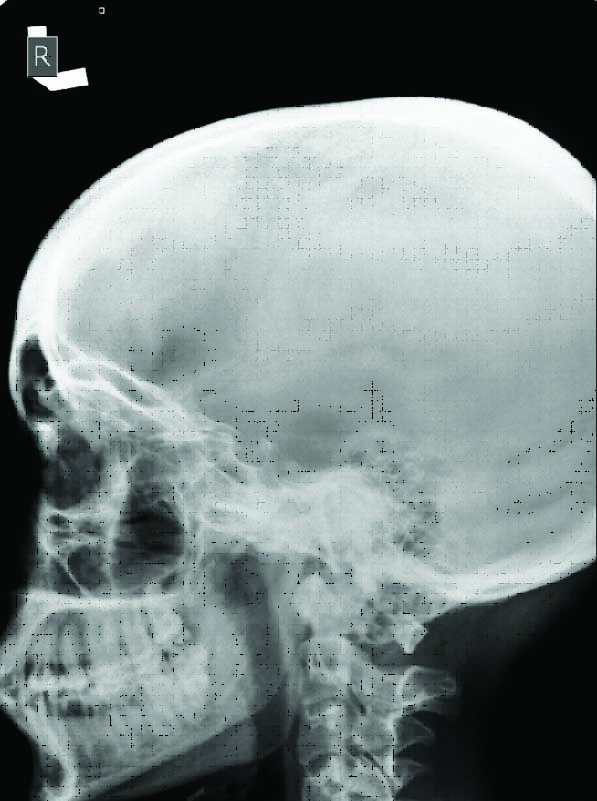
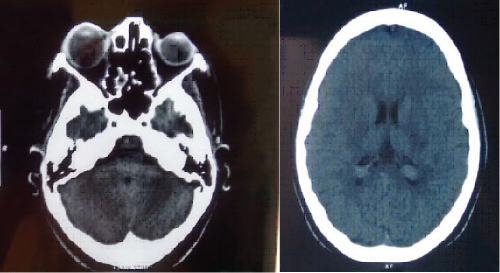
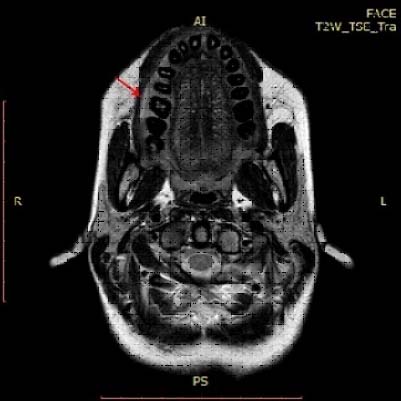
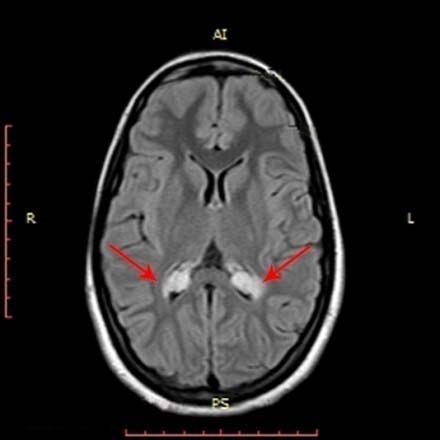
An X-ray examination of right lateral skull revealed slight eminence of the vessels with horizontal bone loss around teeth [Table/Fig-5]. An axial section of CT of brain indicated the presence of prominent right optical lobe with no significant brain parenchymal abnormality [Table/Fig-6,7], MRI of brain and maxilla showed generalized gingival hyperplasia of the right side, mild choroid plexus enlargement and buphthalmos right side [Table/Fig-8,9 and 10]. Blood investigations were normal. The radiological findings confirmed the diagnosis of SWS.
Lateral skull showing slight prominence of the vessels.
Prominent right optical lobe with no significant brain parenchymal abnormality. (Images from left to right)
MRI showing generalized gingival hyperplasia of the right side.
Bilateral mild choroid plexus enlargements.
Right buphthalamos. (Images from left to right)

Once the diagnosis was established the patient was first treated with deep scaling and curettage of right maxillary region. This resulted in a slight regression of gingival hyperplasia. A complete gingivectomy was performed with diode laser using 980 nm continuous wave motion under 5 watts current. Follow up of the patient after three weeks showed good healing with no recurrence.
Discussion
SWS is an uncommon congenital disorder. It is a type of neuro-cutaneous diseases called phakomatoses and is also referred as encephalofacial angiomatosis or cephalotrigeminal angiomatosis. It is seen in 1 in 50,000 populations. It affects both the sexes equally and does not show a racial predisposition [1-3].
It classically presents with a unilateral cutaneous nevus PWS or red wine stains on the face. The cutaneous presentation occurs due to early embryonic vascular malformation [1]. SWS may also present with angiomas in the leptomeninges resulting in epilepsy and hemiparesis and/or angiomas in the eye causing glaucoma [1,2].
The most frequent oral presentation of SWS is hyperplasia of the gingiva, affecting the maxilla, floor of the mouth, lips, cheeks, palate and tongue of the same side [2,4]. SWS may also present with changes in the histology and morphology of gingiva, periodontium, and pulp [2,4].
It’s typical manifestations include, cutaneous-port wine stain on the face, ocular-glaucoma, choroidal haemangioma and neural features- leptomeningeal haemangioma, seizures. Oral involvement in SWS presents as a gingival haemangiomatous lesion limited to the maxilla and mandible of the same side [2].
The disease gets its name from the William Allen Sturge and Frederick Parkes Weber who described it in detail. Although, it was first described by Schirmer in 1860, Sturge described the cutaneous, ocular and neural features of the disease in 1869. Weber documented the radiological changes observed in these patients in 1929 [1,2]. Various manifestations of SWS are tabulated in [Table/Fig-11] [5-13].
Manifestations of SWS [5-13].
| Cutaneous manifestations: | Nevus flammeus or PWS on the face is one of the most common presentations. It is present since birth and extends unilaterally on to the neck along the distribution of trigeminal nerve particularly the ophthalmic branch. The lesion darkens with age from reddish to purple colour [5]. The cutaneous manifestations occur more commonly on the right side and are unlikely to extend beyond the midline [2,5]. |
| Neurological manifestations : | Presence of leptomeningeal angiomatosis of the affected side is a typical feature of SWS. Abnormal pattern of blood flow leading to cerebral ischemia is also seen in SWS. The ischemia causes convulsions, hemiparesis, gliosis, mental retardation and continuous calcium salts deposition. The calcification appears as a tram-line calcification as it follows the convolutions of the cerebral cortex. The tramline calcifications are pathognomonic of SWS [2,6-8]. |
| Ocular manifestations: | Pathological changes in the conjunctiva, choroid and retina along with glaucoma are common in SWS [5]. These changes include increased conjunctival vascularization, episcleral vessel dilatation and vascular formations in the trabecular mesh-work. These structural changes led to the development of glaucoma and buphthalmos [9-11]. |
| Oral manifestations: | SWS commonly manifests as an angiomatous gingival lesion. The severity of lesion can vary from a minor vascular hyperplasia to a large angiomatous lesion. Portwine stain lesion of oral mucosa along with the hypervascular changes is also observed. Gingival haemorrhage with minor trauma is a characteristic feature of SWS. Some patients may show macroglossia and maxillary bone hypertrophy causing malocclusion and facial asymmetry [2,6,12,13]. Haemangiomatous lesion over lip, oral mucosa, tongue and palate are seen around 38% of cases [6]. Oral manifestations are unilateral and end at the midline [2]. |
Diagnosis and investigations: PWS is one of the characteristic features for clinical diagnosis [11]. PWS associated with convulsion with or without neurological loss is sufficient for diagnosis and it must be considered in conjunction with contralateral hemi paresis, glaucoma or mental retardation. Our patient presented with typical oral manifestations along with presence of nevus flammeus and history of epilepsy at a very young age which clinched the diagnosis.
Radiological investigations provide supportive evidence and aid in evaluating the extent of structural changes. CT and MRI are used to examine intracranial calcifications and cerebrovascular malformations respectively [14,15]. The skull radiographs help visualise tram-line calcification on the affected side [16].
Differential diagnosis: The other medical conditions that mimic SWS are- Klippel-Trenaunay-Weber’s syndrome, Rendu-Osler-Weber’s syndrome, Maffuci’s syndrome and Beck with-Wiedmann’s syndrome. The features of Klippel-Trenaunay-Weber’s syndrome are PWS, varicose veins, and bony and soft tissue hypertrophy affecting the extremities [6]. The Rendu-Osler-Weber’s syndrome is an autosomal dominant disorder in which vascular dysplasia affects the blood vessels throughout the body. Mucocutaneous telengiectases, arteriovensous malformations and an increased tendency to bleed are seen in these patients [10]. Maffuci’s syndrome is characterised by the presence of asymmetric enchondromas and haemangiomas, affecting the skin and skeletal system [10]. The haemangiomas present as blue subcutaneous nodules that disappear on pressure [10,15]. Beck with-Wiedmann’s syndrome shows capillary malformation in forehead and upper eyelid region which mimics PWS [16].
Treatment: The treatment of the SWS depends on the clinical manifestation. During the initial presentation medical line of management is preferred. Laser therapy for PWS, anticonvulsants for seizures, medications for controlling the intraocular pressure in glaucoma and symptomatic treatment for manifestations such as head ache. However, with time the medical management proves ineffective and surgical interventions need to be considered [3,5,16]. These include glaucoma surgery and other procedures such as lobectomy or hemispherectomy, corpus callosotomy, vagal nerve stimulation for the neurological manifestations [3,5]. Supportive measures include counselling and physiotherapy and like in all medical conditions early institution of treatment is ideal [3,5,16]. The prognosis of SWS patients is highly variable from patient to patient and was fair in most of the cases except for aesthetic appearance and presence of seizures. Life expectancy is believed to be normal.
Conclusion
In SWS the challenge for the oral physician is to be aware of its other manifestations and institute treatment and referral accordingly. The key in the management of SWS is to prevent or reduce the intensity of complications as the underlying pathology cannot be treated. Early identification and early institution of treatment is imperative for the patient to have a better quality of life.
[1]. Kowalska-Brocka J, Brocki M, Uczniak S, Uczniak K, Kaszuba A, Jurowski P, Sturge-Weber syndrome type II treated with PDL 595 nm laserAdvances in Dermatology and Allergology/Post-py Dermatologii i Alergologii 2015 32(1):63-66. [Google Scholar]
[2]. Patil K, Guledgud MV, Sahni A, Sturge Weber Syndrome- A case reportInternational Journal of Dental Sciences and Research 2015 3(3):45-47. [Google Scholar]
[3]. Siddeswari R, Manohar S, Abhilash T, Sturge Weber syndromeJ Med Allied Sci 2014 4(2):88-90. [Google Scholar]
[4]. Manjhvar SK, Gupta HO, Baghel PK, Gupta S, Jain DK, Sturge Weber syndrome with unusual intracranial findings: a case reportJournal of Evolution of Medical and Dental Sciences 2014 3(15):3863-67. [Google Scholar]
[5]. Neville Bwd DD, Allen CM, Bouquot JE, Patologia Oral e Maxilofacial. Rio de Janeiro Guanabara Koogan, 1998, 87-89 Medical record and literature reviewArch Neurol 2005 62(12):1924-27(s). [Google Scholar]
[6]. Palheta Neto FX, Vieira Junior MA, Ximenes LS, de Souza Jacob CC, Rodrigues Junior AG, Pezzin Palheta AC, Clinical features of sturge-weber syndromeIntl Arch Otorhinolaryngol. São Paulo 2008 12(4):565-70. [Google Scholar]
[7]. Roach ES, Neurocutaneous syndromesPediatr Clin North Am 1992 39(4):591-620. [Google Scholar]
[8]. Raquel IH, Psycho-educational evaluation of an adolescent with Sturge-Weber syndrome 2007 São Paulo:20-23.(Paulista State University, Bauru campus) [Google Scholar]
[9]. Mantelli F, Bruscolini A, La Cava M, Abdolrahimzadeh S, Lambiase A, Ocular manifestations of Sturge–Weber syndrome: pathogenesis, diagnosis, and managementClinical Ophthalmology (Auckland, NZ) 2016 10:871-78. [Google Scholar]
[10]. Marinho AS CK, Sturge-Weber syndromeJournal of Dentistry, University of São Paulo 2006 18:167-73. [Google Scholar]
[11]. Aydin A, Cakmakci H, Kovanlikaya A, Dirik E, Sturge-Weber syndrome without facial nevusPediatr Neurol 2000 22(5):400-02. [Google Scholar]
[12]. Santos MCM AN, Cha SB, Erwenue CM, Ultra-som ocular na síndrome de Sturge-WeberArquivo Brasileiro de Oftalmologia 1998 61:271-75. [Google Scholar]
[13]. Huang JS, Chen CC, Wu YM, Ho KY, Wang CC, Ho YP, Periodontal manifestations and treatment of Sturge-Weber syndrome—report of two casesKaohsiung J Med Sci 1997 13(2):127-35. [Google Scholar]
[14]. Gomes ACA SE, Albert DGM, Sturge-Weber syndrome: Clinical case reportJournal of Oral and Maxillofacial Surgery and Traumatology 2004 4:01-71. [Google Scholar]
[15]. Dilber C, Tasdemir HA, Dagdemir A, Incesu L, Odaci E, Sturge-Weber syndrome involved frontoparietal region without facial nevusPediatr Neurol 2002 26(5):387-90. [Google Scholar]
[16]. Caiazzo A, Mehra P, Papageorge MB, The use of preoperative percutaneous transcatheter vascular occlusive therapy in the management of Sturge-Weber syndrome: report of a caseJ Oral Maxillofac Surg 1998 56(6):775-78. [Google Scholar]