Fibrolipoma of the Oral Cavity: Treatment Choice in a Case with an Unusual Location
Roberto Pippi1, Marcello Santoro2, Romeo Patini3
1 Faculty, Department of Odontostomatological and Maxillo Facial Sciences, “Sapienza” University of Rome, Rome, Italy.
2 Faculty, Department of Odontostomatological and Maxillo Facial Sciences, “Sapienza” University of Rome, Rome, Italy.
3 Faculty, Department of Surgical Sciences for Head and Neck Diseases, Catholic University of Sacred Heart, Rome, Italy.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Marcello Santoro, Via caserta 6, 00161, Rome, Italy.
E-mail: santoro_marcello@yahoo.it
Oral fibrolipoma, Management, Surgical approach
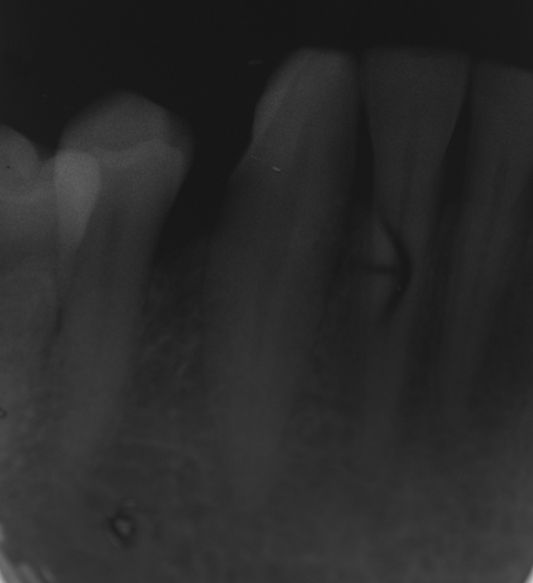
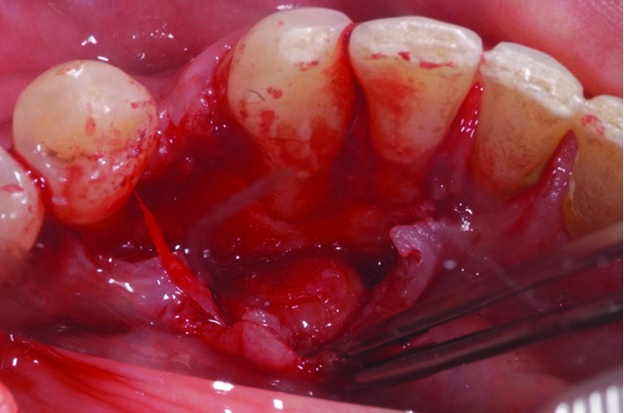
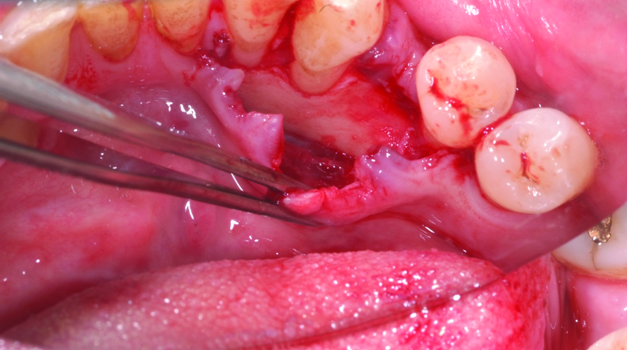
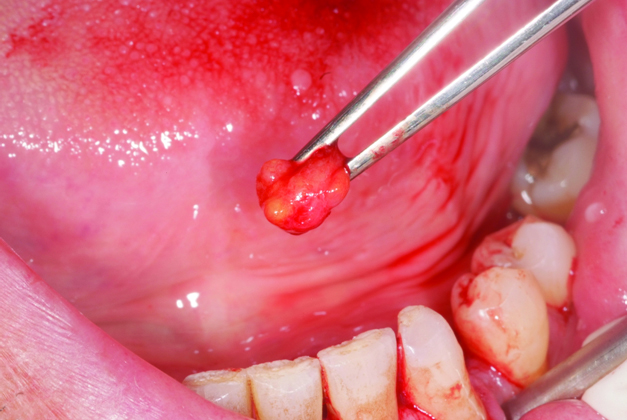
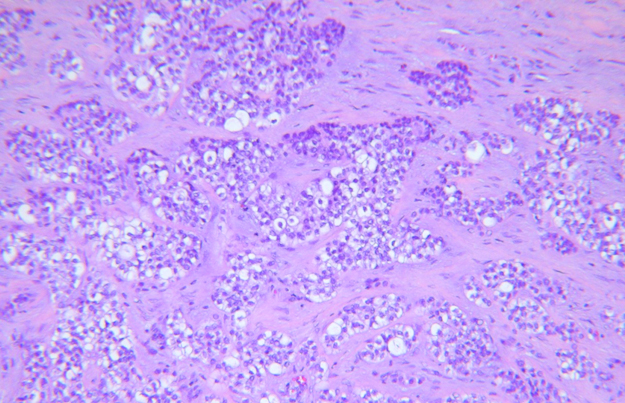
A 65-year-old male patient was admitted to the Oral Surgery Unit of Sapienza University of Rome in July 2012 due to slow but continuous swelling of the lower left canine mucosa on the lingual side, initially detected two years earlier. No difficulty in mastication, speech, or deglutition was reported. Intraoral examination confirmed the presence of a soft, painless and pseudo-fluctuant round swelling, having a greatest diameter of 0.5 cm-1 cm [Table/Fig-1]. No other swellings were found at the physical examination or in the patient’s medical history. A diastema between the left canine and first premolar was present since childhood. Routine blood test results were normal. No sign of bone involvement was found on the peri-apical radiograph [Table/Fig-2]. A provisional diagnosis of solitary intraoral lipoma was established. The lesion was enucleated under local anaesthesia. Following muco-periosteal flap elevation, a 0.8 cm wide soft tissue mass was easily isolated from the surrounding tissues [Table/Fig-3], and then removed [Table/Fig-4,5]. Finally, the flap was sutured [Table/Fig-6]. After fixation with a 10% buffered formalin solution, the pathological tissue was sent for histology [Table/Fig-7] which confirmed a definitive diagnosis of fibrolipoma. The postoperative course was uneventful [Table/Fig-8]. No recurrence of the lesion was observed after two years clinical and radiographic follow up.
Pre-operative clinical view: a pinkish, well-defined round swelling is visible apically to the muco-gingival line at the level of the lingual side of the lower left canine.

Preoperative periapical radiograph: no radiolucencies suggesting any bone involvement are evident.
Intraoperative view: an envelope flap has been elevated on the lingual side of the mandible from the ipsilateral central incisor to the first premolar; the pathological tissue mass has been easily separated by blunt dissection from both the underlying cortical bone and the overlying mucosa.
Surgical area after tumour removal. No sign of bone involvement is evident.
Surgical specimen just after the removal. Note its multi-lobed appearance and yellowish colour.
Intraoperative view: the flap has been stabilized with an interdental 3-0 silk suture.

Histology (H&E, 250X): adipose tissue with compressed blood vessels embedded within dense collagen fibers is evident. Proliferating fibroblasts are detectable in the connective tissue stroma.
Normal appearance of the healing tissues at one month.

Fibrolipomas are benign soft tissue tumours which rarely occur in the oral or maxillofacial region [1-5], and which have been reported to be more frequent in the buccal and vestibular mucosa [4], whereas the location described here is somewhat unusual. This is possibly because lipomas are thought to arise from fat cells which are not usually found, or are present only in minimal amounts in the thin soft tissue lining of this location. Moreover, the lingual side of the mandible is particularly exposed to masticatory trauma when the bolus is still hard and is compressed against the internal cortical bone of the mandible. Actually trauma has also been suggested in lipoma pathogenesis, in addition to chronic infection and hormonal imbalance [4].
Clinical alternatives to be considered in the differential diagnosis include other superficial capsulated or pseudo-capsulated lesions and tumours such as minor salivary pleomorphic adenomas, solitary neurofibromas, fibromas, granular cell tumours, leiomyomas and neurilemmomas [3,4], due to the similarity of their clinical manifestations.
No diagnostic imaging was performed in the present case as it is not usually required in small, longstanding, superficial and well-defined swelling since they are easily evaluated by clinical examination. However, computed tomography, ultrasonography and magnetic resonance imaging have been proposed in difficult cases since they were shown to obtain specific findings in lipoma diagnosis [1].
Conservative excision represents first choice surgical treatment of oral fibrolipomas. However, if clinical provisional diagnosis is highly indicative for oral lipoma due to pseudo-fluctuation, lack of pain on palpation, slow growth, a soft to fibrous consistency and yellowish appearance, the enucleation of sessile lesions may be performed [6]. This kind of treatment is carried out through an incision of the overlying mucosa and by following a cleavage plane between the lesion and the peripheral healthy tissues, unless chronic or acute traumas are reported. Actually, traumas may result in adherences, between the thin peripheral fibrous capsule of the tumour and the overlying mucosa, which may prevent such an intervention. In the current location, a third kind of approach was used with an intra-sulcular incision since it allowed best access to the pathological tissue and optimal flap repositioning. Furthermore, such a flap has a lower risk of post-surgical wound dehiscence, while the incision of the alveolar mucosa on the lingual side of the anterior mandible usually makes removal of pathological tissue and suture stability more difficult. Moreover, although lipo-sarcomas of the oral cavity are very rare and cannot be distinguished from a benign lipoma in an early stage [2,5], intraoperatively this kind of approach allowed to assure that no involvement of the bone wall was present, although this was already indicated by the mobility on palpation and the negative radiographic appearance of the lesion.
Although, recurrence after surgical removal of lipomas is rare and 5-8 months follow up has been reported in the literature [1,5], no sign of recurrence was present after two years of follow up.
[1]. Thompson LDR, Fanburg-Smith JC, Barnes L, Benign soft tissue tumours. In Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization Classification of Tumours. Pathology and geneticsHead and neck tumours 2005 LyonIARC Press [Google Scholar]
[2]. Manjunatha BS, Pateel GS, Shah V, Oral fibro-lipoma-a rare histological entity: report of 3 cases and review of literatureJ Dent (Tehran) 2010 7(4):226-31. [Google Scholar]
[3]. Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA, Lipomas of the oral cavity: clinical findings, histological classification and proliferative activity of 46 casesInt J Oral Maxillofac Surg 2003 32(1):49-53. [Google Scholar]
[4]. Kumaraswamy S, Madan N, Keerthi R, Shakti S, Lipomas of oral cavity: case reports with review of literatureJ Maxillofac Oral Surg 2009 8(4):394-97. [Google Scholar]
[5]. Manor E, Sion-Vardy N, Joshua BZ, Bodner L, Oral lipoma: analysis of 58 new cases and review of the literatureAnn Diagn Pathol 2011 15(4):257-61. [Google Scholar]
[6]. Golden DP, Hooley JR, Oral mucosal biopsy procedures. excisional and incisionalDent Clin North Am 1994 38(2):279-300. [Google Scholar]