The cytodiagnosis of serous effusions relating to distinction between malignant and highly reactive mesothelial cells has been studied extensively by light microscopy [1].
The differentiation of reactive versus malignant mesothelial cells is based on morphological features in conjunction with clinical and radiological findings. Differentiating reactive entity from malignancy needs extensive study of architectural, nuclear and cellular details. Many benign reactive processes show significant atypical features mimicking malignant changes. Likewise, a few malignant conditions lack sufficient atypical changes for a clear diagnosis of malignancy. With the advent of immunocytochemistry this problem can be largely resolved [1,2]. Several antibodies are being currently employed to cytological specimens with varying results. Cell block in conjunction with immunochemistry is being used increasingly to differentiate adenocarcinoma from reactive mesothelial cells. A combination antibody panel comprising mesothelial and epithelial markers is suggested by various studies to provide an immunohistochemical distinction between mesothelial cells and adenocarcinoma cells in serous effusions for increasing diagnostic accuracy [3].
This study was carried out in Cytology Section of Department of Pathology in tertiary care hospital in state of Uttarakhand, India, to study fluid cytology based on morphology and then use two immunomarkers namely EMA and CAL to distinguish between reactive mesothelial cells and malignant cells.
Materials and Methods
This was a prospective study carried out in Department of Pathology, Shri Guru Ram Rai Institue of Medical and Health Science for a period of 18 months from January 2014 to June 2015. A total of 253 concurrent cases of effusion cytology were studied during this period. Approval of the study was taken from the Institutional Ethics Commitee. The relevant history and the clinical findings of all these patients were recorded on a pretested performa. The fluid was used first for conventional smear preparation and stained using MGG stain and Pap stain for morphological diagnosis. The fluid samples which had malignant cells or any reactive or atypical cells on morphological diagnosis were further processed as cell blocks and Immunohistochemistry (IHC) was subsequently employed.
For IHC, sections of 2-4 micron thickness from the paraffin embedded cell blocks were made and taken on Poly-L lysine coated slides. They were subjected to immunostaining using EMA and CAL by indirect method employing rabbit polyclonal antibodies against CAL (Cell Marque dilution 1:500,) and Monoclonal mouse anti-EMA antibody (Cell Marque, dilution 1:300). A positive stain was indicated by a brown colored precipitate in the following manner:
Cells labelled with CAL displayed cytoplasmic and nuclear staining;
Cells labelled with EMA displayed cytoplasmic staining (with membranous accentuation).
The percentage of cells stained and the intensity of staining for each case was graded on semiquantative basis, serous effusions, scores of 0, 1, 2 and 3 were rendered when 0, less than 10, 10-50 and more than 50% of cells were stained and intensity score of 0, 1, 2 and 3 were given when there was none, mild, moderate and strong staining respectively. The final IHC grade of the marker was calculated by adding percentage and intensity score; and cut off more than or equal to 4 was employed for EMA and CAL staining [4].
Statistical Analysis
Statistical analysis of the data was done using the IBM-SPSS software version 20.0. Sensitivity, specificity and overall accuracy with positive and negative predictive value were calculated using Galen and Gambino method.
Results
Of 253 cases, 125 cases (49.4%) were of pleural effusion and 128 cases (50.6%) were of peritoneal effusions.
Pleural fluids: Amongst the 125 cases of pleural fluid, 88 cases (70.4%) were males and 37 cases (29.6%) were females constituting male to female ratio of 2.4:1. The median age of pleural effusion in our study was 37 years. Patients of pleural effusion presented most commonly with complaints of cough (72%), fever (64%) and dyspnoea (39%).
Of 125 cases of pleural fluid cytology, 101 cases (80.8%) were negative for malignancy and 11 cases (8%) were positive for malignancy. The remaining 13 cases exhibited either reactive mesothelial hyperplasia (10 cases, 8.0%) or were suspicious for malignancy (3 cases, 2.4%) [Table/Fig-1]. All the 11 cases that were cytologically diagnosed as malignant were confirmed to be malignant on histologial examination of cell block. Similarly, 10 cases that were of reactive mesothelial hyperplasia on cytology were also confirmed as reactive on cell block. Of three cases (12.5%) which were suspicious for malignancy, two cases (8.3%) were malignant and one case (4.1%) was reactive on histopathological examination of cell block [Table/Fig-2].
Distribution of cases of pleural fluid cytology according to cytological diagnoses.
| Parameters | Predominant Cell Population on Smear Examination | No. of cases | Percentage |
|---|
| Benign (N=101) | 1-Scanty | 14 | 11.2% |
| 2-Predominantly Neutrophil | 18 | 14.4% |
| 3-Mixed Inflammatory Cells | 16 | 12.8% |
| 4- Mainly Lymphocytes | 30 | 24% |
| 5- Mainly Mesothelial Cells | 16 | 12.8% |
| 6-Hemorrhgic Smears | 07 | 5.6% |
| Total | 101 | 80.8% |
| Malignant (N=11) | Adenocarcinoma | 10 | 8% |
| Lymphoma | 01 | 0.8% |
| Total | 11 | 8% |
| Reactive Mesothelial Hyperplasia/Suspicious For Malignancy(N=13) | Reactive Mesothelial Hyperplasia | 10 | 8% |
| Suspicious for Malignancy | 3 | 2.4% |
| Total | 13 | 10.4% |
| Grand Total (N=125) | | 125 | 100% |
Distribution of cases of pleural fluid cytology diagnosed as malignant or reactive mesothelial hyperplasia or suspicious for malignancy according to histopathological diagnosis on cell block (n=24).
| Cytological Diagnosis | Cell Block examination |
|---|
| Diagnosis | Number of Cases | Percentage | Category | Number of cases | Percentage |
|---|
| Reactive Mesothelial Cells | 10 | 41.6% | Reactive | 10 | 41.6% |
| Suspicious for Malignancy | 03 | 12.5% | Adenocarcinoma | 2 | 8.3% |
| Reactive | 1 | 4.1% |
| Adenocarcinoma | 10 | 41.6% | Adenocarcinoma | 10 | 41.6% |
| Lymphoma | 01 | 4.16% | Lymphoma | 01 | 4.1% |
| Total | 24 | | | 24 | |
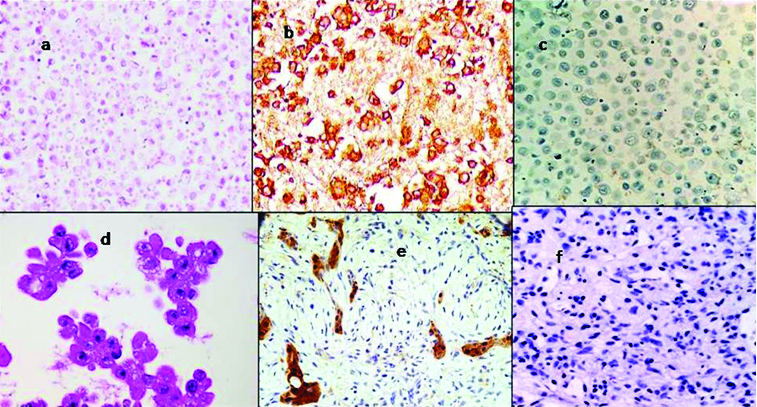
All reactive and malignant cases were subjected to immunocy-tochemical examination using EMA and CAL. Of all pleural fluid cell blocks stained employing EMA, nine cases (81.8%) of reactive mesothelial cells showed IHC grade 0. It was seen that two cases (18.1%) showed mild staining intensity in less than 10% of cells, hence were not considered as positive [Table/Fig-3]. Amongst the malignant cases (n=13), all except one case showed positivity for EMA which `was further confirmed as lymphoma on employing ancillary panel of immunostain. All 11 cases (100%) of reactive mesothelial hyperplasia were positive for CAL. Amongst malignant cases, none showed immunopositivity for CAL [Table/Fig-4].
a) Cell block prepared from a case of pleural effusion positive for malignancy; b) EMA: Malignant mesothelial cells showing strong membranous and cytoplasmic positivity; c) Calretinin: Malignant mesothelial cells displaying negative stain; d) Cell block prepared from a case of pleural effusion of reactive mesothelial hyperplasia; e) Calretinin: Corresponding block of reactive mesothelial cells displaying nuclear and cytoplasmic positivity; f) EMA: Cell block from pleural effusion of reactive mesothelial cells displaying negative stain.
Results of EMA and Calretinin immunostaining in pleural fluid cell blocks (N=24).
| Variables | EMA | Calretinin |
|---|
| Positive | Negative | Positive | Negative |
|---|
| Reactive Mesothelial Cells (N=11) | 0 | 11(100%) | 11(100%) | 0 |
| Malignant Cells (N=13) | 12(92.3%) | 1 (7.7%) | - | 13(100%) |
| 12 | 12 | 11 | 13 |
| 24 | 24 |
Peritoneal fluid: Of 128 cases of peritoneal fluid cytology, 93 cases (73.1%) were females and 35 cases (26.9%) were males. The female to male ratio was 1:2.6, and the median age was 36 years. The patients of peritoneal effusion presented commonly with abdominal pain (94%) and distension (56%).
Of the 128 cases of peritoneal fluid, 79 cases (61.7%) were negative for malignancy and 22 cases (17.1%) were positive for malignancy. The remaining 27 cases exhibited either reactive mesothelial hyperplasia (18 cases, 14.0%) or were suspicious for malignancy (9 cases, 7%) [Table/Fig-5]. All the 22 cases that were cytologically diagnosed as malignant were confirmed to be malignant on histological examination of cell block and were reported as adenocarcinoma (21 cases, 42.8%) and squamous cell carcinoma (1 case, 2.04%). Histopathological examination of nine cases that were suspicious on cytology were diagnosed as adenocarcinoma (2 cases, 4.08%) and reactive mesothelial hyperplasia (7 cases, 14.2%) [Table/Fig-6]. Thus, cell block examination was helpful in detecting two additional cases of malignancy and confirming seven cases of reactive nature.
Distribution of cases of peritoneal fluid cytology according to cytological diagnoses (n=128).
| Predominant Cell Population on Smear Examination | Number of Cases | Percentage |
|---|
| Benign (N=79) | 1-Scanty | 16 | 12.5% |
| 2-Predominantly Neutrophil | 15 | 11.7% |
| 3-Mixed Inflammatory Cells | 14 | 10.9% |
| 4-Mainly Lymphocytes | 24 | 21.8% |
| 5-Mainly Mesothelial Cells | 8 | 6.2% |
| 6-Hemorrhgic Smears | 02 | 1.5% |
| Total | 79 | 61.7% |
| Malignant (N=22) | Adenocarcinoma | 21 | 16.3% |
| Squamous Cell Carcinoma | 01 | 0.7% |
| Total | 22 | 17.1% |
| Reactive Mesothelial Hyperplasia/Suspicious for Malignancy (N= 27) | Reactive Mesothelial Hyper Plasia | 18 | 14% |
| Suspicious for Malignancy | 09 | 7.0% |
| Total | 27 | 21.0% |
Distribution of cases of peritoneal fluid cytology diagnosed as malignant or reactive mesothelial hyperplasia or suspicious for malignancy according to histopathological diagnosis on cell block (n=49).
| Cytological Diagnosis | Cell Block examination |
|---|
| Diagnosis | Number of cases | Percentage | Category | Number of cases | Percentage |
|---|
| Reactive Mesothelial Cells | 18 | 36.7% | Reactive Mesothelial Cells | 18 | 36.7% |
| Suspicious for Malignancy | 09 | 18.3% | Adenocarcinoma | 02 | 4.08% |
| Reactive Mesothelial Cells | 07 | 14.2% |
| Adenocarcinoma | 21 | 42.8% | Adenocarcinoma | 21 | 42.8% |
| Squamous Cell Carcinoma | 01 | 2.0% | Squamous Cell Carcinoma | 01 | 4.1% |
| Total | 49 | | | 49 | |
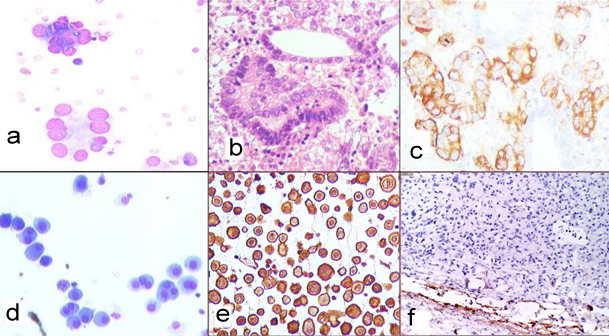
Amongst the peritoneal fluids, there were 25 cases of reactive mesothelial hyperplasia none of which (0%) showed immunoreactivity for EMA. Amongst the malignant cases, 22 cases (91.6%) out of 24 showed positivity for EMA. The two malignant cases (8.4%) that were negative for EMA were later diagnosed as hepatocellular carcinoma and squamous cell carcinoma on further employing IHC panel. Amongst the 25 cases with reactive mesothelial hyperplasia, 24 cases (96%) showed immunoreactivity for CAL. One case (4%) did not show positivity and this had mainly neutrophilic cells with very occasional mesothelial cells. Amongst the 24 malignant cases, all cases (100%) were negative for calretinin [Table/Fig-7,8].
Results of EMA and Calretinin immunostaining on peritoneal fluid cell block (n=49).
| Histopathological Diagnosis on cell Block S | EMA | calretinin |
|---|
| Positive | Negative | Positive | Negative |
|---|
| Reactive Mesothelial Cells (N=25) | - | 25 (100%) | 24 (96%) | 1 (4%) |
| Malignant Cells (N=24) | 22 (91.6%) | 2 (8.4%) | 0 | 24 (100%) |
| Total | 22 | 27 | 24 | 25 |
a) Conventional smear positive for malignancy (MGG; 40X); b) Corresponding cell block prepared displaying neoplastic glands (H&E; 40X); c) EMA: malignant cells showing membranous and cytoplasmic positivity (IHC; 10X); d) Smear showing reactive mesothelial cells (H&E;40X); e) Calretinin: Corresponding cytospin smear displaying nuclear and cytoplasmic positivity (IHC; 10X); f) EMA: Corresponding cell block of reactive mesothelial cells displaying negative stain (IHC; 10X).
Discussion
Cytological examination of pleural and peritoneal fluids is a routine procedure in most laboratories and is of paramount importance in diagnostic, therapeutic and prognostic implications [5]. Effusions are a diagnostic challenge for the cytopathologist due to difficulty in distinguishing atypical mesothelial hyperplasia, mesotheliomas and metastatic adenocarcinoma [6]. Besides, reactive mesothelial cells, abundant inflammatory cells and paucity of representative cells makes the definitive diagnosis still difficult. The overwhelming prognostic implications and therapeutic challenges involved when a patient is diagnosed with presence of malignant cells in serous cells led to the use of ancillary techniques. Amongst these immunostaining has assumed a pioneer role thus, enabling differentiation between benign mesothelial cells from malignant cells in effusions. Employing cell block method carries an additional advantage of studying multiple sections by routine staining, applying immunohistochemistry which aids in diagnosis and retrieving the cases at a later date for retrospective analysis. Various studies by different authors have suggested the use of selective commercially available antibody panel to reach a diagnosis in problematic serous effusions [7].
A total of 253 effusions were analysed by conventional smear and cell block technique; 125 cases (49.4%) were of pleural fluid and 128 cases (50.6%) were of ascitic fluid. Of 125 cases of pleural fluid cytology, the M:F ratio was 2.4:1 thus exhibiting a male preponderance and corresponding to the findings of Bhanvadia VM et al., [8]. Amongst 128 cases submitted for peritoneal fluid cytology the M:F ratio was 1:2.6 displaying peritoneal fluid cytology more commonly in females. In our study most of the effusions (54.1%) were transudative in nature while exudative effusions comprised 45.9% cases and were due to malignant effusions. Most of the effusions were seen in the age group of 41-60 years thus projecting maximum number of cases in the sixth decade which is similar to findings of Kushwaha R et al., [9]. As can be noted, malignant pleural effusions are more likely in males and are indicative of a prodrome of cancer in men which may change in future owing to an increase in number of cases of lung carcinoma in females. However, peritoneal effusions were more commonly noted amongst the females and may be attributed to high incidence of pelvic inflammatory disease in women. These findings are similar to Bhanvadia VM et al., [8].
On routine cytological examination 11 cases (46%) of pleural fluid effusion were reported positive for malignancy which on employing cell block increased to 13 cases (54.1%). An additional increase of two cases of malignancy contributing to 8.3% in the diagnostic yield was observed in our study by using cell block which is similar to findings of Bhanvadia VM et al., and Thapar M et al., who observed an additional increase of 14% and 10% respectively in diagnostic yield on employing cell block method in addition to routine cytological examination [8,10].
Similarly, for peritoneal effusions 49 cell blocks were prepared from cases submitted for pleural fluid cytology. On routine cytological examination 22 cases (44.8%) were diagnosed positive for malignancy. On further cell block examination 24 cases (48.9%) were reported as malignant thus increasing the diagnostic yield for malignancy by 5%. Thus, cell block examination was useful in confirming two additional cases of malignancy. Similarly, Udasimath S et al., studied cell block sections of pleural fluid and were able to diagnose six additional cases thus increasing diagnostic yield for malignancy by 14% [11].
Better morphological details, preservation of patterns, better nuclear and cytoplasmic preservation, and intact cell membrane were seen in cell block sections. The cell block technique offers an additional benefit of recognizing histological pattern of disease that cannot be identified in smear preparation with confidence [8]. Thus, an overall increase in the sensitivity of diagnosis by cell block method was observed in cases that were reported as suspicious for malignancy or reactive mesothelial cells by conventional smears.
In our study, EMA and CAL were employed as immunomarkers in 73 cell block sections to distinguish between reactive mesothelial cells and malignant cells. A total of 37 cases were histologically positive for malignancy (13 pleural effusion and 24 peritoneal effusions) of which 34 cases showed strong membranous and cytoplasmic positivity for EMA and all were negative for CAL. There were 36 cases diagnosed as atypical or reactive mesothelial cell hyperplasia which showed 2%-5% positivity for CAL. These cases showed nuclear and cytoplasmic positivity for CAL and none of these were positive for EMA, although five cases showed a score of 2-3, which was consider negative. Thus, in our study, EMA had a sensitivity of 91.89%, specificity of 100% and accuracy 94.8%. Murugan P et al., found that EMA showed 100% sensitivity and 97% specificity for adenocarcinoma [4]. The sensitivity, specificity and accuracy of CAL in our study were 98%, 100% and 98.9% respectively [Table/Fig-9]. Yahya ZM et al., in their study found sensitivity of mesothelial cells for CAL was 90% with 100% specificity and 96% accuracy which is very similar to our findings [12]. Likewise, other authors have reported a sensitivity of 90%-100% and specificity of 92%-98% for CAL [4,13].
Statistical analysis of EMA and Calretinin in effusion cell blocks (n=73).
| Variables | EMA | calretinin |
|---|
| Sensitivity | 91.8% | 98% |
| Specificity | 100% | 100% |
| Accuracy | 94.8% | 98.9% |
Limitation
Use of IHC markers in addition to conventional cytological smear has contributed to an increase in diagnostic accuracy. However, the plethora of antibody panel used, salient observations made and protocol suggested though gives an indication for the perfect panel yet no consensus has been made till date on the panel of antibodies to be used. It also underlies the obvious need in worldwide cytological practice to make a final diagnosis by employing objective observations in conjunction to morphological diagnosis [14].
Conclusion
In this study, it was concluded that cytological study of body fluids is a reliable, simple and cost effective diagnostic procedure with high patient acceptance and without complications. The results of fluid cytology must be assessed in conjunction with the clinical findings and other radiological and biochemical findings. Cell block method is a simple, safe, and inexpensive method which is a useful adjuvant in evaluating fluid cytology. This method yielded more cellularity with better architectural patterns and improved cytodiagnosis by 8%. Immunocytochemistry with a limited panel of EMA and CAL may help in confirming the adeoncarcinoma cells or reactive mesothelial cells. However, for typing of adenocarcinoma an additional panel of immunomarkers has to be employed.