An Extremely Rare Case of Small Cell Carcinoma in Submandibular Salivary Gland
Nigi Ross Philip1, Teerthanath Srinivas2, Ruhisalma Naagar3, Aakash4, Venkatesh Srinivas5
1 Junior Resident, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
2 Professor, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
3 Junior Resident, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
4 Junior Resident, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
5 Lecturer, Department of Oral and Maxillofacial Surgery, A.B. Shetty Memorial Institute of Dental Sciences, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Teerthanath Srinivas, Professor, Department of Pathology, K.S.Hegde Medical Academy, Mangalore, Karnataka, India.
E-mail: steerthanath@yahoo.com
Small Cell Carcinoma (SCC) of the salivary gland is a rare and aggressive tumour accounting for about less than 1% of the salivary gland tumours. Submandibular gland involvement is extremely rare. These tumours frequently present with metastasis to lymph node and distant organs. We report a case of a 30-year-old male patient who presented with a swelling on the left side of the face below the jaw and the floor of the mouth. The tumour was excised followed by histopathological evaluation and diagnosed as SCC of left submandibular gland. Immunohistochemistry was positive for pan cytokeratin, synaptophysin, chromogranin, Ki-67, CK5/6, and negative for Thyroid Transcription Factor (TTF-1) which confirmed that the tumour was SCC of submandibular salivary gland.
Chromogranin, Pan cytokeratin, Synaptophysin
Case Report
A 30-year-old man presented with a swelling below the left side of the jaw extending to the floor of the mouth since two months. He also gave a history of difficulty in speaking as the swelling interfered with the movement of the tongue. He reported loss of weight over one month. He had no other significant past history and did not smoke or drink alcohol. On examination, there was a diffuse swelling in the left jaw extending to the floor of the mouth in the left side which was about 3 cm from the tip of the tongue. It was firm in consistency with an irregular edge and smooth surface. The skin over the swelling was adherent to the underlying mass. The clinical diagnosis of malignant tumour of the left submandibular gland was made. No lymph nodes were palpable at the time of presentation and the clinical stage was T3N0M0.
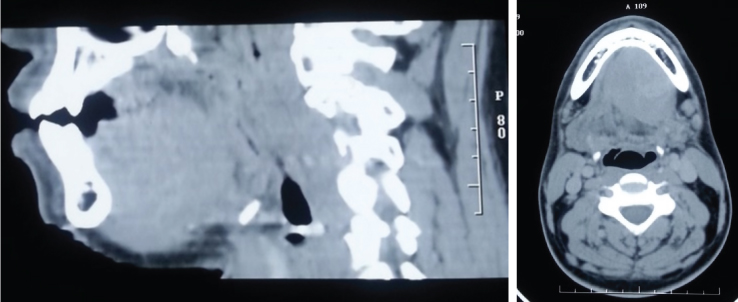
An ultrasound of the neck was done which suggested a diagnosis of left submandibular neoplasm. CT scan of the head and neck revealed submandibular gland tumour [Table/Fig-1a,b]. Fine Needle Aspiration Cytology (FNAC) of the left submandibular salivary gland was done and it was suggestive of poorly differentiated malignant neoplasm of the left submandibular salivary gland. The tumour cells were in irregular clusters showing moderate cellular and nuclear pleomorphism with focal nuclear moulding and moderate amount of cytoplasm. Chest X-ray, endoscopy and whole body scan were done to exclude pulmonary lesions and distant metastasis. Patient underwent surgical resection and specimen was sent for histopathological evaluation.
CT image of lateral view and axial view showing irregular rarefaction of the left submandibular neoplasm.
Grossly, an irregular grey brown tissue mass measuring 7.5 x 5.5 x 3.5 cm was received. The outer surface had attached normal salivary gland with skin on one side of the mass along with muscle and two lymph nodes. The cut surface showed an irregular homogenous grey white lesion with areas of necrosis [Table/Fig-2].
Gross: cut surface of the tumour showing an irregular homogenous grey white mass with adjoining normal looking salivary gland and skin on one pole.

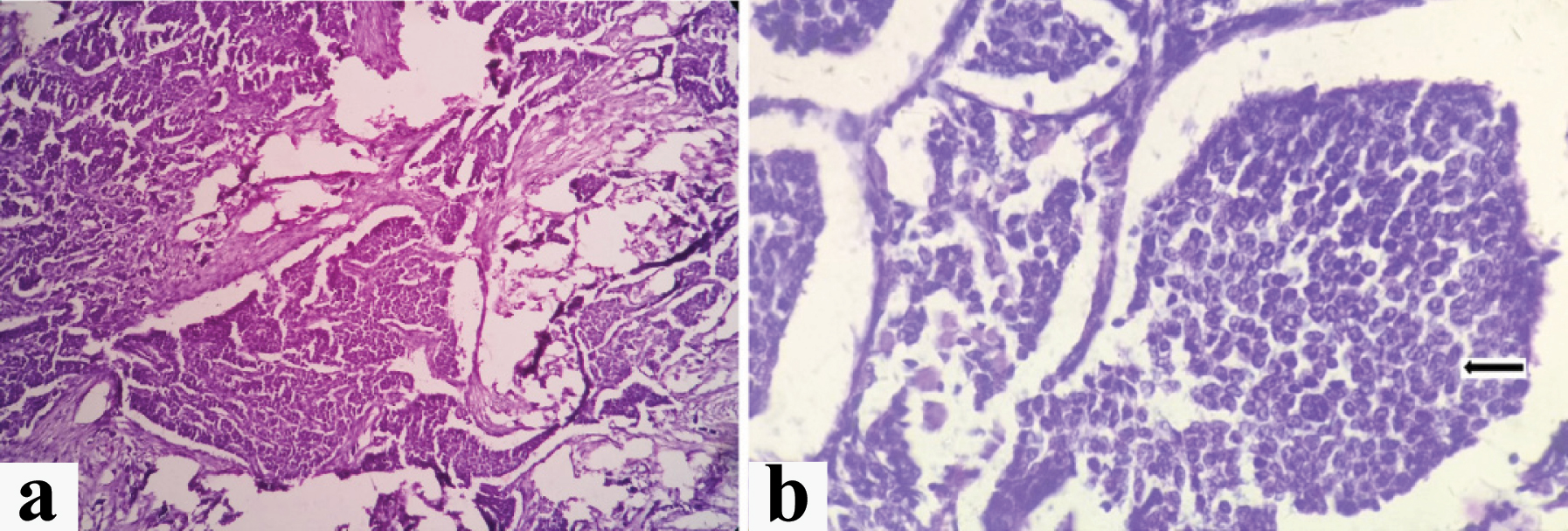
Microscopically, the submandibular salivary gland showed the presence of infiltrating tumour. Tumour cells were small round with round to oval nuclei and scanty cytoplasm in the fibrovascular stroma. The cell border was ill defined with nuclear moulding. There was also focal area of perineural invasion. Tumour cells were seen penetrating the submandibular salivary gland and extending into the dermis, not invading epidermis. There was no evidence of tumour infiltrating the adjoining skeletal muscle and isolated lymph nodes [Table/Fig-3a,b]. The histopathological diagnosis of SCC of left submandibular gland was given. The tumour was in clinical stage of TNM stage III (T3N0M0).
(a) Small round tumour cells arranged in sheets separated by fibrous stroma. (H&E, X100); (b) Small round tumour cells showing nuclear moulding (arrow) (H&E, X400).
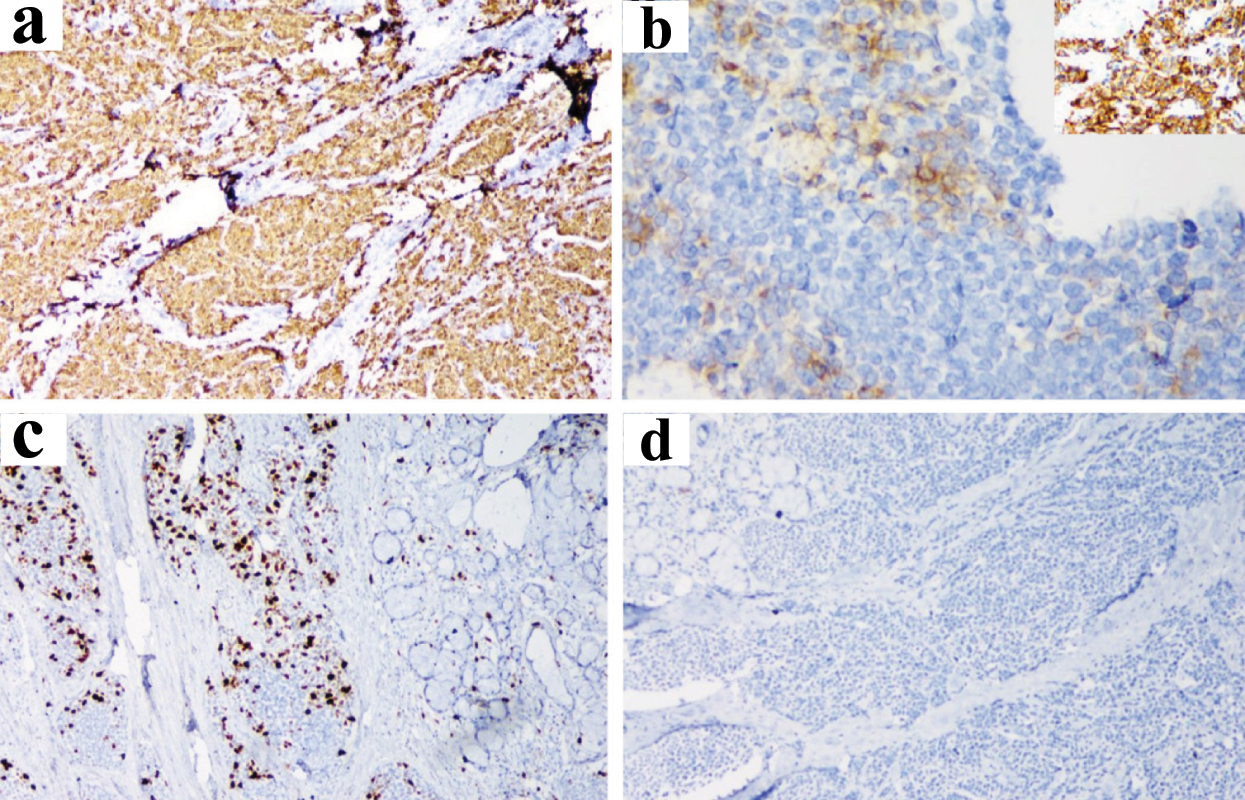
Immunohistochemical study showed positivity for pan cytokeratin, synaptophysin, chromogranin, CK5/6, Ki-67 (20%) and negative for TTF-1 which confirmed the diagnosis of SCC of the left submandibular salivary gland [Table/Fig-4a-d].
(a) Tumour cells show pan cytokeratin positivity (x100); (b) Chromogranin positivity (x400), Inset: Synaptophysin positivity (x400); (c) Tumour cells showing Ki-67-20% (x100); (d) Tumour cells were TTF-1 negative (x100).
Further management included radiotherapy and adjuvant chemotherapy with six cycles of cisplatin (40 mg/body mass index) and paclitaxel (80 mg/body mass index). The patient was followed up after six months and with no recurrence of the tumour.
Discussion
SCC was initially identified in the lung as oat cell carcinoma. In 1972 Olofsson and Van Nostr reported the first case of SCC of the head and neck which was found to be in the larynx [1]. SCC of the salivary glands accounts for less than 1% of the tumours [2]. Only eight cases have been reported till date and we report the ninth case of SCC of the submandibular gland [2]. The median age of presentation is 64.7 years, with a peak incidence in the eighth decade of life. Our patient was only 30 years old which is rare age for presentation of the SCC of submandibular gland. Patients usually present with an asymptomatic swelling. The other uncommon symptoms include pain, paraesthesia, paraneoplastic syndrome and facial nerve paralysis. SCCs have an aggressive behaviour associated with a higher metastatic potential and poor survival, with most patients dying before three years of follow up. The incidence of cervical lymph node involvement is over 50% and that of distant metastases is less than 45% [2]. In our case, there was neither evidence of lymph node or distant metastasis nor involvement of other salivary glands.
Microscopically, the tumour cells in SCC are 2-3 times larger than the mature small lymphocytes and are round or oval in shape, arranged in solid sheets and nest of tumour cells. Majority of the tumour cells in SCC express at least one of the neuroendocrine markers. It has been reported that membrane-bound, dense-core neurosecretory granules were observed in approximately 20% of cases of SCCs of the salivary glands [1]. The expression of pan cytokeratin, synaptophysin, chromogranin suggests a neuroendocrine SCC [1]. Chromogranin is an acidic glycoprotein that is associated with neurosecretory granules which is specific for neuroendocrine differentiation. Synaptophysin is found in the presynaptic nerve cell vesicles. Perinuclear cytokeratin and pankeratin stain positivity are consistent with SCC. A negative TTF-1stain indicates a salivary gland tumour since most of the lung SCCs show positivity for TTF-1 stains [3].
The differential diagnosis for SCC of submandibular gland should include solid-type adenoid cystic carcinoma, malignant lymphoma, ewing’s sarcoma, malignant melanoma, metastatic Merkel cell carcinoma and pulmonary (oat cell) SCC [2]. A negative stain for CD45 rules out lymphoma. Ewing’s sarcoma stains positive for CD99. HMB-45 is used to identify malignant melanoma.
Surgery and adjunctive radiation therapy are the main stay of treatment, with chemotherapy in selected cases. Due to the rarity of these tumours, there are no definitive treatment recommendations [3]. Some authors proposed radiation therapy alone with or without chemotherapy as an alternative to surgery. Overall, SCC of the salivary glands was found to have a better prognosis as compared to the SCCs in other areas. The most favourable one and five year survival rates are 71% and 40%, respectively [4]. The local recurrence occurs in 75% of those patients who have been treated by surgery only, while the recurrence rate is reduced to 20% with the combination of surgery and radiotherapy [5]. There was no evidence of recurrence in the present case during the follow up period.
Conclusion
SCCs of submandibular salivary gland are extremely rare. However, with appropriate early diagnosis and aggressive treatment, these tumours can be completely cured. Immunohistochemical stains are used for the confirmation and characterization of the tumour. Although these tumours are rare, SCC should be included in the differential diagnosis of salivary gland masses. Further studies are needed for the definitive management of SCCs of submandibular salivary gland.
[1]. Liu M, Zhong M, Sun C, Primary neuroendocrine small cell carcinoma of the parotid gland: A case report and review of the literatureOncology Letters 2014 8(3):1275-78. [Google Scholar]
[2]. Servato JP, Da Silva SJ, De Faria PR, Cardoso SV, Loyola AM, Small cell carcinoma of the salivary gland: A systematic literature review and two case reportsIntJ Oral Maxillofac Surg 2013 42(1):89-98. [Google Scholar]
[3]. Walters DM, Little SC, Hessler RB, Gourin CG, Small cell carcinoma of the submandibular gland: a rare small round blue cell tumorAmerican Journal of Otolaryngology-Head and Neck Medicine and Surgery 2007 28(2):118-21. [Google Scholar]
[4]. Lin Y-C, Wu H-P, Tzeng J-E, Small-cell undifferentiated carcinoma of the submandibular gland: an extremely rare extrapulmonary siteAmerican Journal of Otolaryngology-Head and Neck medicine and Surgery 2005 26(1):60-63. [Google Scholar]
[5]. Kanazawa Parotid small cell carcinoma presenting with long-term survival after surgery alone: a case reportJournal of Medical Case Reports 2012 6:431 [Google Scholar]