Saliva plays a key role in the maintenance of oral health. Functions attributed by its fluid characteristics are cleansing of the oral cavity, food bolus formation, facilitation of mastication and swallowing, food and bacterial clearance, lubrication of mucosa and facilitation of speech [1]. In patients older than 60 years it is estimated that more than 30% suffer from dry mouth where as the overall prevalence is between 7 to 29% [2,3]. Xerostomia is defined as dryness of mouth from the lack of normal secretions [3]. People affected with xerostomia complain about the dryness of mouth, problems with eating, speaking, swallowing all of which affect their nutritional status and psychological health. Xerostomia patients often complain of difficulty in wearing dentures and sore mucosa due to diminished lubricating property of saliva [4-6]. The functional deficits caused by xerostomia often progress to psychological impact leading to avoidance of social contact and events, frustration, embarrassment, apnoea all together further reduce the overall quality of life [7,8].
Xerostomia is not generally considered as a disease despite its high prevalence in the elderly; therefore, this condition continues to show its impact on oral health related quality of life [9,10]. Since xerostomia is a subjective feeling of oral dryness, traditional methods like measuring salivary flow rate may not really depict degree of oral dryness to bridge this gap, Osailan SM et al., developed new index known as Clinical Oral Dryness Score (CODS) with acceptable validity and reproducibility in assessment of severity of oral dryness clinically [11].
There is an increased importance of dental care for geriatric populations in all Western and developing countries like India [12]. The prosthetic need for elderly population ranges from 52%-70% [13]. Various factors influence patients’ satisfaction with complete denture prosthesis. Anatomical factors are a key component of denture stability and retention [14]. But denture retention depends on complex relationships between adhesion, cohesion, atmospheric pressure, surface tension, and viscosity. Thin layer of saliva between denture base and oral mucosa highly affects denture retention [15]. Apart from poor retention and stability of dentures, oral dryness may also influence the patient’s satisfaction with complete dentures. Hence, the aim of the study was to assess the relation between oral dryness score and denture satisfaction among elderly patients. The research hypothesis tested was that “there is no relation between clinical oral dryness score and denture satisfaction among elderly complete denture wearers”.
Materials and Methods
In the present cross-sectional study, completely edentulous patients who got complete dentures done at prosthodontic department of the Drs. Sudha and Nageswara Rao Siddhartha Institute of Dental Sciences, Gannavaram, India, during January 2015 to May 2015 were invited to participate in this study. An invitation letter was sent to all eligible patients who met inclusion criteria of the study and those patients who agreed to participate were included in this study. Study protocol was approved by Institutional Review board (reference number: OR-2015/108).
Inclusion Criteria
Edentulous subjects, wearing complete dentures for at least six months and who gave written and voluntary consent to participate in this study.
Exclusion Criteria
Patients having any complications like broken dentures, poor retention and stability, over/under extended borders, centric/vertical relation problems, irregular in using dentures, etc., and medically compromised/who were under any medication which affects salivary flow rate.
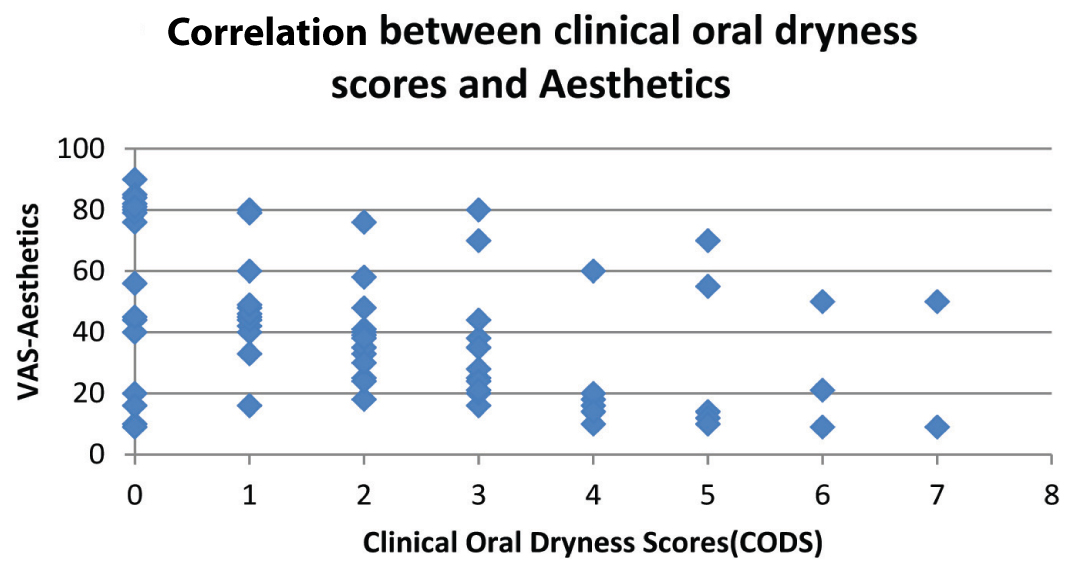
After obtaining informed consent, patients were examined to assess status of prosthesis and denture related lesions. Sample size was calculated from Mean±SD oral dryness scores obtained from pilot study conducted on ten patients which has standard deviation of 0.25. Sample size was calculated using the formula:
Hence, total sample of 200 was required to detect clinically significant difference of 10% with 95% CI and 80% and sample size was increased to 220 forecasting 10% errors, loss of data, etc. Finally, 220 participants out of 423 responders were included in this study.
Prosthetic Status Assessment
The patients and dentures were examined by three qualified prosthodontists who were blinded to the study protocol. Patients with following prosthetic complications were excluded from the study like ulceration, denture stomatitis, inflammatory papillary hyperplasia, epulis fissuratum, loss of retention, denture base fracture, loss or fracture of artificial teeth, inappropriate vertical dimension, poor centric relations and poor denture hygiene [15].
Recording of Clinical Oral Dryness Score (CODS)
As described by the Osailan SM et al., the CODS used in the present study consisted of a 10-point scale, each point representing a feature of dryness in the mouth [Table/Fig-1] [11].
Clinical oral dryness scoring criteria by Osailan SM et al., [11].
| Score | Criteria |
|---|
| 1 | Mirror sticks to buccal mucosa. |
| 2 | Mirror sticks to tongue. |
| 3 | Frothy saliva. |
| 4 | No saliva pooling in floor of mouth. |
| 5 | Tongue shows loss of papillae. |
| 6 | Altered/smooth gingival architecture. |
| 7 | Glassy appearance of other oral mucosa, especially palate. |
| 8 | Tongue lobulated/fissured. |
| 9 | Active or recently restored (last 6 months) cervical caries (2 teeth). |
| 10 | Debris on palate (excluding under dentures). |
Although the scoring system reflects an approximate severity scale, each feature scores one point and the total is determined. A high total score indicates increased severity of oral dryness and individual score ranges from 0-10.
Denture Satisfaction Assessment
Each patient used a VAS to express satisfaction with aesthetics, chewing ability and phonetics with the prosthesis [15]. Considering each aspect, patients were asked to score on a 100-point scale with scores ranging from 0-100. For example, patient were asked three questions like how you rate your satisfaction on your chewing ability with your present dentures on a 100-point scale, score zero for dissatisfaction and score hundred for complete satisfaction and similar questions on aesthetics and phonetics [15].
Statistical Analysis
Data was analysed with Statistical Software for Social Sciences, (SPSS) version 20.0 (Chicago.inc). Kendall’s tau-b correlation was used to determine the relationship between mean denture satisfactions and mean clinical oral dryness scores. The results were assessed at the 95% confidence interval at a significance level of p<0.05.
Results
Out of the 220 study participants, 42 were between 45-55 years age group, 96 of them were 56-65 years and 82 of the were above 65 years. A total of 126 of 220 were males and 94 of them were females [Table/Fig-2].
Demographic characteristics of the participants.
| Characteristic | Participants (%) |
|---|
| Age (yrs)45-5556-65>65Total | 42 (19%)96 (43.6%)82 (37.4%)220 (100%) |
| GenderMaleFemale | 126 (57.2%)94 (42.7%) |
Among the VAS-scores for denture satisfaction, the mean score for aesthetics was 74.32±21.20, for chewing ability the mean score was 62.31±19.64 and for phonetics it was 67.82±30.60 [Table/Fig-3].
Participants denture satisfaction scores.
| Patient satisfaction (VAS) | Range | Mean ±SD | Median |
|---|
| Aesthetics | 0-100 | 74.32 ± 21.20 | 78 |
| Chewing ability | 0-100 | 62.31 ± 19.64 | 56 |
| Phonetics | 0-100 | 67.82 ±30.60 | 60 |
When clinical dryness scores were recorded, nearly one-fourth of the participants has no signs of dryness, 26% of them had dryness score one, 21% had score two, 16% of them had score three and so on. Overall mean and median dryness score of the participants were 1.8±0.6 and 2 respectively [Table/Fig-4].
Frequency distribution of clinical oral dryness scores overall mean CODS score= 1.8±0.6 and Median=2.
| Score | Frequency | Percentage |
|---|
| 0 | 53 | 24.1 |
| 1.00 | 57 | 25.9 |
| 2.00 | 46 | 20.9 |
| 3.00 | 35 | 15.9 |
| 4.00 | 17 | 7.7 |
| 5.00 | 7 | 3.2 |
| 6.00 | 3 | 1.4 |
| 7.00 | 2 | 0.9 |
| Total | 220 | 100 |
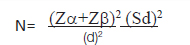
When clinical oral dryness score was correlated with various aspects denture satisfaction, there was strong negative correlation between the Clinical Oral dryness scores and Patients satisfaction (VAS scores) for chewing ability which was statistically significant (τb = -0.634, p= 0.001) [Table/Fig-5] and similarly typical negative correlation was identified between CODS scores and patients satisfaction with Phonetics (τb = -0.512, p= 0.001) [Table/Fig-6]. There is no statistically significant correlation between patient satisfaction (VAS) scores for Aesthetics and Clinical Oral dryness scores {τb = -0.220, p= 0.711} [Table/Fig-7].
Correlation between clinical oral dryness scores and VAS scores of chewing ability using Kendall’s tau-b test. Correlation coefficient τb = -0.634, p= 0.001.
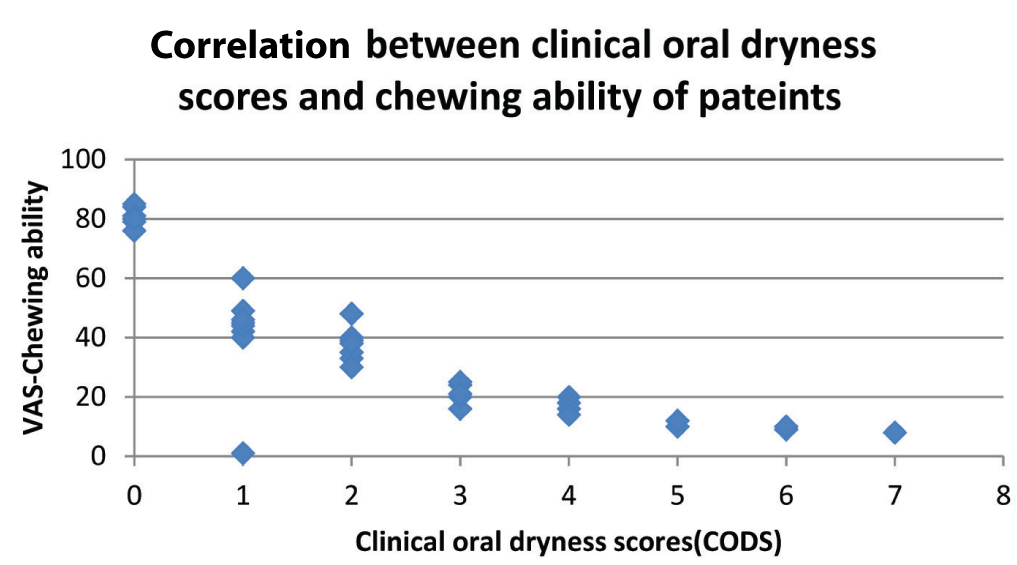
Correlation between clinical oral dryness scores and VAS scores of phonetics using Kendall’s tau-b test. Correlation coefficient τb = -0.512, p= 0.001.
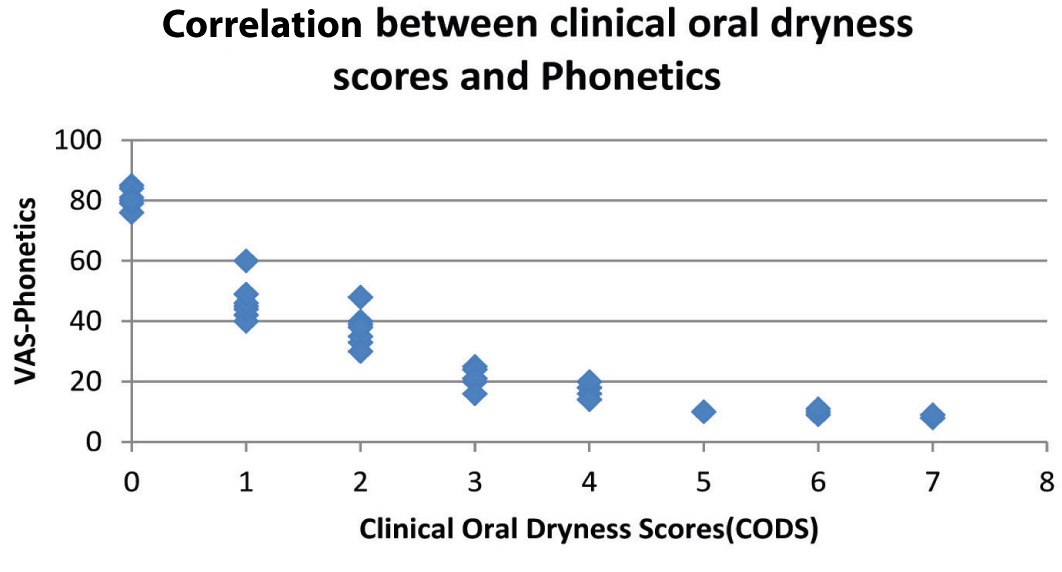
Correlation between CODS and VAS Scores of aesthetics using Kendall’s tau-b test. Correlation coefficient τb = -0.220, p= 0.711.
Discussion
Edentulism and xerostomia are two most common problems in elderly population. These two problems influence the oral health related quality of life which in turn may have an impact on general health of these populations [16]. In India, mode of rehabilitation for edentulism in majority of the patients is complete denture [17].
Saliva plays an important role in the retention of complete denture which is a major factor in success of complete denture and retention also plays an important role in patient satisfaction and comfort in using prosthesis. The study participants who were involved in this study were the patients who were using complete dentures for at least six months; this was done to avoid problems of new denture confounding with study outcome. Out of the 423 respondents who agreed to participate in this study, nearly half of them were excluded after examination by prosthodontists. The common problems for exclusion were poor retention, ulcers and patients not using dentures regularly which may decrease denture satisfaction. Traditionally, decreased salivary rate has been measured in terms of Unstimulated Salivary Flow Rate (USSR) and stimulated Salivary Flow Rate (SSR), since xerostomia is a subjective feeling of a patient, relatively new index has been used to measure the degree of xerostimia closely to subjective feeling of a patient, known as CODS proposed by Osailan SM et al., which has good reproducibility of 0.89-0.96 [11].
The major findings of this study were comparable to only one study where this index was used [11]. The mean CODS score (1.8±0.6) of present study were similar to CODS scores of control group (otherwise healthy) of Osailan SM et al., study in which mean score was 1±0.9 [11].
In the present study, VAS-scale has been used to elicit the patient’s denture satisfaction, the mean VAS- score for aesthetics, chewing ability and phonetics were similar to study conducted by Bilhan H et al., in Turkey in which the mean VAS-score for aesthetics was 64.27±31, for chewing ability 57.73±32 and 77.27±29.04 for phonetics [15]. The results of the present study can be compared to study reported by Gosavi SS et al., from India, in which 35% of the patients were dissatisfied with their dentures due to poor retention [18].
In the present study, there was a strong negative correlation between the clinical oral dryness scores and VAS scores for patients chewing ability and phonetics, no significant correlation between VAS scores for aesthetics and oral dryness scores, which can be explained by the fact that chewing and phonetics represent the functional aspect of the complete denture which can be impaired by oral dryness.
This study has some limitations especially relating to the lack of representativeness of the sample. Patients were recruited from a dental institution during a short period. Patients who attend this type of clinical setup were usually from lower social economic class and their perceptions may be different from patients who are attending private clinics. Therefore, generalization of this study should be made with caution. However, each approach has its own strengths and weakness, this study made an attempt to correlate a new index to measure severity of xerostomia clinically i.e., CODS with complete denture satisfaction and the findings suggest that CODS negatively influence denture satisfaction.
The present study did not evaluate retention and stability of the prosthesis worn by the study subjects objectively. Measurement of the retention and stability using specific scales and standardisation on patient selection based on these scores would have resulted in more specific results. Further studies can be conducted incorporating these objective scales.
Conclusion
Increased CODS is one of the factors which adversely affect patient’s denture satisfactions. Dentists should consider this in predicting prognosis.