Diagnostic Dilemma in a 15-Year-Old Boy with Recurrent Pneumococcal Meningitis
Aniruddha Ghosh1, Saurav Sharma2, Partha Pratim Halder3, Arunaloke Bhattacharya4, Swapan Mukherjee5
1 Junior Resident, Department of Paediatric Medicine, Institute of Child Health, Kolkata, West Bengal, India.
2 Junior Resident, Department of Paediatric Medicine, Institute of Child Health, Kolkata, West Bengal, India.
3 Assistant Professor, Department of Paediatric Medicine, Institute of Child Health, Kolkata, West Bengal, India.
4 Associate Professor, Department of Paediatric Medicine, Institute of Child Health, Kolkata, West Bengal, India.
5 Professor, Department of Paediatric Neurology, Institute of Child Health, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aniruddha Ghosh, Institute of Child Health, Kolkata Male PGT Quarters, Room No-7 MRI Building 3rd floor-11, Dr. Biresh Guha Street, Kolkata-700017, West Bengal, India.
E-mail: aniruddha179@gmail.com
Recurrent bacterial meningitis is very rare phenomenon in paediatric age group. Finding the aetiology of recurrent meningitis often poses diagnostic challenge to clinicians. Among the several aetiologies, structural deficiencies at the base of skull, congenital or acquired, are readily correctable ones and hence it’s imperative to find out the location of the gap in order to surgically repair it. We report the diagnostic dilemma faced while managing a 15-year-old boy with recurrent pneumococcal meningitis. Aetiology could only be found after exclusion of immunodeficiency and performing a series of imaging studies. CT cisternogram clinched the diagnosis and patient was cured successfully. A single imaging modality, be it CT/MRI scan, although proven to be better than others according to literature, might not be sufficient while finding the cause of recurrent bacterial meningitis in an immunocompetent host.
CT cisternogram, Pneumococcus, Recurrent meningitis
Case Report
A 15-year-old boy with history of two episodes of acute bacterial meningitis in the past, (first episode at nine years and second at 10 year and two months of age) presented with history of high grade fever for last two days associated with headache, nuchal pain and recurrent vomiting. There was no history of seizure or altered sensorium.
Patient was normal between and after the previous attacks. There was no history of trauma, otorrhea, rhinorrhoea or any history suggestive of chronic infection of parameningeal structures/spaces. Also there was no history of recurrent infections involving any other system, blood transfusion or family history of any immunodeficiency disorder.
During the 1st episode, Cerebospinal Fluid (CSF) culture was negative and MRI scan of brain revealed an insignificant small retrocerebellar cyst.
During the next episode, CSF culture showed growth of pneumococci. High Resolution Computed Tomography (HRCT) of skull was within normal limits. An audiological assessment was done which revealed no hearing impairment. Serum complement levels, i.e., C3 and C4 were also found to be normal.
Both the times, patient received intravenous ceftriaxone for 14 days and responded well to treatment. After the 2nd episode, he also received vaccination against pneumococci, meningococci and H. Influenzae.
This time, the third attack of the series, definite neck rigidity, Kernig’s and Brudzinski’s signs could be elicited. There was no focal neurological deficit and examination of the cranial nerves including the fundi was normal. Other systemic examinations didn’t reveal any abnormality.
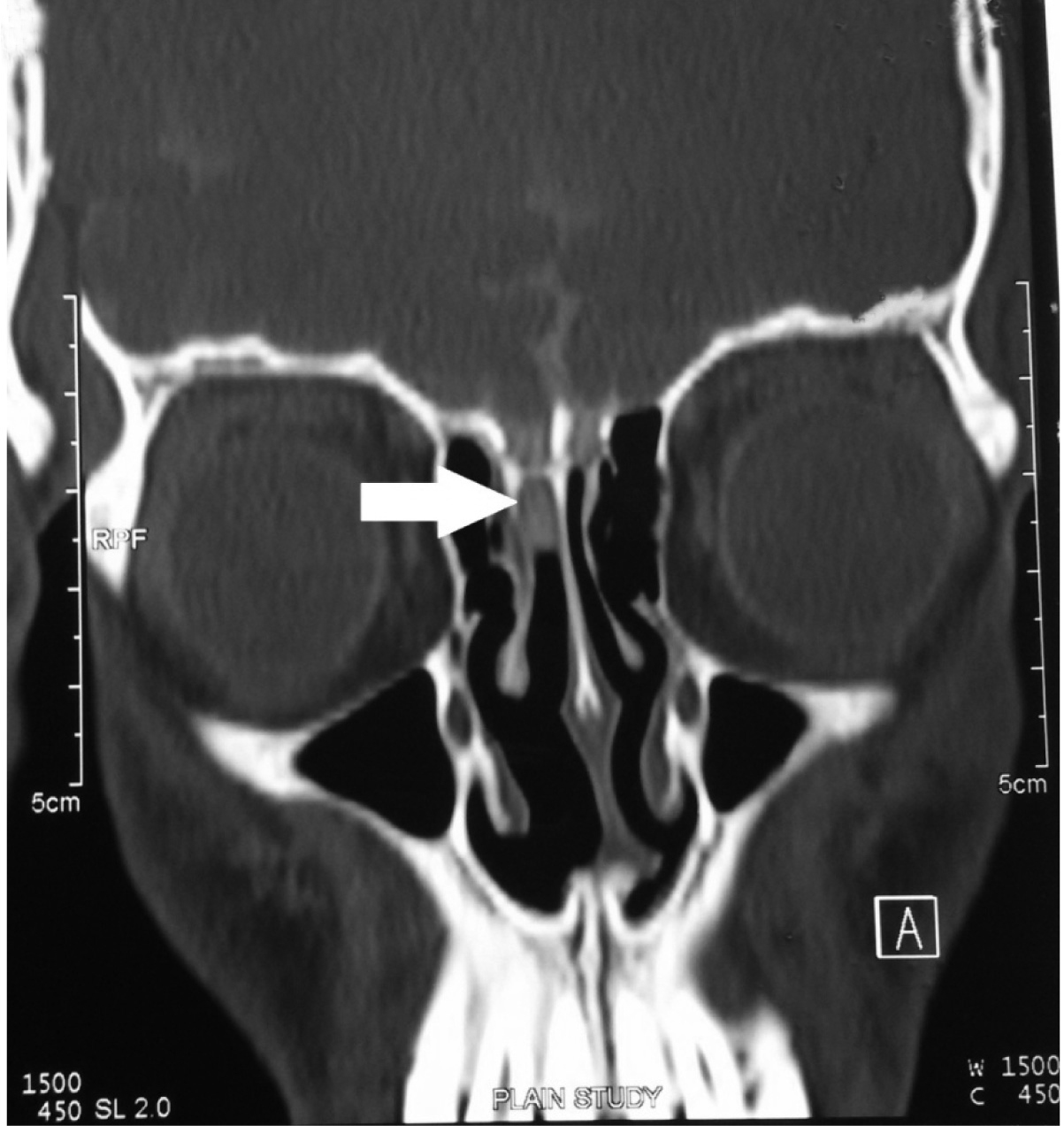
CSF analysis showed a cell count of 38,400/cmm with 70% neutrophilic preponderance; Glucose 1 mg/dL, protein 20 mg/dL. Culture revealed growth of pneumococci and patient was successfully treated with course of intravenous ceftriaxone for 14 days. All the previous reports, specially the radiological images were reviewed but no cause of recurrence was found. Immunoglobulin levels, HIV serology, CD4 and CD8 counts, assessment of total serum haemolytic complement (CH 50) – all were within normal limits. Finally a CT Cisternogram was done which clinched the diagnosis. It revealed a focal bony defect at the right cribriform plate with thin streak of contrast leaking from it and extending into nasal cavity [Table/Fig-1].
CT cisternogram showing focal bony defect at the region of right cribriform plate with thin streak of contrast leaking from here (marked by white arrow) into the nasal cavity.
A planned surgical repair of the defect was done through intranasal approach and patient was on regular follow up for last 5 months and is stable.
Discussion
Bacterial meningitis is a potentially life threatening infection in paediatric population. In spite of advancements in antimicrobial therapy and paediatric intensive care support, mortality and long term neurological sequelae are still a cause of concern even in very good tertiary care centers. Luckily, recurrence of bacterial meningitis is rare and occurs in around 1% of all pyogenic meningitis cases [1].
Recurrent bacterial meningitis is defined as two or more episodes of pyogenic meningitis separated by a period of convalescence and the complete resolution of all signs, symptoms and laboratory findings [2,3]. Drummond DS et al., observed that out of all the children admitted to a tertiary care hospital with bacterial meningitis over a period of 11 years, only 1.3% suffered from recurrence [4].
Congenital abnormalities (anatomical defects of skull bone exposing the meninges to extra-calvarial environment, immunodeficiency disorders etc.) as well as several acquired conditions (skull bone fractures, human immunodeficiency virus infection, chronic parameningeal infections etc.,) predispose a patient to recurrent bacterial meningitis, the most common risk factor being anatomical defects of the cranial bones [2,3].
Bony dehiscence involving anterior skull base, middle ear cavity and adjoining mastoid areas, persistent sinus tracts communicating vertebral column with superficial surface of dermis and rarely neurenteric cysts and fistulas are reported among congenital defects giving rise to recurrent meningitis during childhood or adolescence [5]. Apart from neurosurgery and parameningeal chronic infections, trauma resulting in fracture of cribriform plate of ethmoid bone is the commonest acquired cause of recurrent meningitis [6]. Kline MW et al in their review marked congenital skull base defects as the most predominant cause in paediatric population [7].
In a case series reported by Lieb G et al., out of 25 patients, only two with skull fracture had definite history of head injury but similar history was also noted by the authors to be present in patients with congenital bony defects also [8]. So history regarding any major traumatic event which occurred even years before the first episode of meningitis should not be missed. Equally, a history of otorrohea and rhinorrhea should also be taken as many a times persistent nasal discharge has reportedly been neglected by the caregivers for years after a head trauma as they could not realise it to be associated with the disease [9].
According to almost all review articles on recurrent bacterial meningitis, streptococcus pneumoniae was found to be the most common infectious agent and neisseria meningitidis was the second most common organism though it was more common in immunodeficient hosts [2].
In their review, Tebruegge M et al., recommended a full blood count with a differential and microscopy to detect Howell-Jolly bodies (which may suggest asplenia) as well as lymphopenia or neutropenia [2]. Abnormalities in immunoglobulin levels may point towards immunodeficiency disorders like selective IgA deficiency, common variable immunodeficiency, IgG subclass deficiency etc. Assessment of the total serum haemolytic complement (CH50) will detect abnormalities of the classical complement pathway (C1 to C9) and should be followed with assays for individual complement components if found to be abnormal. An HIV antibody test should also be considered.
A number of radiological techniques can be used to identify CSF fistulas, including cranial CT scans, CT cysternogram, radionucleotide cisternogram and specially weighted cranial MRI scans. Carrol AD et al., reported the case of a nine-year-old boy with recurrent meningitis whose ethmoidal defect was missed in initial CT scan just like our case [10]. It has to be accepted that this cohort of paediatric patients may require repeated and simultaneous application of varied radiological investigations to pinpoint the underlying subtle anatomical defect [8].
Conclusion
In conclusion, though HRCT scan of skull is preferred by many authors (for production of the best definitions of bony structures) as first choice, no single imaging modality is competent enough to diagnose a fistula in all the instances. Depending upon the clinical scenario a physician should consult an experienced radiologist before planning appropriate investigations to diagnose the aetiology of recurrent meningitis in an immunocompetent patient.
[1]. Yilmaz Ciftdogan D, Bayram N, Ozdemir Y, Bayraktaroglu S, Vardar F, A case of mondini dysplasia with recurrent streptococcus pneumoniae meningitisEur J Paediatr 2009 168(12):1533-35. [Google Scholar]
[2]. Tebruegge M, Curtis N, Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitisClin Microbiol Rev 2008 21(3):519-37. [Google Scholar]
[3]. Janocha-Litwin J, Simon K, Recurrent meningitis—a review of current literaturePrzeglad Epidemiologiczny 2013 67(1):41-45. [Google Scholar]
[4]. Drummond DS, De Jong AL, Giannoni C, Sulek M, Friedman EM, Recurrent meningitis in the paediatric patient—the otolaryngologist’s roleInt J Paediatr Otorhinolaryngol 1999 48(3):199-208. [Google Scholar]
[5]. Ginsberg L, Difficult and recurrent meningitisJ Neurol Neurosurg Psychiatry 2004 75(1):16-21. [Google Scholar]
[6]. Ginsberg L, Kidd D, Chronic and recurrent meningitisPract Neurol 2008 8(6):348-61. [Google Scholar]
[7]. Kline MW, Review of recurrent bacterial meningitisPaediatr Infect Dis J 1989 8:630-34. [Google Scholar]
[8]. Lieb G, Krauss J, Collman H, Schrod L, Sorensen N, Recurrent bacterial meningitisEur J Paediatr 1996 155:26-30. [Google Scholar]
[9]. Kohrmann M, Schellinger PD, Wetter A, Hahnel S, Nasal meningoencephalocele an unusual cause for recurrent meningitis. Case report and review of the literatureJ Neurol 2007 254:259-60. [Google Scholar]
[10]. Carrol ED, Latif AH, Misbah SA, Flood TJ, Abinun M, Clark JE, Lesson of the week: Recurrent bacterial meningitis: the need for sensitive imagingBMJ 2001 323:501-03. [Google Scholar]