Introduction
First recognized near the Ebola River valley during an outbreak in Zaire in 1976, Ebola Viruses have been identified as an emerging threat in recent years as it causes severe haemorrhagic fever in human with mortality rates ranging from 50 to 90% [1-3]. It is also impending biological threat. Recent epidemic of Ebola Virus Disease (EVD) in West Africa has accounted for more than 25,000 cases and 11,308 deaths [4]. Earlier this hazardous epidemic was controlled by identification isolation tactics/contact tracing but this was not sufficient and time needed a cure that is vaccine. The present review explores the potential targets to design a vaccine and status of currently available vaccine for protection against Ebola.
Structure and classification: Ebola virus and Marburg virus are two genera in the family Filoviridae. The genus Ebola virus includes five species (each represented by a single virus): Zaire Ebola virus (Ebola virus, EBOV), Sudan Ebola virus (Sudan virus, SUDV), Reston Ebola virus (Reston virus, RESTV), Taï Forest Ebola virus (Tai Forest virus, TAFV), and Bundibugyo Ebola virus (Bundibugyo virus, BDBV).
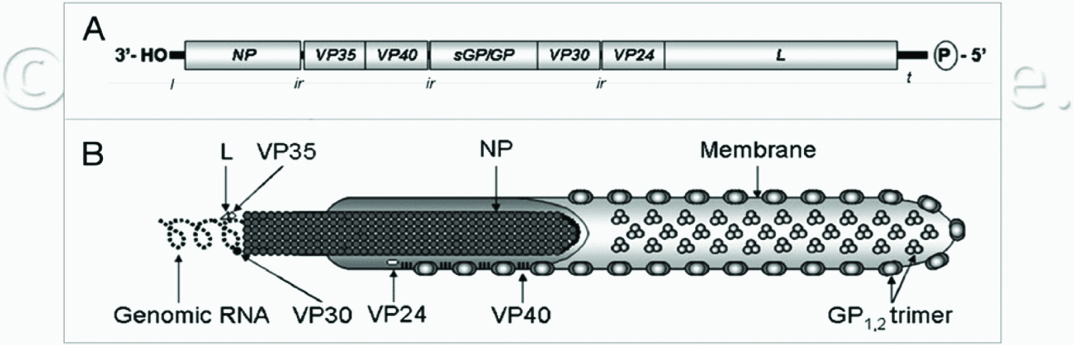
Ebola virus’s genome is a single stranded RNA, which is about 18-19 kb in size [5] containing seven genes which encode a Nucleoprotein (NP), four viral proteins (VP24, VP30, VP35 and VP40), a Glycoprotein (GP), and a RNA dependent RNA polymerase (L) [Table/Fig-1]. VP40 is the major matrix protein which regulates virion assembly [6]. GP mediates attachment to and entry into host cells.
Schematic representation of (A) organization of filovirus genomic RNA (ZEBOV depicted); l, Leader sequence; NP, nucleoprotein gene; VP, viral protein gene; GP, glycoprotein gene; L, RNA-dependent RNA polymerase gene; ir, intergenic region and (B) filovirus particle; NP, nucleoprotein; VP, viral protein gene; GP, glycoprotein gene; L, RNA-dependent RNA polymerase.
*From Richardson JS, Dekker JD, Croyle MA, Kobinger GP. Recent advances in Ebola virus vaccine development. Human Vaccines 2010; 6(6): 439-49.
*From Richardson JS, Dekker JD, Croyle MA, Kobinger GP. Recent advances in Ebola virus vac-cine development. Human Vaccines 2010; 6(6): 439-49.
Pathogenesis: The receptors required for cell binding and infection are not completely understood. The role of a folate related receptor as a cofactor to facilitate infection remains unclear [7]. Transferrin and DC-sign have both been proposed as cellular receptors involved in mediating filovirus entry through binding and internalization, although their real contribution to virus entry remains controversial [8]. Several lines of evidence suggest that the viral GP plays a key role in the manifestations of Ebola virus infection. Transmembrane form of GP helps Ebola virus to enter into target monocytes/macrophages. Release of cytokines from these cells after viral infection is responsible for increased vascular integrity causing inflammation and fever [9,10].
The pathogenesis of Ebola virus infection mimics in Guinea pigs, nonhuman primates and in human, therefore these animals have been used to study the pathogenesis of Ebola virus infection and to assess the efficacy of various vaccine approaches [11,12].
Clinical course of disease: Typically, Ebola virus infection incubation period varies from two to 21 days. Nonspecific flu-like symptoms such as fever, myalgia, and malaise are the initial manifestations. In later stage of infection, it results in severe bleeding, coagulation irregularities, gastrointestinal bleeding, haematological abnormalities like neutrophilia and lymphopenia. There is exaggerated inflammatory response due to cytokine release when reticulo endothelial cells encounter virus but they are not protective. Liver also gets affected and endothelial cell dysfunction leads to disseminated intravascular coagulopathy. The lethal stages include diffuse bleeding and hypotensive shock resulting into Ebola virus mortalities [13].
Currently available vaccines: A number of vaccines have been in development for Ebola over the years, but none are yet approved for use in human subjects. The main obstacle is the lack of safety data. The various immune evasion strategies utilized by the Ebola virus further limits the predictive power of animal models in forecasting expected efficacy in human subjects. The 2014 Ebola epidemic in West Africa has killed over 10,000 and its persistence has implied enormous pressure on scientists for developing new treatments and vaccines. An effective vaccine against Ebola might be the most effective way to control future epidemics. Several vaccines against Ebola, based on both inactivated and live viruses, are in different stages of clinical trials [Table/Fig-2].
Different type of vaccines in clinical trial or effective in Non Human Primates (NHPs).
| S. No. | Type ofVaccines | Key component | Efficacy | Adverse effect |
|---|
| 1 | Conventional Vaccines | Inactivation of EBOV by heat, formalin, or γ-irradiation | not effective | significant risk of reversion |
| 2 | Sub-Unit Vaccines (Non- Viral) | Ebola virus genes inserted into a DNA plasmid | Full protection was reported in mice and later in guinea pigs with optimized strategies | - |
| 3 | Virus-like Particles (VLPs) as a Candidate Vaccine | EBOV-like particles generated by the expression of VP40 alone or along with GP. | Full Protection | - |
| 4 | Vector-Based Vaccines | 1. not be recommended for use in immuno- compromised individuals2. Pre existing immunity against viral vector decreases immune response3. Multiple doses required |
| a. Vaccinia virus-based vaccines. | recombinant vaccinia virus | incomplete protection in guinea pigs, no protection in NHPs |
| b. VEE virus-like replicon particles | recombinant Venezuelan equine encephalitis (VEE) virus | Fully protective in mice, no protection in NHPs |
| c. Adenovirus- Based Vaccines. | recombinant human adenovirus serotype-5 (AdHu5) virus | complete protection in NHPs |
| d. Vesiculovirus (VSV)-based candidate vaccines. | recombinant VSV | 100% protection in mice, 50% protection in guinea pigs and NHPs |
Conventional Vaccines: The base of conventional vaccines is EBOV neutralization by heat, chemical or γ-irradiation. However most of candidates did not developed protective immune response with inactivated virus with/without liposome or adjuvant even after alteration of route of administration from intramuscular to sub cutaneous injection [14-16]. The probable risk of reversion associated with live attenuated filovirus vaccine candidates, as evident from studies [17], have shown the retention of virulence of mouse adapted and guinea pig adapted Ebola virus in NHPs, making safety a major concern.
Sub-unit vaccines (Non viral): To elicit an immune response to the corresponding virus particle, Ebola virus genes are inserted into a DNA plasmid and then injected directly into a patient’s muscle. The major advantage of DNA vaccines are generation of antibody and cytotoxic T lymphocytes [18]. Additionally, they are easily manufactured, cost effective and are stable for storage and shipping at ambient temperatures [19]. Several methods of DNA vaccine delivery have been used including direct administration into tissue via syringe, gene gun delivery of DNA, or electroporation of muscle tissue following injection of DNA. Vaccines have been evaluated in mice, guinea pigs with full protection achieved against virus antigens GP, NP, VP35 or VP40 [12,20,21].
Virus-Like Particles (VLPs) as a Candidate vaccine: There are no safety issues with VLP vaccines as they lack NP, VP24, VP30, VP35 and L proteins as well as EBOV RNA genome. VLP can be generated by expression of filoviral antigen VP40 alone or along with GP [22-25]. Frequently, vector based vaccines expressing EBOV epitopes can be subject to host pre-existing immunity to the vector backbone, thereby inhibiting vaccine efficacy by preventing an immune response to the antigen. But VLP based vaccines bypasses pre-existing immunity issue to vector backbone.
Mice vaccinated with VLPs expressing ZEBOV VP40 and ZEBOV GP followed by either two booster injections, or one booster with QS-21 adjuvant, resulted in complete protection from a challenge with a lethal dose of mouse-adapted ZEBOV [26]. In these experiments, this vaccine generated CD4+ and CD8+ T cells specific to GP and VP40 peptides, mouse IgG responses, and B cell activation with no toxic cytokine response [26].
Vector based vaccines: Vaccines can be generated using viruses as vaccine vectors. The candidate genes encoding EBOV antigen are inserted and expressed from the viral carrier. Viral vectors can be replication competent or defective, each having its own advantages and disadvantages. Replication competent viral vector based vaccines are not useful for immunocompromised population but they can produce strong and long-lasting immune responses following immunization. On the other hand, replication defective viral vector based vaccines can be used safely among all individuals but they need to be administered in multiple doses to achieve optimal immunity.
Vaccinia virus based vaccines: Vaccines based on recombinant vaccinia virus expressing ZEBOV GP, VP24, VP35 and VP40 were tested in the guinea pig model. Following lethal ZEBOV challenge, a recombinant vaccinia virus expressing ZEBOV GP afforded incomplete protection in guinea pigs. None of the other recombinant vaccinia-based vaccines expressing the other ZEBOV antigens protected the guinea pigs from succumbing to the infection [27]. Although neutralizing antibodies against ZEBOV were detected, NHPs administered recombinant vaccinia virus expressing ZEBOV GP did not protect the animals against lethal homologous challenge [16].
VEE virus like replicon particles: Venezuelan Equine Encephalitis (VEE) virus has a positive-sense RNA genome. The VEE virus structural genes can be replaced by EBOV NP or GP, generating replicons that are single cycle and propagation deficient. VEE replicons expressing ZEBOV GP (VEE-GP), NP (VEE-NP), or a combination of GP + NP (VEE-GP + NP) were shown to be fully protective in mice challenged with ZEBOV. Vaccination with VEE-GP, VEE-NP or VEE-GP + NP followed by two booster injections resulted in no protection of NHPs challenged with ZEBOV [16].
Adenovirus based vaccines: Initially human adenovirus serotype-5 (AdHu5) was mostly used as the adenovirus-based vaccine prototype. The recombinant AdHu5 backbone contains deletions in the intermediate early E1 gene. Additional deletions to the E3 and E4 regions of AdHu5 have increased the carrying capacity of this vector to approximately 8 kb. The initial success generated from boosting a DNA vaccine combining ZEBOV GP + ZEBOV NP + SEBOV GP + ICEBOV GP with an additional booster injection of recombinant adenovirus expressing ZEBOV GP (AdHu5-ZGP) has encouraged the development of more replication-deficient adenovirus-based strategies [28]. A single dose of AdHu5-GP mixed with AdHu5 expressing NP (AdHu5-NP) offered complete protection in NHPs against lethal ZEBOV challenge [28,29]. There are problems associated with the use of AdHu5-based vaccine platforms. Exposure to naturally occurring adenoviruses within the human population can lead to the development of neutralizing antibodies, potentially compromising the efficacy of adenovirus based vaccine administration [30].
Vesiculovirus (VSV) based candidate vaccines: Candidate vaccines based on replication competent recombinant VSV can grow to high titers and induce a strong humoral and cellular response in humans [31]. VSV expressing ZEBOV antigens have been made by manipulation of an infectious VSV cDNA clone. Mice vaccinated and boosted with recombinant VSV expressing ZEBOV GP (VSV-GP) survived a challenge of ZEBOV with complete protection [32]. Full protection of ZEBOV challenged mice vaccinated with VSV-GP was achieved when administered through the I.M., I.P., or mucosal route. When NHPs were challenged with ZEBOV following vaccination with VSV-GP, 100% protection was observed [33].
Importantly, VSV based vaccine platforms have also been shown to be an effective post exposure treatment regimen. Mice and guinea pigs challenged with ZEBOV were administered VSV-GP 24 hours post exposure resulting in 100% and 50% protection, respectively [34]. Fifty percent protection was achieved in NHPs immunized with the recombinant VSV-GP, 20–30 minutes post exposure to ZEBOV [34]. Progress has been made using the VSV-based platform for single dose blended vaccines, capable of protection against several EBOV species. Full survival and protection was observed in the NHPs after administering the recombinant VSV vaccine expressing SEBOV GP, ZEBOV GP or ICEBOV GP following challenge with SEBOV, ZEBOV or ICEBOV [35]. Recombinant VSV-GP vaccine given 28 days before challenge either I.N., orally (OR) or I.M. protected NHPs against a lethal challenge of ZEBOV [36]. ZEBOV GP-specific T- and B-cell responses were induced in the I.N. and OR groups. These groups also produced the most IFNγ and IL-2 secreting cells, in addition to long term memory responses following immunization and challenge [36].
Antigen express – Ii-key hybrid technology: The vaccines are produced by adding a small peptide (Ii-Key), derived from the MHC Class II-associated invariant chain (Ii) protein, onto the antigen of interest during synthesis. Ii-Key Hybrid vaccines are peptide-based agents that are engineered to stimulate strong and specific CD4+ T cell responses. The Ii-Key addition significantly augments MHC Class II loading and presentation by directly charging MHC Class II molecules on the surface of antigen presenting cells, bypassing the usual intracellular processing mechanism. By this means, Ii-Key hybrids effectively hijack MHC Class II molecules on the surface of any antigen presenting cell to potently activate CD4+ T helper cells in an antigen-specific manner, resulting in stronger cellular and humoral immunity through the interaction of CD4+ cells with CD8+ and B cells, respectively [37].
The other advantages of the technology is that synthetic production methods are rapid, cost effective, scalable, and enable the speedy production of very large batches in a matter of months. The activity of Ii-Key/antigen hybrids has been further demonstrated in Phase I and II clinical trials involving over 400 patients or volunteers, accumulating a wealth of safety and immunological data. In particular, Ii-Key Hybrid peptides have been shown to be safe, well tolerated, and produced the desired immunological response [38,39]. Of note is that a recent long term follow up to a Phase I study showed a specific and undiminished immunological response even three years after receiving an Ii-Key hybrid vaccine [40]. Therefore, it is believed that Antigen Express Ii-Key Hybrid technology represents an excellent opportunity for the rapid development of an effective Ebola vaccine.
Human vaccines [Table/Fig-3]: Three potential vaccines which had shown promising results in animals have now been entered into human trials. One is produced by GlaxoSmithKline (GSK) and the National Institutes of Health in the United States, another is being developed by the Public Health Agency of Canada in collaboration with Merck. Johnson and Johnson with company Bavarian Nordic are third to enter human testing.
Human vaccines in clinical trial.
| S. No. | PharmaceuticalCompany | Vaccine | Content | Status ofTrial |
|---|
| 1 | GlaxoSmithKline (GSK) | cAd3-EBO | type chimpanzee adenovirus type 3 (ChAd3), as a carrier | Phase 1 |
| 2 | Public Health Agency of Canada with Merck | rVSV-ZEBOV | attenuated vesicular stomatitis virus | Phase 1 |
| 3 | Johnson and Johnson with company Bavarian Nordic | Ad26.ZEBOV/MVA-BN-Filo | replication-defective adenovirus-vector | Phase 1 |
| 4 | Novavax | EBOV GP Nanoparticle | Baculovirus- derived Ebola GP nanoparticle + Matrix M adjuvant | Phase 1 |
| 5 | NovaSep | rVSVN4CT1 EBOV (Profectus) | recombinant Ad5 virus--vector | Pre clinical trial |
| 6 | Niaid with IDT Biologika | Rabies EBOV-GP | vector based combination trivalent (Zaire, Sudan, Marburg) | Pre clinical trial |
| 7 | Lonza | VXA ZEBOV -GP (VaxArt) | recombinant VSV- vector vaccine | Pre clinical trial |
cAd3-EBO by GSK: This vaccine was developed by the NIH’s National Institute of Allergy and Infectious Diseases (NIAID) in association with a biotechnology company Okairos, acquired by GSK in 2013. The chimpanzee adenovirus type 3 (ChAd3), is used as a carrier to deliver benign genetic material of the Zaire strain, which is responsible for the current Ebola outbreak in West Africa [41] GSK and NIH has been working in collaboration to accelerate development in response to the current Ebola epidemic.
Analysis of trial data shows that candidate vaccine has acceptable safety and high immunological profile. Based on this immunity development data of West African population GSK has designed highly precise dosage level for next stage of testing. The cAd3-EBO vaccine may also be used in a heterologous prime-boost strategy with a recombinant Modified Vaccinia Ankara (MVA) GP booster vaccine (MVA-BN-Filo) manufactured by Bavarian Nordic [42].
Merck’s Ebola vaccine: The rVSV-ZEBOV vaccine is a recombinant replication competent vaccine containing vasicular stomatitis virus as a vector in which one gene of VSV has been replaced with the gene that codes for the outer protein of the Zaire Ebola virus. It was initially developed by the Public Health Agency of Canada which later licensed it to Bio Protection Systems (BPS), a wholly owned subsidiary of New Link Genetics (NLG). In November 2014, NLG licensed it to Merck Vaccines for the research, development, manufacture, and distribution of the vaccine. This is a single-dose, live-virus replication-competent monovalent recombinant vaccine based on an attenuated Vesicular Stomatitis Virus (VSV) platform [43].
Johnson and Johnson’s Ebola vaccine: Ad26.ZEBOV/MVA-BN-Filo: a monovalent, live-virus replication-defective adenovirus-vector vaccine expressing GP from the Zaire Ebola virus (Ad26. ZEBOV) applied in a heterologous prime boost strategy with MVA-BN-Filo, a booster vaccine. Ad26. ZEBOV is manufactured by Janssen Pharmaceuticals, a subsidiary of Johnson and Johnson (J and J) [44]. MVA-BN-Filo is a recombinant multivalent replication-defective MVA booster vaccine containing the GP from Zaire Ebola virus, Sudan virus, and Marburg virus. MVA-BN-Filo is manufactured by Bavarian Nordic [45]. Crucell Holland BV, one of the Janssen Pharmaceutical Companies of J and J, licensed the MVA-BN-Filo booster from Bavarian Nordic for use with the Ad26- ZEBOV vaccine. In January, Johnson and Johnson said it had begun administering its vaccine to healthy volunteers in the United Kingdom. This is under Phase 1 clinical trial.
EBOV GP Nanoparticle (Novavax): This is a Baculo virus based vaccine containing Ebola virus GP with matrix adjuvant, developed by Novavax. Preclinical results have shown high immunogenicity in mice, rabbits and baboons as well as 100% protection in lethal mouse challenge [46]. In January 2015, 1st NHP challenge was initiated in C macaque. In the same year, clinical trials were started on 200 healthy young adults using antigen in different doses and with or without adjuvant. Eficacy of 1 vs 2 dose regimen were also checked.
Preclinical trails: rVSVN4CT1 EBOV (Profectus): It is a recombinant monovalent (Zaire) vaccine containing Ad5 virus--vector which is replication-incompetent live virus. Manufacturing is done at Nova Sep. Complete protection was seen following single dose in murine and NHP models during pre clinical studies. Phase 1 Clinical trials have been started in 2015 in USA [47].
Rabies EBOV-GP (TJU): It’s a trivalent (Zaire, Sudan, Marburg) rabies vector based vaccine for VHF and rabies which contain replication-competent live virus. Complete protection was seen following single dose in NHP during pre-clinical Studies. Clinical trials are expected to be started in mid 2015 in USA [48].
VXA ZEBOV -GP (VaxArt): Another recombinant, monovalent (Zaire) VSV-vector vaccine which uses replication-competent virus, Manufacturing is done at Lonza. In Pre clinical Studies, NHP challenge studies showed complete protection following single dose. Clinical trials are expected to be started in 2015 in USA.
Conclusion
As for now, neither a specific treatment nor a vaccine against Ebola virus licensed for use in humans is available. However, since last decade numerous vaccines have been developed showing high immunity against virus in non-human primates. Among these vaccines are recombinant Adenoviruses (Ad5/chAd3), recombinant VSV, and recombinant Human Parainfluenza viruses vaccines. Vaccination offers a promising intervention to prevent infection and limit spread. Even though, more work needs to be done to determine the effectiveness and clinical significance of all those vaccine candidates which are being in trial phase currently.
[1]. Bowen ET, Lloyd G, Harris WJ, Platt GS, Baskerville A, Vella EE, Viral haemorrhagic fever in southern Sudan and northern Zaire. Preliminary studies on the aetiological agentLancet 1977 309(8011):571-73. [Google Scholar]
[2]. Peters CJ, Khan AS, Filovirus diseasesCurr Top Microbiol Immunol 1999 235:85-95. [Google Scholar]
[3]. Sanchez A, Khan AS, Zaki SR, Nabel GJ, Ksiazek TG, Peters CJ, Knipe DM, Howley PM, Filoviridae: Marburg and Ebola virusesFields virology 2001 Philadelphia, PALippincott, Williams and Wilkins:1279-1304. [Google Scholar]
[4]. Centers for disease control and preventionEbola outbreak in West Africa - Case counts 2014 Available at http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html (accessed 16 October 2015) [Google Scholar]
[5]. Regnery RL, Johnson KM, Kiley MP, Virion nucleic acid of Ebola virusJ Virol 1980 36:465-69. [Google Scholar]
[6]. Elliott LH, Kiley MP, McCormick JB, Descriptive analysis of Ebola virus proteinsVirology 1985 147:169-76. [Google Scholar]
[7]. Chan SY, Empig CJ, Welte FJ, Speck RF, Schmaljohn A, Kreisberg JF, Goldsmith MA, Folate receptor is a cofactor forcellular entry by Marburg and Ebola virusesCell 2001 106:117-26. [Google Scholar]
[8]. Alvarez CP, Lasala F, Carrillo J, Muniz O, Corbi AL, Delgado R, C-type lectins DC-SIGN and L-SIGN mediate cellular entry by Ebola virus in cis and in transJ Virol 2002 76:6841-44. [Google Scholar]
[9]. Ströher U, West E, Bugany H, Klenk HD, Schnittler HJ, Feldmann H, Infection and activation of monocytes by Marburg and Ebola virusesJ Virol 2001 75:11025-33. [Google Scholar]
[10]. Yang ZY, Duckers HJ, Sullivan NJ, Sanchez A, Nabel EG, Nabel GJ, Identification of the Ebola virus glycoprotein as the main viral determinant of vascular cell cytotoxicity and injuryNat Med 2000 6:886-89. [Google Scholar]
[11]. Wyers M, Formenty P, Cherel Y, Guigand L, Fernandez B, Boesch C, Histopathological and immunohistochemical studies of lesions associated with Ebola virus in a naturally infected chimpanzeeJ Infect Dis 1999 179(suppl 1):S54-S59. [Google Scholar]
[12]. Xu L, Sanchez A, Yang Z, Zaki SR, Nabel EG, Nichol ST, Nabel GJ, Immunization for Ebola virus infectionNat Med 1998 4:37-42. [Google Scholar]
[13]. Colebunders R, Borchert M, Ebola haemorrhagic fever—A reviewJ Infect 1999 40:16-20. [Google Scholar]
[14]. Ignatyev GM, Agafonov AP, Streltsova MA, Kashentseva EA, Inactivated Marburg virus elicits a nonprotective immune response in Rhesus monkeysJ Biotechnol 1996 44:111-18. [Google Scholar]
[15]. Lupton HW, Lambert RD, Bumgardner DL, Moe JB, Eddy GA, Inactivated vaccine for Ebola virus efficacious in guinea pig modelLancet 1980 2:1294-95. [Google Scholar]
[16]. Geisbert TW, Pushko P, Anderson K, Smith J, Davis KJ, Jahrling PB, Evaluation in nonhuman primates of vaccines against Ebola virusEmerg Infect Dis 2002 8:503-07. [Google Scholar]
[17]. Fisher-Hoch SP, Platt GS, Neild GH, Southee T, Baskerville A, Raymond RT, Pathophysiology of shock and haemorrhage in a fulminating viral infection (Ebola)J Infect Dis 1985 152:887-94. [Google Scholar]
[18]. Vanderzanden L, Bray M, Fuller D, Roberts T, Custer D, Spik K, DNA vaccines expressing either them GP or NP genes of Ebola virus protect mice from lethal challengeVirology 1998 246:134-44. [Google Scholar]
[19]. Robinson HL, Pertmer TM, DNA vaccines for viral infections: Basic studies and applicationsAdv Virus Res 2000 55:1-74. [Google Scholar]
[20]. Riemenschneider J, Garrison A, Geisbert J, Jahrling P, Hevey M, Negley D, Comparison of individual and combination DNA vaccines for B anthracis, Ebola virus, Marburg virus and Venezuelan equine encephalitis virusVaccine 2003 21:4071-80. [Google Scholar]
[21]. Mellquist-Riemenschneider JL, Garrison AR, Geisbert JB, Saikh KU, Heidebrink KD, Jahrling PB, Comparison of the protective efficacy of DNA and baculovirus-derived protein vaccines for EBOLA virus in guinea pigsVirus Res 2003 92:187-93. [Google Scholar]
[22]. Kolesnikova L, Berghofer B, Bamberg S, Becker S, Multivesicular bodies as a platform for formation of the Marburg virus envelopeJ Virol 2004 78:12277-87. [Google Scholar]
[23]. Swenson DL, Warfield KL, Negley DL, Schmaljohn A, Aman MJ, Bavari S, Virus-like particles exhibit potential as a pan-filovirus vaccine for both Ebola and Marburg viral infectionsVaccine 2005 23:3033-42. [Google Scholar]
[24]. Wahl-Jensen V, Kurz SK, Hazelton PR, Schnittler HJ, Stroher U, Burton DR, Role of Ebola virus secreted glycoproteins and virus-like particles in activation of human macrophagesJ Virol 2005 79:2413-19. [Google Scholar]
[25]. Watanabe S, Watanabe T, Noda T, Takada A, Feldmann H, Jasenosky LD, Production of novelebola virus-like particles from cDNAs: An alternative to Ebola virus generation by reverse geneticsJ Virol 2004 78:999-1005. [Google Scholar]
[26]. Warfield KL, Olinger G, Deal EM, Swenson DL, Bailey M, Negley DL, Induction of humoral and CD8+T cell responses are required for protection against lethal Ebola virus infectionJ Immunol 2005 175:1184-91. [Google Scholar]
[27]. Chepurnov AA, Ternovoi VA, Dadaeva AA, Dmitriev IP, Sizikova LP, Volchkov VE, Immunobiological properties of vp24 protein of Ebola virus expressed by recombinant vaccinia virusVopr Virusol 1997 42:115-20. [Google Scholar]
[28]. Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ, Development of a preventive vaccine for Ebola virus infection in primatesNature 2000 408:605-09. [Google Scholar]
[29]. Sullivan NJ, Geisbert TW, Geisbert JB, Shedlock DJ, Xu L, Lamoreaux L, Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPsPLoS Med 2006 3:e177 [Google Scholar]
[30]. Kobinger GP, Feldmann H, Zhi Y, Schumer G, Gao G, Feldmann F, Chimpanzee adenovirus vaccine protects against Zaire Ebola virusVirology 2006 346:394-401. [Google Scholar]
[31]. Bukreyev A, Skiadopoulos MH, Murphy BR, Collins PL, Non-segmented negative-strand viruses as vaccine vectorsJ Virol 2006 80:10293-306. [Google Scholar]
[32]. Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Moller P, Wagner R, Properties of replication competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arena virusesJ Virol 2004 78:5458-65. [Google Scholar]
[33]. Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg virusesNat Med 2005 11:786-90. [Google Scholar]
[34]. Feldmann H, Jones SM, Daddario-DiCaprio KM, Geisbert JB, Stroher U, Grolla A, Effective post exposure treatment of Ebola infectionPLoS Pathog 2007 3:2 [Google Scholar]
[35]. Geisbert TW, Geisbert JB, Leung A, Daddario- DiCaprio KM, Hensley LE, Grolla A, Single-injection vaccine protects nonhuman primates infection with marburg virus and three species of Ebola virusJ Virol 2009 83:7296-304. [Google Scholar]
[36]. Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, Dick D, Mucosal immunization of cynomolgus macaques with the VSVDeltaG/ZEBOVGP vaccine stimulates strong Ebola GP-specific immune responsesPLoS One 2009 4:5547 [Google Scholar]
[37]. Erskine CL, Krco CJ, Hedin KE, Borson ND, Kalli KR, Behrens MD, MHC class II epitope nesting modulates dendritic cell function and improves generation of antigen-specific CD4 helper T cellsJ Immunol 2011 187(1):316-24. [Google Scholar]
[38]. Perez SA, Kallinteris NL, Bisias S, Tzonis PK, Georgakopoulou K, Varla-Leftherioti M, Results from a phase I clinical study of the novel Ii-Key/HER- 2/neu(776-790) hybrid peptide vaccine in patients with prostate cancerClin Cancer Res 2010 16(13):3495-506. [Google Scholar]
[39]. Riedmann EM, Positive Phase II interim data on AE37 cancer vaccine releasedHum Vaccin Immunother 2012 8(2):152 [Google Scholar]
[40]. Perez SA, Anastasopoulou EA, Tzonis P, Gouttefangeas C, Kalbacher H, Papamichail M, AE37 peptide vaccination in prostate cancer: A 4-year immunological assessment updates on a Phase I trialCancer Immunol Immunother 2013 62(10):1599-608. [Google Scholar]
[41]. Ledgerwood JE, DeZure AD, Stanley DA, Novik L, Enama ME, The VRC 207 Study TeamChimpanzee adenovirus vector Ebola vaccine- preliminary reportN Engl J Med 2014 [Google Scholar]
[42]. Stanley DA, Honko AN, Asiedu C, Trefry JC, Lau-Kilby AW, Johnson JC, Chimpanzee adenovirus vaccine generates acute and durable protective immunity against Ebolavirus challengeNat Med 2014 20:1126-29. [Google Scholar]
[43]. Feldmann H, Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infectionsJ infect Dis 2011 204(suppl 3):S1075-81. [Google Scholar]
[44]. Van Hoof J, Janssen Ebola vaccine emergency track program: Review of Ebola vaccines in Phase 1 clinical evaluationPresented at World Health Organization Meeting, 8 January 2015 Janssen R and DAvailable at: http://www.who.int/mediacentre/events/2015/S2.1_Janssen_ZEBOV_vaccine-Revised.pdf (accessed 16 September 2015) [Google Scholar]
[45]. Bavarian Nordic Infectious DiseasesMVA-BN Filo: Ebola and Marburg vaccine candidateAvailable: http://clinicaltrials.gov/ct2/show/NCT02240875 (accessed 5 November 2015) [Google Scholar]
[46]. ClinicalTrials.govStudy to evaluate the immunogenicity and safety of an Ebola virus (EBOV) glycoprotein (GP) vaccine in healthy subjectsAvailable: https://clinicaltrials. gov/ct2/show/NCT02370589 (accessed 14 September 2015) [Google Scholar]
[47]. Clinical Trials.govTrial to Evaluate Safety and Immunogenicity of an Ebola Zaire Vaccine in Healthy AdultsAvailable: https://clinicaltrials.gov/ct2/show/NCT02718469 (accessed 16 October 2015) [Google Scholar]
[48]. Willet M, Kurup D, Papaneri A, Wirblich C, Hooper JW, Kwilas SA, Preclinical development of inactivated rabies virus based polyvalent vaccine against rabies and filovirusesJ Infect Dis 2015 212(suppl 2):S414-24. [Google Scholar]