The Effect of Cavity Design on Fracture Resistance and Failure Pattern in Monolithic Zirconia Partial Coverage Restorations - An In vitro Study
Madhavareddy Sri Harsha1, Mynampati Praffulla2, Mandava Ramesh Babu3, Gudugunta Leneena4, Tejavath Sai Krishna5, G Divya6
1 General Practitioner, Consultant Endodontist, Guntur, Andhra Pradesh, India.
2 Senior Lecturer, Department of Conservative Dentistry and Endodontics, Drs Sudha and Nageswara Rao Siddhartha Institute of Dental Sciences, Vijayawada, Andhra Pradesh, India.
3 Professor and Head, Department of Conservative Dentistry and Endodontics, Drs Sudha and Nageswara Rao Siddhartha Institute of Dental Sciences, Vijayawada, Andhra Pradesh, India.
4 Lecturer, Department of Conservative Dentistry and Endodontics, Amist University, Kuala Lumpur, Wilayah Persekutuan Kuala Lumpur, Malaysia.
5 Senior Lecturer, Department of Conservative Dentistry and Endodontics, Mamata Dental College, Khammam, Telangana, India.
6 Senior Lecturer, Department of Pediatric and Preventive Dentistry, St. Joseph Dental College, Eluru, Andhra Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mynampati Praffulla, D. No 76-5-14, Bhagat Singh Road, Bhavanipuram, Vijayawada, Andhra Pradesh, India.
E-mail: praffullamynampati@yahoo.com
Introduction
Cavity preparations of posterior teeth have been frequently associated with decreased fracture strength of the teeth. Choosing the correct indirect restoration and the cavity design when restoring the posterior teeth i.e., premolars was difficult as it involves aesthetic, biomechanical and anatomical considerations.
Aim
To evaluate the fracture resistance and failure pattern of three different cavity designs restored with monolithic zirconia.
Materials and Methods
Human maxillary premolars atraumatically extracted for orthodontic reasons were chosen. A total of 40 teeth were selected and divided into four groups (n=10). Group I-Sound teeth (control with no preparation). Group II-MOD Inlay, Group III-Partial Onlay, Group IV-Complete Onlay. Restorations were fabricated with monolithic partially sintered zirconia CAD (SAGEMAX- NexxZr). All the 30 samples were cemented using Multilink Automix (Ivoclar) and subjected to fracture resistance testing using Universal Testing Machine (UTM) (Instron) with a steel ball of 3.5 mm diameter at crosshead speed of 0.5 mm/minute. Stereomicroscope was used to evaluate the modes of failure of the fractured specimen. Fracture resistance was tested using parametric one way ANOVA test, unpaired t-test and Tukey test. Fracture patterns were assessed using non-parametric Chi-square test.
Results
Group IV (Complete Onlay) presented highest fracture resistance and showed statistical significant difference. Group II (MOD Inlay) and Group III (Partial Onlay) showed significantly lower values than the Group I (Sound teeth). However, Groups I, II and III presented no significant difference from each other. Coming to the modes of failure, Group II (MOD Inlay) and Group III (Partial Onlay) presented mixed type of failures; Group IV (Complete Onlay) demonstrated 70% Type I failures.
Conclusion
Of the three cavity designs evaluated, Complete Onlay had shown a significant increase in the fracture resistance than the Sound teeth.
Complete onlay, MOD Inlay, Partial onlay, Zirconia CAD
Introduction
A sound tooth rarely fractures during normal mastication. The loss of tooth structure due to caries, cavity preparation or trauma reduces the tooth resistance compared to sound tooth. Reeh ES et al., reported that one wall loss during cavity preparation along with isthmus width approximately one third of the intercuspal distance resulted in around 20% decrease in stiffness. The cavity preparation that destroyed one marginal ridge resulted in a 46% loss in tooth stiffness and a MOD preparation resulted in a 63% decrease in stiffness [1]. However, it is a big challenge to regain the fracture resistance of tooth lost due to cavity preparation.
Several cavity designs for a MOD preparation were proposed for the posterior teeth based on the caries extent and the reinforcement of the cusp. In the literature there is no standard cavity design for premolar teeth. Cubas GB et al., reported that inlays restored with ceramic restorations (Vitadur Alpha) performed better than partial and complete onlays [2]. According to Casselli DS et al., adhesive inlay restorations, irrespective of the type of composite resin and light activation technique used, restored the fracture resistance of intact teeth compared to partial onlay [3]. Yamada Y et al., reported that MOD cavity preparations on endodontically treated maxillary premolars could be restored successfully by cast onlay and inlay restorations luted with adhesive resin cement [4]. Kantardzic I et al., evaluated the stress values in cavity preparation of premolar and concluded that stress values in dental tissues and restorative material can be revealed by palatal cusp reduction [5]. The main factors which influence the fracture resistance are the depth of the cavity, intercuspal distance, restorative material, the type of cementing agent and the fracture load.
Currently, there is an increased demand for aesthetic restoration in the posterior dentition.
The material of choice may be direct or indirect composite and ceramic. Among the options available ceramic restorations could be the alternative material for the posterior teeth with extensive loss of tooth structure. Compared to resin composite restorations these restorations have superior aesthetics, chemical durability, biocompatibility and resistance to compression and wear [2].
With the recent development of Computer-Aided Design/Computer-Assisted Manufacture (CAD-CAM) technologies and new ceramic materials, it is possible to mill full contour ceramic restorations without veneering. This full contour restoration can avoid ceramic chipping and reduce wear of antagonists.
Zirconia, a crystalline dioxide of zirconium was proposed by Gravie in 1975 [6]. In zirconia the crystals are organized in Monoclinic (M), Cubic (C) and Tetragonal (T) patterns.
Yttrium stabilized zirconia, also known as Tetragonal Zirconia Polycrystal (TZP) is presently used. Its mechanical strength, chemical properties, toughness, and Young’s modulus (210 GPa) was similar to that of stainless steel alloy (193 GPa). Compression resistance and resistance to traction was as high as 2000 MPa and 900-1200 MPa respectively [7]. The high initial strength and fracture toughness of zirconia is related to its transformation toughening phenomenon i.e., when stress is applied on zirconia the cracking energy is created which causes tetragonal monoclinic transformation with a volume expansion of 3 to 5%. This expansion will finally lead to compressive stresses at the edge of the induced crack front, which require extra energy for the crack to propagate. Because of its excellent mechanical properties it is called as ‘Ceramic Steel’ [7].
Considering these properties high strength monolithic zirconia restorations are indicated in posterior regions, where aesthetics do not rank first and in patients with limited occlusal space or those suffering from bruxism. However, limited data is available regarding selection of appropriate cavity design for premolars and its influence on fracture resistance. The aim of the present study was to evaluate the fracture resistance and failure pattern of three different cavity design i.e., MOD Inlays, Partial Onlays and Complete Onlays restored with monolithic zirconia.
Materials and Methods
This in vitro study was conducted in the Department of Conservative Dentistry and Endodontics at Drs Sudha and Nageswara Rao Siddhartha Institute of Dental Sciences, Gannavaram, Andhra Pradesh, India. The study was performed for the time period of one month i.e., in July 2016. Human maxillary first premolars which were extracted atraumatically for orthodontic reasons were collected and observed under microscope at 10X magnifications. Teeth with cracks were excluded and finally forty sound teeth were selected [4]. The power of the study was 80%. The teeth were stored in 0.5% chloramine solution (Oxford Lad Chem., India) before use. The roots of the teeth were embedded in acrylic resin 2 mm below the cementoenamel junction and parallel to the long axis of teeth. Periodontal ligament simulation was not performed.
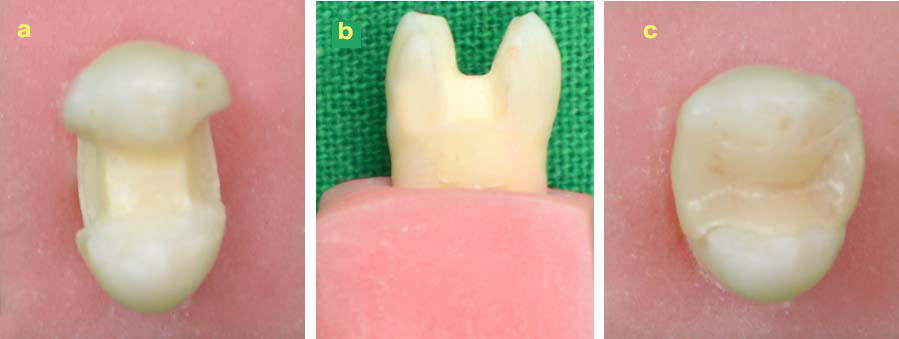
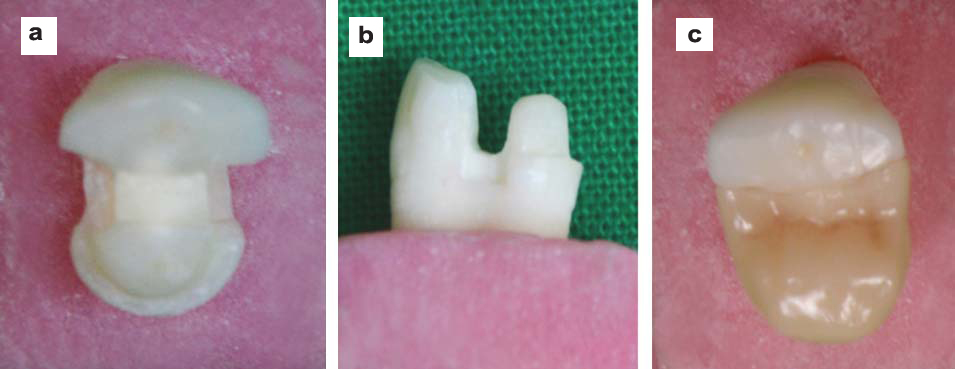
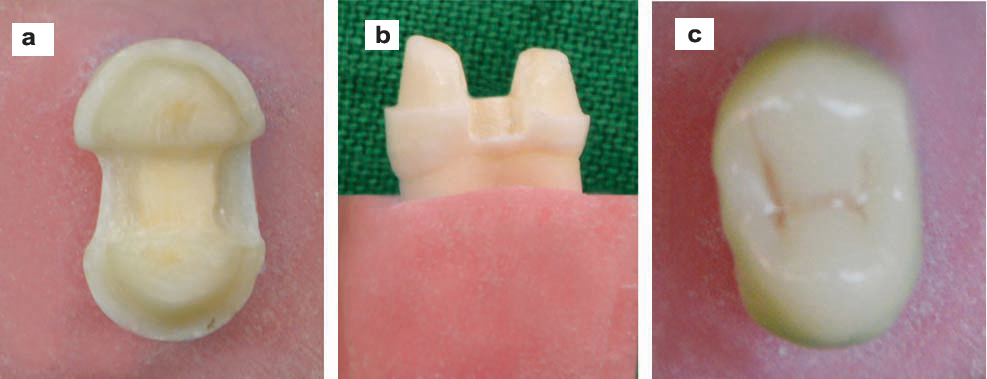
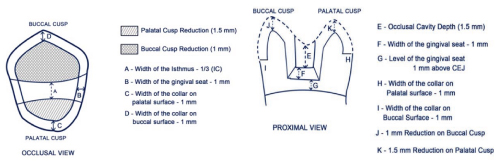
Among 40 teeth, 10 teeth were randomly selected for the control group, i.e., Sound teeth (Group I) and remaining teeth were divided into three groups based on the cavity designs. MOD cavities were prepared using FG 271 and FG169L carbide burs (SS White, Lake wood, USA). In Group II-MOD Inlay, cavity preparations were done with occlusal cavity width kept at 1/3rd the intercuspal distance, the cavity pulpal floor depth was 1.5 mm at the central groove area and each wall with a taper of 3°. In the proximal box, gingival seat was placed 1 mm above the cementoenamel junction and mesiodistal width of the seat was kept to 1 mm [Table/Fig-1]. In Group III-Partial Onlay, preparations were similar to Group II but the palatal cusp was reduced by 1.5 mm with a collar of 1 mm [Table/Fig-2]. In Group IV -Complete Onlay preparations were similar to Group III with palatal cusp reduction by 1.5 mm with a collar of 1 mm width and buccal cusp reduction of 1 mm with collar of 1 mm [Table/Fig-3, 4].
Group II - MOD Inlay cavity preparation: a) Occlusal view; b) Proximal view; c) Zirconia restoration.
Group III - MOD Onlay with buccal cusp preservation and palatal cusp reduction (Partial Onlay); a) Occlusal view; b) Proximal view; c) Zirconia restoration.
Group IV - MOD Onlay with buccal and palatal cusp reduction (Complete Onlay): a) Occlusal view; b) Proximal view; c) Zirconia restoration.
Schematic diagram of occlusal and proximal view of Complete Onlay (Group IV). IC-Intercuspal distance; CEJ- Cementoenamel Junction
Load application using Universal Testing Machine (UTM) for testing fracture resistance.

Restorations were fabricated with monolithic partially sintered zirconia CAD (SAGEMAX- NexxZr) using Computer Aided Design/ Computer Aided Manufacturing (CAD/CAM) i.e., Delcam Dent CAD and Roland milling machine. All the restorations were cemented using Multilink Automix (Ivoclar Vivadent, Schaan, Lichtenstein) according to the manufacturers recommendation. Prior to cementation, the fitting surface of the restorations were sand blasted with air borne particle abrasion with 27 µm aluminium oxide at 30 psi followed by the application of silane coupling agent (Metal/Zirconia Primer) for 180 seconds. Multilink primer A and B were mixed and applied to the cavity preparations. The restorations were finally cemented and light cured on all restored surfaces for 40 seconds.
The samples were stored in water at 37°C for 21 days. The fracture resistance of the samples was tested using UTM (Instron, UK). The load was applied on the center of the buccal cusp slope at an angle of 30° to the long axis of the tooth with a steel ball of diameter 3.5 mm and a crosshead speed of 0.5 mm per minute [Table/Fig-5]. The applied force was measured in Newtons (N).
All the fractured specimens were observed under stereomicroscope (2X magnification) to visualize the fracture lines in the tooth and the restoration [Table/Fig-6].
Representative images of the observed failure modes in four groups: a) Type I failure pattern; b) Type II failure pattern; c) Type V failure pattern.

Failure patterns were evaluated and classified into five categories [8].
Type I - No visible fracture in the restoration and tooth;
Type II - No visible fracture in the restoration but fracture in the tooth;
Type III - Fracture in the restoration only;
Type IV - Fracture in the restoration and the tooth above CEJ; Type V - Fracture in the restoration and the tooth below CEJ.
Statistical Analysis
Fracture resistance of the samples was analysed using parametric one way ANOVA test, unpaired t-test and Tukey test. Evaluation of failure patterns was performed using non parametric Chi-square test. The analysis was done using Statistical Package for Social Sciences (SPSS), version #16. The level of significance was considered when p-value was <0.01 and <0.05.
Results
The mean fracture resistance of the experimental groups and their standard deviation are shown in [Table/Fig-7]. Highest fracture resistance was presented in Group IV (Complete Onlay) and it showed statistical significant difference (p<0.01) [Table/Fig-8, 9]. Group I (Sound teeth) showed significantly higher values than Group II (MOD Inlay) and Group III (Partial Onlay). However, there is no statistical significant difference between Groups I, II and III [Table/Fig-10]. According to the failure pattern shown in [Table/Fig-11], Group II (MOD Inlay) and Group III (Partial Onlay) presented mixed type of failures. Group IV (Complete Onlay) demonstrated 70% Type I failure.
Mean fracture resistance and Standard Deviations (SD) of different groups using one way ANOVA test.
| Groups | Mean | SD |
|---|
| Group I- Sound teeth | 997.8401 | 115.73 |
| Group II- MOD Inlay | 879.6334 | 158.92 |
| Group III- Partial Onlay | 929.9543 | 158.14 |
| Group IV-Complete Onlay | 1843.663 | 306.20 |
Comparison between the experimental groups using Tukey test.
| Groups | SE | p-value | Inference |
|---|
| Group II (MOD Inlay) | Group III- (Partial Onlay) | 50.25 | 0.865 | Not significant |
| Group IV (Complete Onlay) | 96.82 | <0.01 | Significant |
| Group III (Partial Onlay) | Group IV (Complete Onlay) | 96.82 | <0.01 | Significant |
Comparison of Group I (Control)-Sound teeth with Group IV-Complete Onlay using unpaired t-test.
| Groups | SE | t value | p-value | Inference |
|---|
| Group I (Control) Sound teeth | 36.6 | 8.171 | <0.01 | Significant |
| Group IV- Complete Onlay | 96.83 |
Comparison of Group I-Sound teeth (control) with Group II-MOD Inlay and Group III- (Partial Onlay) using unpaired t-test.
| Groups | | SE | t value | p-value | Inference |
|---|
| Group I- (Control) Sound teeth | Group II- (MOD Inlay) | 50.25 | 1.901 | 0.073 | Not significant |
| Group III- (Partial Onlay) | 36.59 | 1.095 | 0.288 | Not significant |
Frequency table of failure patterns observed in all group using Chi-square test.
| Types | Group II MOD Inlay (%) | Group III Partial Onlay (%) | Group IV Complete Onlay (%) | Chi-square value | p-value |
|---|
| Type - I | 3 (30) | 4 (40) | 7 (70) | 4.766 | <0.05 |
| Type - II | 3 (30) | 1 (10) | 0 |
| Type - III | 0 | 0 | 0 |
| Type - IV | 0 | 0 | 0 |
| Type - V | 4 (40) | 5 (50) | 3 (30) |
Discussion
The fracture resistance of human maxillary premolar with different MOD cavity design was assessed in the present study. Premolar teeth are an interesting option because these teeth have been reported to show a high incidence of fractures in the clinical situation. Fracture of buccal cusps of premolars occur more often compared to palatal cusps which was supported by Cavel WT et al., who reported that high percentage of fractures upto 60% occurred on the non functional buccal cusp while 40% fractures on the functional palatal cusp [9]. The fracture load was applied on the buccal cusp in order to simulate extreme eccentric forces [10].
In the present study, the cavities were more conservative considering the high fracture toughness and superior properties of zirconia. The occusal cavity width was maintained at 1/3rd the intercuspal distance and occlusal depth of 1.5 mm from the central groove. Palatal cusp was reduced by 1.5 mm in both Partial Onlay and Complete Onlay groups and buccal cusp by 1 mm. The gingival seat was located 1 mm above the CEJ as the margins placed below CEJ affected the stability of the restorations and also bonding.
The Sound teeth presented mean fracture resistance of 997.84 N, similar to values found in other studies, which ranged between 882 N and 1568 N [11]. Statistically there was no significant difference in the fracture resistance of Sound teeth and Inlay (Group II). This might be attributed to the minimal cavity preparation in the present study. Ragauska A et al., concluded that ceramic inlays prepared with 1/2 or 1/3rd of the intercuspal distance can recover tooth strength near to that of intact teeth [12]. According to Cubas GB et al., inlay restorations required less invasive preparation and should be preferred as they are more conservative since there is no occlusal reduction and they present fracture resistance similar to sound teeth [2].
Cuspal coverage is commonly recommended to protect the weakened cusp and to enhance the fracture resistance. In the present study palatal cusp coverage i.e., Partial Onlay (Group II) restored the fracture resistance of premolar to that of Sound teeth. These results are in accordance with a study conducted by Kantardzic I et al., who concluded that palatal cusp reduction is preferred for ideal stress distribution than inlay and complete onlay [5]. On the contrary, Cubas GB et al., suggested that partial and complete onlays with cuspal coverage has no influence on improving the fracture resistance of premolars [2]. There was no significant difference in fracture resistance values between Inlay (Group II) and Partial Onlay (Group III). It might be because of adhesively bonded zirconia restoration in both the groups which had increased the fracture resistance similar to that of Sound teeth.
Complete onlays with both the buccal and palatal cusps involved had showed a mean fracture resistance of 1843.6 N, highest of all the groups. The main reason may be related to the transformation toughening phenomenon of zirconia which requires a higher load to fracture the material and minimal onlay preparation with both cusps involved so that there is equal stress distribution in the cavity which resulted in highest fracture resistance compared to inlay, partial onlay and sound teeth. These findings were supported by Mynampati P et al., where RCT treated premolars restored with monolithic zirconia complete onlays showed a very high fracture resistance (1524.4 N) compared to sound teeth (980 N) [8]. This proves the reinforcement capability of monolithic zirconia complete onlays. Salies SG et al., reported that the fracture resistance of teeth restored with MOD Type III gold inlays with cuspal coverage is enhanced to a level much greater than the sound teeth i.e., the absorption energy of sound teeth was 7.58 kg.cm and sound teeth with gold onlay was 21.41 kg.cm. Similarly the same can be applied to the present study as the reinforcement of the tooth by zirconia complete onlays was much higher than the sound teeth [13].
In the present study, none of the samples in the experimental groups showed Type III failure (Fracture restricted to the restoration alone) i.e., cohesive failure alone in zirconia restorations. This might be attributed to sub critical crack growth and transformation toughening properties of zirconia [14]. The results obtained in the study are contradictory to the values obtained by Soares SJ et al., where the failure mode analysis revealed that fractures of the ceramic restoration occurred before the tooth structure fractured where they used IPS Empress (Leucite reinforced glass ceramic) [15].
According to the outcome of the present study, Type V mode of failure i.e., 40% and 50% was observed in Inlay and Partial Onlay groups respectively. One possible explanation is the non homogeneous stress distribution in the tooth because of the cusps involvement resulting in predominance of catastrophic failure. The findings were supported by Jiang W et al., who reported that ceramic inlay restorations result in higher stress levels in the internal surfaces of the preparation [16]. These results are in accordance with those of the current study where Onlay restored tooth (Group IV) presented 30% of Type V failures and 70% of Type I failures. The occurrence of Type I failure pattern might be because of bond failure in the cementation (adhesive) or the fracture in the internal surface of tooth, where more amount of stresses are concentrated, which had occurred before any visible cracks observed in the restoration or external surface of the tooth. However, none of the onlays got debonded. These findings are similar to the study done by Mynampati P et al., where they found 90% Type I failure and 10% Type V failure in premolars restored with zirconia onlays [8].
Limitation
The study consists of smaller sample size and the marginal fit of the restorations was not considered. Future studies with larger sample size can be undertaken to evaluate different aesthetic materials with different cavity designs.
Conclusion
Although the MOD inlays and partial onlays almost reinforced the tooth structure to that of sound teeth, complete onlays showed maximum reinforcement of the tooth structure. Hence monolithic zirconia can be chosen as the ideal material to complete onlays because of the reinforcing effect on the tooth. With the overall improvement in the aesthetics of zirconia, it could probably be the best alternative to all metal and all ceramic onlays in aesthetic areas.
[1]. Reeh ES, Messer HH, Douglas WH, Reduction in tooth stiffness as a result of endodontic and restorative proceduresJ Endod 1989 15:512-16. [Google Scholar]
[2]. Cubas GB, Habekost L, Camacho GB, Pereira-Cenci T, Fracture resistance of premolars restored with inlay and onlay ceramic restorations and luted with different agentsJ Prosthodont Res 2011 55:53-59. [Google Scholar]
[3]. Casselli DS, e Silva AL, Casselli H, Martins LR, Effect of cavity preparation design on the fracture resistance of directly and indirectly restored premolarsBraz J Oral Sci 2008 27:1636-40. [Google Scholar]
[4]. Yamada Y, Tsubota Y, Fukushima S, Effect of restoration method on fracture resistance of endodontically treated maxillary premolarsInt J Prosthodont 2004 17:94-98. [Google Scholar]
[5]. Kantardzic I, Vasiljevic D, Blazic L, Luzanin O, Influence of cavity design preparation on stress values in maxillary premolars: A finite element analysisCroat Med J 2012 53:568-76. [Google Scholar]
[6]. Piconi C, Maccauro G, Zirconia as a ceramic biomaterialBiomaterial 1999 20:01-25. [Google Scholar]
[7]. Manicone PF, Rossi Iommetti P, Raffaelli L, An overview of zirconia ceramics: Basic properties and clinical applicationsJ Dent 2007 35:819-26. [Google Scholar]
[8]. Mynampati P, Babu MR, Saraswathi DD, Kumar JR, Gudugunta L, Gaddam D, Comparision of fracture resistance and failure pattern of endodontically treated premolars with different esthetic onlay systems: An in vitro studyJ Conserv Dent 2015 18:140-43. [Google Scholar]
[9]. Cavel WT, Kelsey WP, Blankenau RJ, An in vivo study of cuspal fractureJ Prosthet Dent 1985 53:03-41. [Google Scholar]
[10]. Bitter K, Meyer-Lueckel H, Fotiadis N, Blunck U, Neumann K, Kielbassa AM, Inflluence of endodontic treatment, post insertion, and ceramic restoration on the fracture resistance of maxillary premolarsInt Endod J 2010 43:469-77. [Google Scholar]
[11]. Soares PV, Santos-Filho PC, Martins LR, Soares CJ, Influence of restorative technique on biomechanical behaviour of endodontically treated maxillary premolars. Part I: Fracture resistance an failure patternsJ Prosthet Dent 2008 99:30-37. [Google Scholar]
[12]. Ragauska A, Apse P, Kasjanovs V, Berzina-Cimdina L, Influence of ceramic inlays and composite fillings on fracture resistance of premolars in vitroStomatologija 2008 10:121-26. [Google Scholar]
[13]. Salis SG, Hood JA, Kirk EE, Stokes AN, Impact-fracture energy of human premolar teethJ Prosthet Dent 1987 58:43-48. [Google Scholar]
[14]. Vagkopoulou T, Koutayas SO, Koidis P, Strub JR, Zirconia in dentistry: Part 1-Discovering the nature of an upcoming bioceramicEur J Aesthet Dent 2009 4(2):130-51. [Google Scholar]
[15]. Soares CJ, Martins LR, Fonseca RB, Correr-Sobrinho L, Fernandes Neto AJ, Influence of cavity preparation design on fracture resistance of posterior Leucite reinforced ceramic restorationsJ Prosthet Dent 2006 95:421-29. [Google Scholar]
[16]. Jiang W, Bo H, Yongchun G, Long Xing N, Stress distribution in molars restored with inlays or onlays with or without endodontic treatment: A three dimensional finite element analysisJ Prosthet Dent 2010 103:06-12. [Google Scholar]