Introduction
Tracheostomy is commonly used to secure the airway during the immediate postoperative period in maxillofacial oncological operations. We conducted a study to review the utility of elective tracheostomy in head and neck surgery.
Aim
To review the incidence of intraoperative, perioperative and postoperative complications and its management in elective tracheostomy and to analyse its utility in head and neck surgery.
Materials and Methods
The study included review of 50 patients, who were treated for head and neck cancers in the Department of Oral And Maxillofacial Surgery of our centre between January 2011 to December 2014.
Results
The study showed a male predilection with mean tracheostomy time of 25 minutes and operative time of 11 hours. The patients had an ICU stay of two days and elective ventilation of one day with mild tracheal secretion seen postoperatively. No other complications were noted intraoperatively or postoperatively.
Conclusion
Elective tracheostomy even though an invasive tool when used properly in selected patients, can be safe and beneficial to the patients.
Introduction
One of the major challenges in the management of patients with complex oral maxillofacial procedures is in the maintenance of airway. In patients with oral cancer and faciomaxillary trauma many factors influence the management of airway due to the basic disease, proximity to airway and also the surgical procedures involved. Managing the airways in an ideal way would determine the outcomes and hence, the recovery of the patient.
There are many studies in the literature comparing the outcomes of elective and emergency tracheostomies. Moreover, there are also comparisons between surgical and percutaneous methods of performing tracheostomy in these clinical situations [1]. We reviewed our subset of patients who underwent major surgical resections and reconstructions for head and neck oncology with elective tracheostomy and assessed various parameters in them.
There is a lot of controversy in the management of airway during the immediate postoperative period in maxillofacial oncological operations despite tracheostomy being used commonly [2,3].
Tracheostomy was recommended by the American Academy of Otolaryngology to be one of the effective methods to manage the airway in major head and neck surgeries. However, the recommendation was vague [4]. In 2009 Marsh M et al., in their study found that 39% of units would “almost always” and 30% would “usually” do an elective tracheostomy for an uncomplicated free flap surgery from data involving 57 centres. Twenty eight percent of patients in this study were “almost always” ventilated postoperatively and 26% of patients were “usually” ventilated. This study also concluded that only 7% of patients were almost always managed with elective overnight intubation, postoperatively [5].
Tracheostomy is however associated with appreciable morbidity, with reported complication rates of 8–45% [3,6-8]. The complications include bleeding, injury to adjacent structures, surgical emphysema, pneumothorax, or pneumomediastinum, blockage of the tracheostomy cannula, displacement of the cannula, tracheitis, cellulitis, pulmonary atelectasis, tracheoinnominate fistula, trachea-oesophageal fistula, tracheocutaneous fistula, tracheomalacia, granulation, excessive scarring, and failure to decannulate.
Halfpenny W and McGurk M, in their case report, reported a displaced tracheostomy tube which was inadvertently replaced outside the trachea which resulted in cardiorespiratory arrest [6].
However, for complex maxillofacial trauma cases most of the clinicians have been practicing alternatives to tracheostomy such as submental intubation. In head and neck oncology cases, there is very less literature evidence for alternatives to tracheostomy [9].
It was also noted that pulmonary complications were more in patients undergoing major head and neck surgery with tracheostomy as shown by Morton RP et al., and Ong SK et al., who reported a rate of 45% and 72% respectively despite being on antibiotics [10,11]. Many other studies, including by Rao MK et al., have also reported pulmonary complications were more in the presence of tracheostomy [12].
The aim of the present study was to retrospectively review the incidence of intraoperative, perioperative and postoperative complications and its management in elective tracheostomy in patients undergoing surgery for head and neck oncology and its utility in these patients.
Materials and Methods
This was a retrospective study wherein the records of the patients who were admitted with head and neck cancer in the past four years were reviewed. The study included 50 patients [male 48: female 2], who were treated for head and neck cancers in the Department of Oral and Maxillofacial Surgery of SDM Craniofacial Unit, Dharwad, Karnataka, India between 2011 to 2014. All patients who underwent elective tracheostomy and who had a major intraoral resection, a unilateral or bilateral neck dissection, and reconstruction with free flaps were included in the study. Patients whose records were not available, patients who didn’t consent for inclusion and patients who were lost to follow up were excluded. Ethical clearance was obtained from the college ethical committee and proper consent was taken.
Procedure of tracheostomy performed in our unit: Once the patient was fit for surgery, we performed elective tracheostomy prior to the surgery either under general anaesthesia or under local anaesthesia with or without sedation after obtaining written and informed consent of the patient. All the patients received antibiotic prophylaxis half an hour before the procedure. Anaesthesiologists monitored the vital signs.
The tracheostomy procedure was performed by a surgeon under all aseptic precautions usually under local anaesthesia with intravenous sedation or general anaesthesia with the help of an anaesthesiologist.
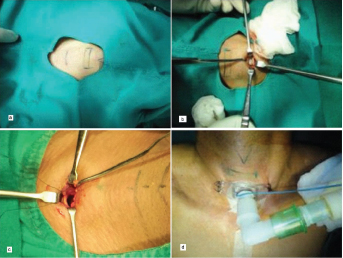
Patient was positioned in supine position with full extension of the head and neck by placing a shoulder pad under the patient’s shoulders. Neck and head was positioned in the midline which would bring the cervical trachea forward in the neck and more tracheal rings were accessible in the neck. After preparing and draping the area, a horizontal neck incision midway between the second and third tracheal rings was made using surgical blade as shown [Table/Fig-1a].
a) Showing the incision markings for elective tracheostomy; b) The pretracheal fascia is incised and the tracheal rings were exposed; c) Bjork flap was marked and taken on the anterior wall of trachea; d) Tracheostomy tube fixed in place.
Further the incision was deepened in midline cutting both the layers of cervical fascia (superficial and deep layers) including subcutaneous fat.
Dissection was carried out with a curved haemostat, strictly in the midline. The midline raphe present between two sets of strap muscles on either side of neck was dissected. Retractors were used to retract the strap muscles on either side. The thyroid isthmus was now exposed and retracted upwards to expose the 2nd and 3rd tracheal rings. The pretracheal fascia was incised and the tracheal rings were exposed as shown [Table/Fig-1b]. Next a syringe loaded with local anaesthesia was inserted into the trachea and aspirated and checked for air bubbles, taking care not to pierce the posterior wall of trachea. Lignocaine was instilled into tracheal lumen to anaethetise the mucosa and prevent vasovagal attack. A Bjork flap was marked and taken on the anterior wall of trachea as shown in figure [Table/Fig-1c].
The opening made in the trachea was further dilated with a tracheal dilator following which tracheostomy tube was inserted with the help of an obturator or guide. After removal of these, the position of the tube was confirmed by airblast and auscultation of chest bilaterally. Tracheostomy tube was fixed in place with 3-0 silk to the skin of the neck. The cuffed portex tube was inflated. The dressing was done as shown in figure [Table/Fig-1d].
After, the procedure patient was shifted to ICU with a tracheostomy kit always kept by the bedside of the patient. Proper care of the tracheostomy and airway was taken. Suction through the tube was done every two hours with instillation of diluted sodium bicarbonate before suctioning.
A sterile catheter of 1/3rd diameter of tracheostomy tube was used with sterile gloves for suctioning everytime. The size of the catheter tube must be 1/3rd the inner diameter of tracheostomy tube.
100% oxygen was given before and after suction.
Over the opening of the tracheostomy tube, single moist gauze was placed at all times to help in humidification of air entering the lower respiratory tract.
Tracheostomy dressing was changed every day.
Chest physiotherapy and nebulization with bronchodilator was done two to three times.
Results
The following variables were recorded: age and sex, American Society of Anaesthesiologists (ASA) grade, smoking/tobacco chewing, site of tumour, type of neck dissection, use of mandibulotomy/mandibulectomy, type of reconstruction, duration of stay in ICU, and total hospital stay. Any postoperative complications associated with the airway were also recorded.
Fifty patients were included in this study, among them 48 were males and two females showing a male gender predilection and their details are given in the table [Table/Fig-2]. The mean hospital stay was 21 days with mean tracheostomy time of 25 minutes while the mean operating time was found to be 11 hours. The patients had an ICU stay of two days with elective ventilation of one day and mild tracheal secretions were seen postoperatively. The buccal mucosa was the most common sites of the tumour 32 out of 50 followed by mandible/alveolous and anterior tongue as given in table [Table/Fig-3]. In 46 cases, unilateral neck dissection was done and in four bilateral neck dissection, other operative procedures were mandiblectomy, mandibulotomy and maxillectomy which were done in 36, 12 and two cases respectively. Radial forearm flap was the most common used flaps followed by Anterolateral Thigh (ALT) flap, free fibula and Pectoralis Major Myocutaneous (PMMC) flap. Details of operative procedures and type of reconstruction are given in table [Table/Fig-4].
Aetiology and ASA Grading.
| Mean age (years) | Sex | ASA Grading | Tobacco Chewing | Postoperative Surgical Complications |
|---|
| 40 years (32-60 years) | 48:02 (male:female) | I | 42 | Yes | 50 | 1 (haematoma on the first postoperative day) |
| II | 08 | No | 00 |
| III | 00 | | |
| Anterior tongue/lateral tongue | 06(50) |
| Floor of mouth | 01(50) |
| Mandible/alveolus | 08(50) |
| Buccal mucosa | 32(50) |
| Palate | 02(50) |
| Retromolar trigone | 01(50) |
Types of operation and reconstruction.
| Neck dissection |
| Unilateral | 46 |
| Bilateral | 04 |
| Mandibulectomy | 36 |
| Mandibulotomy | 12 |
| Maxillectomy | 02 |
| Types of reconstruction |
| Radial forearm flap | 22 |
| ALT flap | 12 |
| Free fibula | 10 |
| PMMC flap | 06 |
ALT = anterolateral thigh flap
PMMC = pectoralis major myocutaneous
We reported one case of surgical complication, where re-exploration of the surgical site had to be done due to haematoma on the first postoperative day. This was the only major complication noted due to tracheostomy [Table/Fig-1].
Discussion
Patients suffering from head and neck cancer usually have significant comorbid conditions. Surgery being the mainstay of treatment in these patients, they are prone for postoperative complications due to prolonged surgery and also comorbid conditions, hence most of the patients would need intensive care postoperatively. Airway management is crucial for any surgery and especially for patients undergoing maxillofacial oncological operations [13]. Head and neck oncological surgical procedures are major surgical exercises wherein airway and support of ventilation is an important component in the appropriate management of immediate postoperative period. Therefore, recently, overnight ventilation with an endotracheal tube has been introduced for cases in which challenging airway maintenance is predicted such as in postoperative oedema [8,9,13,14]. However, this technique is not optimal because the endotracheal tube can cause discomfort and restlessness. It is difficult to perform tracheobronchial lavage. Not all the patients will tolerate the endotracheal tube unless sedated.
Due to this it sometimes becomes difficult to determine the ideal timing for removal of the tube. Moreover, the trauma due to major surgery would lead to an increase in the oedema during the first two or three days after surgery, and extubation at this time would be inappropriate which could lead to many problems.
Once the patient is extubated reintubation can be very problematic and if fails, an emergency tracheostomy should be performed. The emergency tracheostomy in these conscious patients with head and neck oedema is highly demanding. This can lead to complications and increase the failure rate of securing airway [15].
Intubation can also pose a difficulty index for the anaesthetist to reintubate in cases of complications even in presence of fibreoptic due to anatomical changes. The incidence of re-exploration in our unit was 2% so in such cases of re-exploration due to anastomosis failure, large haematoma, internal bleed; the time taken for reinducing was much faster and easier with elective tracheostomy.
We reported one case of surgical complication, where re- exploration of the surgical site had to be done due to heamatoma on the first postoperative day. Due to the tracheostomy tube, it was advantageous to both the anaesthetist to induce general anaesthesia and for the surgeon to prevent neck oedema and to perform re-exploration with ease.
In this aspect elective tracheostomy is the most definitive technique to maintain airway in the postoperative period. As long term airway maintenance can be on the cards, an elective tracheostomy is recommended in high risk patients [16]. Even though done in a proper manner tracheostomy has a very low complication rates, but the procedure is invasive, adds to the costs and stay of the patient [17,18].
In consideration of these challenges, this study retrospectively researched the morbidity and other occurrences pertaining to elective tracheostomy.
The routine use of elective tracheostomy remains common place. Marsh M et al., in their study found that 39% units “almost always” and 30% “usually” doing a tracheostomy for a hypothetical patient with an uncomplicated free flap. The same study found that only 9% of units would “almost never” do a tracheostomy for these patients [5]. This still is in accordance with our practice wherein around 70% of the centers still carry out elective tracheostomy.
It is also important to understand that tracheostomy is always not free of complications. These complications can be life threatening and chest infections are more common in patients who have had a tracheostomy [3,10-12].
Patients who develop tracheostomy-related complications have a longer ICU stay and also have a longer total duration of hospital stay; Castling B et al., found that patients spent a mean of four days in the ICU compared to the mean ICU stay of two days in our study [3]. In this study, it was also reported that the mean hospital stay of patients with tracheostomy related complication was 25 days compared to the mean stay of 14 days for patients without complications.
The mean duration of hospital stay for our patients was 21 days. Fortunately, none of our patients developed any pulmonary complications.
One potential argument for the continued use of elective tracheostomy is that patient can be cared for in a ward, which means there is no need for a bed in ICU. It was established in the past that it was acceptable to resect cancers of the head and neck without transferring patients to the ICU immediately postoperatively [19,20].
Contrary to this Marsh M et al., noted that 54% of patients in the total 57 units who underwent major intraoral resection and reconstruction with a free flap required ICU care while 33% of patients would return to High Dependency Unit (HDU) [5].
All of our patients had an ICU stay of two days (range). Decannulation was carried out on third postoperative day. One could also state that tracheostomy also offers improved patient comfort, promotion of better nutrition, decreased risk of laryngeal damage, easier tracheobronchial toilet, reduction in anatomic dead space by 50% [2,3].
Limitation
The data for this study was collected retrospectively and there was no control group, which could be regarded as a limitation, but the quality of note keeping was high and the information required was available in the notes.
A future study that prospectively compares the outcomes from units who routinely do tracheostomies with those who do not, could generate more data and greater numbers, and would also allow a direct comparison of outcomes between the two groups.
Conclusion
We should constantly question our practice and examine the necessity for performing any procedure. The over-riding consideration above all others must be that we do what is best and least damaging for the patient. There should be a clear benefit for any procedure performed and it should be the least invasive option available. Conventional open tracheostomy is associated with a low complication rate, is safe, efficient in maintaining the airways in complex maxillofacial surgeries. In our procedure there was no loss of airway control for greater than 20 sec, no airway obstruction, no blood loss exceeding 30 ml and no aspiration, perioperative mortality and postoperative complications. We conclude that elective tracheostomy even though an invasive tool when used properly in selected patients can be safe and beneficial to the patients.
ALT = anterolateral thigh flapPMMC = pectoralis major myocutaneous
[1]. Gysin C, Dulguerov P, Guyot JP, Perneger TV, Abajo B, Chevrolet JC, Percutaneous versus surgical tracheostomyAnn Surg 1999 230(5):708 [Google Scholar]
[2]. Crosher R, Baldie C, Mitchell R, Selective use of tracheostomy in surgery for head and neck cancer: An auditBr J Oral Maxillofac Surg 1997 35:43-45. [Google Scholar]
[3]. Castling B, Telfer M, Avery BS, Complications of tracheostomy in major head and neck cancer surgery: A retrospective study of 60 consecutive casesBr J Oral Maxillofac Surg 1994 32:3-5. [Google Scholar]
[4]. Archer SM, Baugh RF, Nelms CR, 2000 Clinical Indicators Compendium 45 2000 Alexandria, VAAmerican Academy of Otolaryngology-Head and Neck Surgery [Google Scholar]
[5]. Marsh M, Elliott S, Anand R, Brennan PA, Early postoperative care for free flap head and neck reconstructive surgery - a national survey of practiceBr J Oral Maxillofac Surg 2009 47:182-85. [Google Scholar]
[6]. Halfpenny W, McGurk M, Analysis of tracheostomy-associated morbidity after operations for head and neck cancerBr J Oral Maxillofac Surg 2000 38:509-12. [Google Scholar]
[7]. Waldron J, Padgham ND, Hurley SE, Complications of emergency and elective tracheostomy: A retrospective study of 150 consecutive casesAnn R Coll Surg Engl 1990 72:218-20. [Google Scholar]
[8]. Taicher S, Givol N, Peleg M, Ardekian L, Changing indications for tracheostomy in maxillofacial traumaJ Oral Maxillofac Surg 1996 54:292-96. [Google Scholar]
[9]. Scutz P, Hamed H, Submental intubation versus tracheostomy in maxillofacial trauma patientsJ Oral Maxillofac Surg 2008 66:1404-09. [Google Scholar]
[10]. Morton RP, Mellow CG, Dorman EB, Chest infection following head and neck surgery: A pilot studyClin Otolaryngol Allied Sci 1990 15:363-66. [Google Scholar]
[11]. Ong SK, Morton RP, Kolbe J, Whitlock RM, McIvor NP, Pulmonary complications following major head and neck surgery with tracheostomy: A prospective randomised, controlled trial of prophylactic antibioticsArch Otolaryngol Head Neck Surg 2004 130:1084-87. [Google Scholar]
[12]. Rao MK, Reilley TE, Schuller DE, Young DC, Analysis of risk factors for postoperative pulmonary complications in head and neck surgeryLaryngoscope 1992 102:45-47. [Google Scholar]
[13]. Mishra S, Bhatnagar S, Jha RR, Singhal AK, Airway management of patients undergoing oral cancer surgery: A retrospective studyEur J Anaesthesiol 2005 22:510-14. [Google Scholar]
[14]. Coyle MJ, Shrimpton A, Perkins C, Fasanmade A, Godden D, First do no harm: Should routine tracheostomy after oral and maxillofacial oncological operation be abandoned?Br J Oral Maxillofac Surg 2012 50:732-35. [Google Scholar]
[15]. Phero JC, Rosenberg MB, Giovannitti JA, JrAdult airway evaluation in oral surgeryOral Maxillofac Surg Clin North Am 2013 25:385-99. [Google Scholar]
[16]. Astrachan DI, Kirchner JC, Goodwin WJ, JrProlonged intubation vs. tracheotomy: Complications, practical and psychological considerationsLaryngoscope 1988 98:1165-69. [Google Scholar]
[17]. Chew JY, Cantrell RW, Tracheostomy: Complications and their managementArch Otolaryngol 1972 96:538-45. [Google Scholar]
[18]. Kenan PD, Complications associated with tracheostomy: Prevention and treatmentOtolaryngol Clin North Am 1979 12:807-16. [Google Scholar]
[19]. Godden DR, Patel M, Baldwin A, Woodwards RT, Need for intensive care after operations for head and neck cancer surgeryBr J Oral Maxillofac Surg 1999 37:502-05. [Google Scholar]
[20]. McVeigh KP, Moore R, James G, Hall T, Barnard N, Advantages of not using the intensive care unit operations for oropharyngeal cancer: An audit at Worcester Royal HospitalBr J Oral Maxillofac Surg 2007 45:648-51. [Google Scholar]