A Prospective Study of Different Methods of Inferior Turbinate Reduction
Santosh Uttarkar Panduranga Rao1, Prashanth Basavaraj2, Supriya Basavaraj Yempalle3, Aravind Darga Ramachandra4
1 Professor, Department of Ear, Nose and Throat, J.J.M. Medical College, Davangere, Karnataka, India.
2 Professor, Department of Ear, Nose and Throat, J.J.M. Medical College, Davangere, Karnataka, India.
3 Post Graduate, Department of Ear, Nose and Throat, J.J.M. Medical College, Davangere, Karnataka, India.
4 Post Graduate, Department of Ear, Nose and Throat, J.J.M. Medical College, Davangere, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Santosh Uttarkar Panduranga Rao, No.4123, ’Saavan’ 14th Cross, Anjaneya Layout, Davangere-577004, Karnataka, India.
E-mail: drsantoshup@gmail.com
Introduction
All the functions of nasal cavities are performed through mucosa and contours of the turbinates. Hypertrophied inferior turbinate is one of the major and common causes of nasal obstruction. In these patients nasal obstruction is relieved by inferior turbinate reduction. Many procedures on turbinate reduction have been described earlier.
Aim
To compare and evaluate the better method for inferior turbinate reduction among submucosal diathermy using monopolar cautery and bipolar cautery, complete turbinectomy, inj. sodium tetradecylsulphate infiltration.
Materials and Methods
Eighty patients of either sex between 17-50 years of age having inferior turbinate hypertrophy were included in the study. The patients were divided into four groups with 20 patients in each group. Each group had 20 patients. Group A was subjected to submucosal diathermy using monopolar cautery, Group B to bipolar cautery, Group C to complete inferior turbinectomy and group D to injection sodium tetradecylsulphate. Patients were assessed for nasal patency and symptomatic relief, postoperative bleeding, pain, crusting and synachiae. Follow up was done on 7th day, 21st day and 3rd month postoperatively. Statistical analysis was carried out using IBM SPSS Version 20.0 for windows. Mean and standard deviations were calculated for quantitative data, for categorical variables frequencies and percentages were calculated, within the group comparisons were done with paired t-tests.
Results
The mean reduction in postoperative nasal obstruction was found to be maximum with bipolar cautery when compared with the other modalities and this difference was found to be statistically significant (p<0.001). Bipolar cautery was found to be associated with minimum after effects when compared to other modalities except for postoperative pain which was found more in the patients operated by the bipolar cautery method.
Conclusion
We found inferior turbinate reduction using bipolar cautery was better and safe method, when compared to monopolar cautery, complete turbinectomy and inj. sodium tetradecylsulphate, however further studies are required with larger sample size.
Bipolar cautery, Complete turbinectomy, Inferior turbinate hypertrophy, Sodium tetradecyl sulphate, Monopolar cautery
Introduction
Nasal airflow disturbance occur in about 30% of the population causing nasal obstruction and most common cause being hypertrophied inferior turbinate [1]. Nasal obstruction is a result of submucosal or mucosal hypertrophy due to increased vascularity as the anterior end of the inferior turbinate is an erectile tissue [2].
Usually hypertrophied inferior turbinates are treated with drugs like antihistamines, local decongestants, steroids [3]. When conservative management is not able to relieve the nasal obstruction completely, surgical treatment is indicated.
At least 13 surgical techniques have been used over the past 130 years to treat hypertrophy of the inferior turbinate [4] these include simple turbinate out fracture; turbinoplasty techniques such as extramucosal destruction, and submucosal tissue removal, electrocautery, chemical cautery and extramural turbinate resection (partial or complete), radiofrequency, laser and many more. The purpose of surgically reducing inferior turbinate should be to relieve nasal obstruction and maintain a good nasal health.
The tertiary care centre recommends either laser or radiofrequency ablation [2]. The district level ENT practitioners perform simple and conventional procedures like complete turbinectomy, sclerosing agents, electrocautery and chemical cautery due to lack of availability of modern equipments. Each conventional method has its advantages and drawbacks. The aim of our study was to analyze and compare the outcome and better method of inferior turbinate reduction among submucosal diathermy using monopolar cautery and bipolar cautery, complete turbinectomy, inj. sodium tetradecylsulphate infiltration.
Materials and Methods
This was a prospective interventional and comparative study conducted between September 2014 to September 2015, in the Department of Otorhinolaryngology and Head and Neck Surgery, Chigateri General Hospital and Bapuji Hospital a teaching hospital attached to Jagadguru Jayadeva Murugarajendra Medical College, Davangere, Karnataka, India. A total of 80 patients were enrolled in this study, after taking an informed consent and acquiring the ethical committee clearance.
A total of 52 males and 28 females between 17-50 years of age with complaints of nasal obstruction who had mucosal type of inferior turbinate hypertrophy were selected and divided into four groups. Each group consist of 20 patients. Patient with only bilateral hypertrophied inferior turbinate and no other associated pathology were included in study. Patients with previous history of nasal surgery, deviated nasal septum and sinusitis were excluded. All patients were examined clinically for ENT and preoperative evaluation was done with routine profile and CT scan paranasal sinus. The inferior turbinates were evaluated by anterior rhinoscopy and nasal endoscopy before and after the application of topical decongestants. The size of the inferior turbinates were graded as follows: Grade 0 – no turbinates, grade 1 - the inferior turbinates occupying <25% of nasal cavity, grade 2 - the inferior turbinate occupying 25%-50% of nasal cavity, grade 3 - the inferior turbinate occupying 50%-75% of the cavity, grade 4- the inferior turbinate occupying almost the nasal cavity and touching nasal septum.
First set of 20 patients was included in Group A and underwent submucosal diathermy using monopolar cautery, subsequent 20 patients were put in Group B and they underwent bipolar cautery then next 20 patients were put in Group C who underwent complete turbinectomy and last 20 patients were put in Group D who were subjected to inj. sodium tetradecylsulphate infiltration. Patients were assessed with regard to symptomatic relief, postoperative synachiae formation, bleeding, pain and crusting. Follow up was done on 7th day, 21st day and 3rd month postoperatively.
Statistical Analysis
Statistical analysis was carried out using IBM SPSS Version 20 for windows. Mean and standard deviations were calculated for quantitative data, for categorical variables frequencies and percentages were calculated, within the group comparisons were done with paired t-tests.
Procedure
All procedures were performed under general anaesthesia.
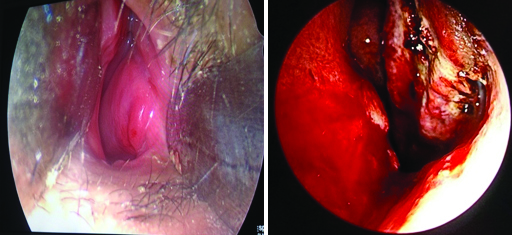
Monopolar cautery (Group A): Inert electrode was placed under right thigh. A 7.5 cm 22 gauge spinal needle was used as monopolar probe and inserted longitudinally into the anterior end of inferior turbinate inferior surface. The cautery was operated with foot switch control till the anterior end of turbinate blanches avoiding charring. Similar procedure was repeated on medial and superior surface then posterior part of the turbinate with precaution not to injure septum and ala [Table/Fig-1].
Group A: a) Pre-cauterisation; b) Post cauterization.
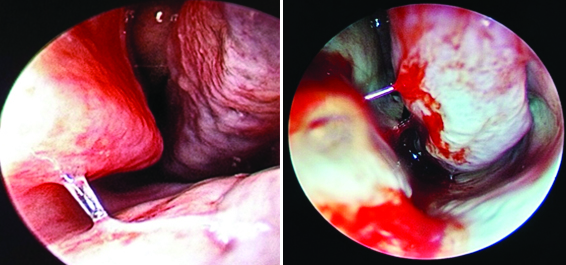
Bipolar cautery (Group B): Bipolar cautery forceps is introduced into the nasal cavity touching both the superior and inferior surface of the turbinate. The forcep is inserted till the bone is felt. Bipolar cautery was controlled with foot switch [Table/Fig-2].
Group B: a) Pre cauterisation; b) Post cauterisation.
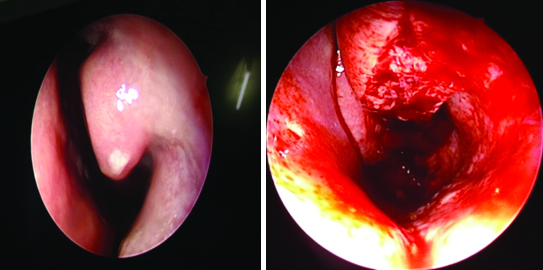
Complete turbinectomy (Group C): Conventional method of complete turbinectomy followed using turbinectomy scissors [Table/Fig-3].
Group C- (a) Pre turbinectomy (b) Post turbinectomy.
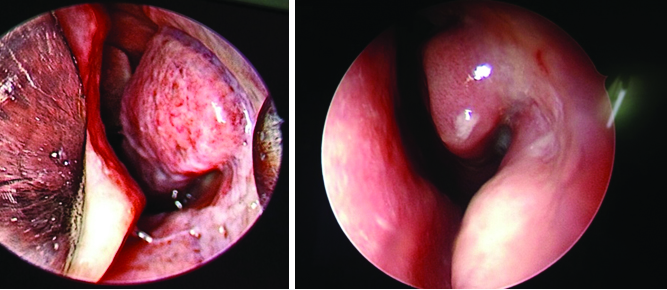
Inj. Sodium tetradecylsulphate (Group D): Inj. sodium tetradecylsulphate was diluted with normal saline in ratio of 1:1 that is 1 ml of sodium tetradecylsulphate added to 1 ml of normal saline. Each inferior turbinate was then infiltered with 1 ml of the dilution [Table/Fig-4].
Group D-(a) Pre infiltration (b) Post infiltration.
After the procedure nasal cavity was packed using vaseline gauze. All the surgeries were performed by same surgeon to maintain the uniformity. Nasal pack was removed after 24 hours followed by examination. Follow up was done on the seventh and 21st day, and after third month.
Results
Our study included 52 (65%) males and 28 (35%) females. The mean age of the patient was reported to be 33.5 years. The main symptom prior to surgery was 100% nasal obstruction in patients. On follow up the mean reduction in postoperative nasal obstruction [Table/Fig-5] was found to be 66.5±13.96 in first week and 63.0±16.25 on third month using unipolar cautery; 83.0±22.96 and 78.0±23.19 on first week and third month respectively using bipolar cautery; 57.5±12.62 and 49.0±17.14 on first week and third month respectively by complete turbinectomy; 50.0±35.54 and 48.0±24.99 on first week and third month respectively by using Inj. setrol.
Mean nasal obstruction reduction at different follow up.
| Methods | Preoperative(Present) | 1st WeekMean±SD | 3rd WeekMean± SD | 3rd MonthMean± SD | 1st Week Vs. 3rdWeek | 1st Week Vs. 3rdMonth | 3rd Week Vs. 3rdMonth |
|---|
| Monopolar (N=20) | 100% | 66.5±13.96 | 60.0±15.04 | 63.0±16.25 | t=2.63, p<0.01 | t=1.03, p<0.317 | t=1.03, p,0.316 |
| Bipolar (N=20) | 100% | 83.0± 22.96 | 78.0±23.19 | 78.0±23.19 | t=1.72, p<0.101 | t=1.72, p<0.101 | |
| Complete Turbinectomy (N=20) | 100% | 57.5±12.62 | 47.5±14.55 | 49.0±17.14 | t=3.56, p<0.002 | t=3.31, p<0.004 | t=0.78, p<0.445 |
| Inj. Setrol (N=20) | 100% | 50.0±35.54 | 54.25±29.44 | 48.0±24.99 | t=1.17, p<0.254 | t=0.36, p<0.722 | t=1.52, p<0.144 |
“Paired t-test”
Postoperative complications like synechiae, postoperative pain, post-operative bleeding and crusting was more in complete turbinectomy than compared to other procedures, no synachiae was found in monopolar and bipolar cautery [Table/Fig-6,7].
Inferior turbinate size reduction.
| Inferior turbinate size | Monopolar(N=20) | Bipolar(N=20) | CompleteTurbinectomy(N=20) | Inj. Setrol(N=20) |
|---|
| Preoperative | Grade 0 | 0 | 0 | 0 | 0 |
| Grade 1 | 0 | 6 | 6 | 2 |
| Grade 2 | 10 | 12 | 10 | 10 |
| Grade 3 | 10 | 2 | 4 | 8 |
| Postoperative |
| 1st week | Grade 0 | 0 | 0 | 20 | 0 |
| Grade 1 | 8 | 18 | 0 | 7 |
| Grade 2 | 12 | 2 | 0 | 6 |
| Grade 3 | 0 | 0 | 0 | 7 |
| 3rd week | Grade 0 | 0 | 0 | 20 | |
| Grade 1 | 10 | 18 | 0 | 5 |
| Grade 2 | 10 | 2 | 0 | 4 |
| Grade 3 | 0 | 0 | 0 | 11 |
| 3rd month | Grade 0 | 0 | 0 | 20 | 0 |
| Grade 1 | 8 | 18 | 0 | 5 |
| Grade 2 | 12 | 2 | 0 | 4 |
| Grade 3 | 0 | 0 | 0 | 11 |
Postoperative complications.
| Parameters | Monopolar(N=20) | Bipolar(N=20) | CompleteTurbinecto-my (N=20) | Inj. Sodium tetrade-cylsulphate (N=20) |
|---|
| Synechiae | 0 | 0 | 8(40) | 6(30) |
| Postoperative pain | 4(20) | 10(50) | 14(70) | 0 |
| Postoperative bleeding | 4(20) | 6(30) | 20(100) | 0 |
| Crusting | 4(20) | 6(30) | 20(100) | 8(40) |
Discussion
The aim of inferior turbinate reduction is to reduce the size of turbinate in order to create sufficient space for normal nasal cycle regulation [5]. Only subjective assessment was done postoperatively for nasal obstruction and complications associated procedures.
With submucosal diathermy using monopolar electrocautery and bipolar electrocautery, histological mucosal changes occur which include conversion of columnar epithelium into cuboidal epithelium as a result of burn injury.
Mohammad Hassan Al-Baldawi did a comparative study between partial turbinectomy and submucus diathermy, according to his study postoperative nasal obstruction improvement seen in 82.5% patients with submucous diathermy and 97.5% in patients with turbinectomy postoperative bleeding seen in 12.5% patients with turbinectomy and with submucosal diathermy it was negligible. Nasal crusting was seen in 5% patients with turbinectomy [6]. Imad et al., did comparative study of submucosal diathermy with partial turbinectomy and found submucosal diathermy safe and better procedure in respect to bleeding, pain, crusting and healing than partial turbinectomy and nasal permeability between two procedures at the end of one month was (SMD: PIT) 11:14 [7].
In our study mean reduction in nasal obstruction after three months was 63.0±16.25% with monopolar electrocautery, 78.0±23.19 % with bipolar electrocautery, 49.0±17.14% with complete turbinectomy and 48.0±24.99% with Inj. sodium tetradecylsulphate infiltration. Postoperative pain, crusting and synachiae formation was seen maximum complete turbinectomy patients with bleeding being the major postoperative problem and it is aggressive procedure whereas, postoperative pain and bleeding was minimal with Inj. sodium tetradecylsulphate infiltration. With monopolar electrocautery postoperative pain, bleeding and crusting seen in 20% of patients. With bipolar electrocautery reduction of nasal obstruction was significant and inferior turbinate size in 18 (90%) patients at the third month follow up was grade 1, but postoperative pain was present in 50% of patients.
Limitation
The limitation of this study is the sample size and patients were not divided as per the size of inferior turbinate.
Conclusion
Every method of inferior turbinate reduction has its own advantages and disadvantages. In our study efforts were made to compare, analyse and find out the best effective procedure keeping in view of intraoperative ease and postoperative outcome. We found that the uses of bipolar electrocautery is better, safe and effective for significant nasal obstruction reduction with major after effect being postoperative pain which can be managed effectively with conservative management. However, further studies are required with larger sample size.
“Paired t-test”
[1]. Luczaj J, Submucosal bipolar radio frequency therapy for treatment of inferior turbinate hypertrophyOtolaryngol Pol 2007 61(3):290-94. [Google Scholar]
[2]. Taneja M, Taneja MK, Intra turbinate diathermy cautery v/s high frequency in inferior turbinate hypertrophyIndian J Otolaryngol Head Neck Surg 2010 62(3):317-21. [Google Scholar]
[3]. Magarey MJ, Jayaraj SM, Saleh HA, Sandison A, Ball valve nasal obstruction following incomplete inferior turbinectomyJ Laryngol Otol 2004 118:146-47. [Google Scholar]
[4]. Hol MK, Huizing EH, Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniquesRhinology 2000 38(4):157-66. [Google Scholar]
[5]. Mlynski G, Restorative procedures in disturbed function of the upper airway- nasal breathingGMS Curr Top Otorhinolaryngol Head Neck Surg 2005 4:Doc07 [Google Scholar]
[6]. Al-Baldawi MH, Management of inferior turbinate hypertrophy: a comparative study between partial turbinectomy and submucus diathermyIraqi J Comm Med 2009 22(4):264-67. [Google Scholar]
[7]. Imad Javed, Sanaullah Comparison of submucosal diathermy with partial inferior turbinectomy: A fifty case studyJPMI 2012 26(1):91-95. [Google Scholar]