Staghorn calculi cause severe morbidity due to renal failure; infections and death [1]. Indications for open stone surgery have markedly diminished due to advances in endourological surgery and Shock Wave Lithotripsy (SWL) [2].
PNL, SWL and Retrograde Intra Renal Surgery (RIRS) have high incidence of recurrence due to infective process and incomplete removal [1]. Open stone surgery in the modern era constitutes to 1%–5.4% of the cases [2]. The indications for open stone surgery include complex staghorn stones not removable by a reasonable number of PNL attempts without SWL procedures and large staghorn calculi with comorbidities like chronic obstructive pulmonary disease [1]. Anatrophic Nephrolithotomy (AN) as proposed by Smith and Boyce in 1968 is the most preferred technique for such surgery [2]. Stone free rate of 80%-100% can be achieved as compared with SWL or PNL with preserved renal function [3]. We present our experience of AN in our centre wherein we have performed more than 2500 procedures for renal calculi.
Materials and Methods
Between April 2008 and July 2015, AN was done in 14 renal units in 13 patients at our institute which is a tertiary care referral urological center. These records were assessed and analysed for this retrospective study.
Case details of patients undergoing AN were retrieved from our institutional patient database. Demographic details including age and gender, stone characteristics such as stone size, side, location, kidney function and previous surgeries for stone were included. Operative characteristics like approach, operative duration, intraoperative complications, placement of stent, nephrostomy and drain and postoperative course were analysed. Clearance as assessed after ancillary procedures like SWL if needed was studied. Follow up for recurrence and renal failure was done at regular intervals.
Statistical Analysis
Statistical analysis was performed using SPSS version 20 for Windows (SPSS, IBM Corp., Armonk, NY, USA). Descriptive statistics was used. After assessing the normality of the data using a Box and Whisker plot, the variables were summarized using mean and standard error or median and interquartile range and percentages based on the characteristics of the variables.
Results
Over the past seven years, a total of 2,565 procedures were performed for stone disease and 1,308 (51%) were SWL. PNL was performed in 1,086 (42.3%) patients, pyelolithotomy in 148 (5.8%) patients and RIRS was done in 10 patients (0.4%). Thirteen patients underwent AN (0.5%). Open surgery was performed in 161 (6.3%) patients.
Baseline characteristics and investigations: The median (IQR) age was 58 (30) years and male:female ratio was 10:3. The mean (SD) Length of Hospitalization (LOH) was 20.67±6.21 days. The duration of symptoms was 193.33±208.99 (mean±SD) days, ranging from one month – two years. Eight patients had comorbidities diabetes mellitus in 4; Chronic Kidney Disease (CKD) in 2 and COPD in 2 patients. Most patients (12/13) presented with loin pain and one patient presented after PNL for complete clearance. The patient characteristics, operative time, in situ cold ischemia time, postoperative LOH, clearance and blood loss are shown in [Table/Fig-1].
Patient and operative characteristics.
| Patient | Age, years | Gender | OT, min | In situ cold ischemia, min | Postop LOH, d | Clearance, % | Blood loss, ml | No of blood units transfused |
|---|
| 1 | 58 | Male | 180 | 45 | 20 | 90 | 150 | 1 |
| 2 | 60 | Male | 130 | 60 | 17 | 100 | 500 | 1 |
| 3 | 25 | Male | 190 | 55 | 8 | 90 | 200 | 5 |
| 4 | 60 | Male | 210 | 50 | 10 | 90 | 100 | 0 |
| 5 | 60 | Male | 210 | 45 | 8 | 85 | 100 | 0 |
| 6 | 62 | Male | 220 | 55 | 25 | 95 | 100 | 2 |
| 7 | 45 | Female | 200 | 50 | 26 | 95 | 100 | 2 |
| 8 | 30 | Male | 195 | 50 | 16 | 95 | 150 | 2 |
| 9 | 30 | Female | 200 | 45 | 9 | 100 | 50 | 0 |
| 10 | 46 | Male | 210 | 39 | 11 | 95 | 120 | 2 |
| 11 | 17 | Male | 190 | 45 | 10 | 95 | 150 | 2 |
| 12 | 35 | Male | 210 | 44 | 9 | 100 | 200 | 2 |
| 13 | 43 | Male | 200 | 45 | 8 | 100 | 150 | 1 |
| 14 | 25 | Female | 190 | 39 | 10 | 95 | 200 | 1 |
OT – Operative time; Postop LOH – Postoperative length of hospitalization
Three patients had prior surgeries for renal stone. One patient underwent ipsilateral PNL four years back, one patient came for clearance post PNL and one patient underwent pyelolithotomy 7 years back. This patient had bilateral staghorn calculi and underwent bilateral AN.
The mean (SD) weight was 53.67 (11.61) kg, mean (SD) blood urea was 49.89 (30.24) (range: 19–85 mg/dL) and mean (SD) serum creatinine was 2.94 (3.04) (range: 0.9–9.9) mg/dl. Two CKD patients were on maintenance haemodialysis. Mean (SD) haemoglobin was 10.89 (1.7) (range: 9-14.8) gm/dL. Preoperative urine culture was sterile in nine patients, Escherichia coli and Proteus vulgaris were identified in 2 patients each. Ultrasound was done in all 13 patients. The mean (SD) kidney size was 10.66 (1.53) (range: 9-14.5) cm. All patients had staghorn calculi occupying all calyces with largest stone measuring 6 cm. Intravenous pyelogram and contrast enhanced computed tomogram were done in 12 out of 14 patients and the kidney showed good function in all patients.
Indications and surgical procedure: The indications for AN in our patients were complex staghorn calculi involving pelvis and all calyces in 10 patients, massive stone burden with infundibular stenosis in two patients and failed PCNL in one patient. All patients were operated under general anaesthesia. Left:Right ratio was 9:5.
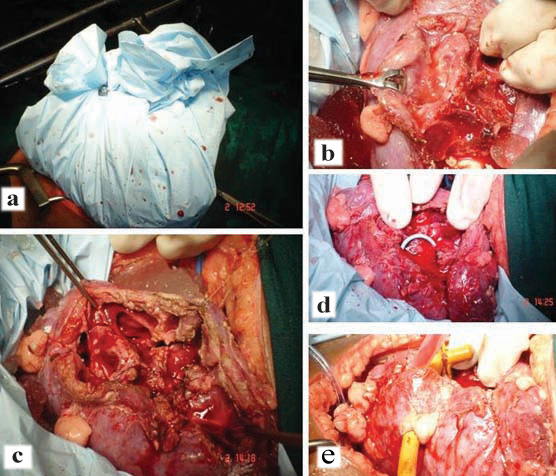
Standard operative technique described was followed in all patients. After induction, Foley cathetrisation was done in supine position. Patient was turned to kidney position and parts were prepared and draped. Supracostal 11th/12th rib approach was used as appropriate. Posterior aspect of kidney was exposed after retroperitoneum was entered. Ureter was then looped and dissection at hilum was done to identify renal artery, vein and then the posterior segmental artery. It was clamped and immediately sterile crushed normal saline ice slush was placed around for 15 minutes [Table/Fig-2a]. At this point 100 ml of 20% mannitol was infused. The avascular plane of brodel was marked with cautery and after confirmation with blanching, incision was made in this avascular plane on the convex border of the kidney. Blunt separation of parenchyma was done along the plane with back of Bard Parker knife handle. Care was taken to avoid the renal poles. The calyx was incised with knife and adjacent infundibula were opened into the calyces [Table/Fig-2b]. After all stones were removed, calicoplasty was done with 5-0 polydiaxonone sutures [Table/Fig-2c]. A 5F 26 cm Double J Stent (DJS) [Table/Fig-2d] and nephrostomy in selected cases were placed and pelvis was closed with 4-0 vicryl sutures [Table/Fig-2e]. Arterial clamp was released and reapplied to allow suture of bleeding vessels with figure-of-8 sutures with 4-0 vicryl. Renal parenchyma and capsule were closed with 3-0 vicryl interrupted sutures. A retroperitoneal drain was placed. The wound was closed in layers.
Intraoperative images depicting stages of anatrophic nephrolithotomy; a) Posterior segmental artery clamped and sterile crushed normal saline ice slush applied around kidney and covered for 15 minutes; b) Calyx incised and adjacent infundibula opened; c) Calicoplasty with 5-0 polydiaxonone sutures; d) Double J stent placement in renal pelvis; e) Nephrostomy placement and renal pelvis closure.
Operative details, outcomes and complications: The mean (SD) duration of surgery was 195.35(41.83) (range: 130-220) minutes. All 13 patients received 100 ml of intravenous mannitol. The mean (SD) in situ cold ischemia time was 47.64(5.27) (range 39-60) minutes. Nephrostomy tube was placed in 7 (50%) renal units. Retroperitoneal drain and DJS were placed in all 13 patients. Postoperatively two CKD patients required maintenance haemodialysis. The median (IQR) estimated blood loss was 130 (75) ml and the mean (SD) haemoglobin drop was 1.5 (1.9 gm/dL) (range 0.8–2.6 gm/dL). Based on renal units, three patients did not need transfusion, four needed 1 unit PRBC, six needed two units PRBC and one needed 5 units PRBC transfusion. There was no perioperative mortality. Surgical site infection was seen in two patients – Escherichia coli sensitive to piperacillin-tazobactam and cefoperazone-sulbactam (preoperative urine culture sterile) and urosepsis in two patients, urinary tract infection in E.coli and responded to antibiotics. Two patients with CKD required ventilation, inotropes and ICU care. Two patients developed haematuria with clot retention which settled with conservative management in one patient with CKD and persistent bleeding in one patient lasted for 15 days in nephrostomy which settled with conservative management.
The mean (SD) time to clamp nephrostomy clamping was 7.11 (7.15) (range 4-23) days and nephrostomy removal was usually after 24 hours of clamping at a mean (SD) of 8.78 (7.6) (range 5-24) days. Drain removal was at a mean (SD) of 9.11 (6.15) (range 5-22) days. Mean (SD) postoperative LOH was 15.44 (7.14) (range 8-26) days.
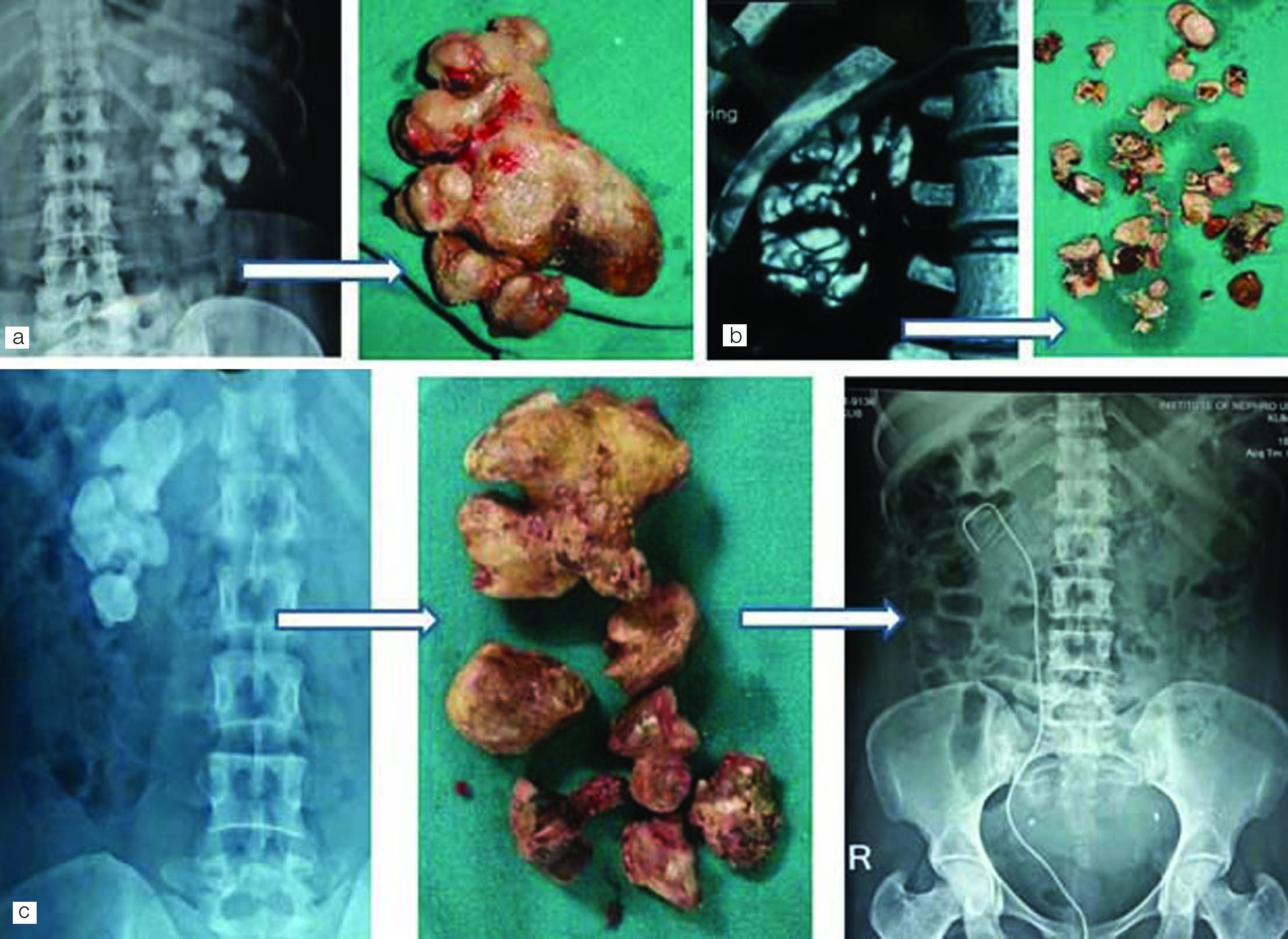
Residual calculi: For residual calculi, SWL was performed in three patients and conservative management (0.3–0.6 cm) in five patients and near complete clearance (residual 0.3 cm) was achieved. The median (IQR) clearance was 95 (7.5%). Three patients had 100% clearance, three had 95% clearance, three had 90% clearance with one patient needed SWL and three had 85% clearance with two needed SWL [Table/Fig-3a-c].
a,b) Preoperative radiological image and calculi retrieved after anatrophic nephrolithotomy; c) Preoperative radiological image, calculus retrieved after AN and postoperative X-ray kidney, ureter and bladder showing complete clearance with double J stent in situ.
Follow up: The mean (±SD) follow up period was 15.4±11.2 months. Stent removal was done in all patients between two to eight weeks. One patient had re-admission for ipsilateral pyelonephritis with a small distal ureteric calculus which resolved with stenting and intravenous antibiotics after a period of one year. Two patients with CKD died after 12 and 15 months, due to progression of disease. There was no renal failure or new calculi during the follow up period.
Discussion
AN was designed to minimize renal parenchymal damage but few complications have been reported. A temporary and occasionally a permanent decrease in renal function, significant postoperative bleeding requiring transfusion, vascular wall damage and ischemia/reperfusion injury of kidney due to renal artery clamping and it is technically much more difficult than doing an extended pyelolithotomy [2].
Han SH et al., reported 24 cases of AN. There were no operative deaths and eight transient postoperative complications. The mean operative time was 250 minutes and mean cold ischemia time was 22.44 (15-25) minutes. They reported an average LOH of 10.3 days and 17.4 days in complicated cases. Postoperative evaluation in 16 out of 24 patients, seven out of 16 (43.8%) had residual calculi (due to lack of intraoperative X-ray) and nine out of 24 had complete clearance. About 14 patients had residual fragments [4].
Jaffery AH et al., reported their series of 100 cases with a mean operative time of 76.93 (45–190) minutes and mean cold ischemia time of 22.44 (15-25) minutes [Table/Fig-4]. One patient needed nephrectomy for uncontrollable haemorrhage and 7% had secondary haemorrhage needing readmission, out of which 4/7 needed angioembolisation. Around 12% patients (including three with secondary haemorrhage) needed transfusion and 7% had residual fragments out of which four cleared spontaneously and three needed ESWL (8 mm–1 cm) [5]. Morey AF et al., reported their experience of 15 cases with a mean operative time of 3.7 hours, mean blood loss of 325 ml and mean hospital stay of 4 days. Three patients had residual stones [6].
Comparison with contemporary AN series.
| Parameter | Our series | Open AN [5] | Lap AN (LAN) [1] | Retro- peritoenal LAN [7] | Robotic assistedLAN [8] |
|---|
| Number of patients | 13 (14 renal units) | 100 | 25 | 11 | 7 |
| Mean OT, min | 163.3 | 76.93 | 170 | 139 | 158 |
| Ischemia time, min | Cold-47.64 | Cold-22.24 | Warm-32 | Warm-31 | Warm-37 |
| Clearance | 95%SWL in 3 units; 22.2% complete clearance | 93 patients complete clearance; SWL in 4 out of 7patients | 2 patients underw- entSWL | 1 patient underwent SWL | >90% 29% patients had complete clearance |
| Complications | Persistent bleed in one case | 8 out of 100 patients | 1 patient had complications; 2 patients converted to open AN | None reported | None reported |
| Blood loss, ml | 130 | Not mentioned | <100 ml | No transfusion | 121 |
OT – operation time; SWL – shock wave lithotripsy
Deger S et al., reported successful Laparoscopic AN (LAN) with no DJ stenting in five patients with no conversion for a median stone size 53 mm with mean operative time 170 minutes and mean warm ischemia time of 32 minutes with no cooling system. The EBL was <100 ml with no need of transfusion and mean hospital stay 5.4 days. Patients were discharged after drain removal and residual calculi was seen in two patients needing ESWL. Similarly, 25 procedures in 24 patients with conversion to open in two patients and nephrectomy in one patient and DJ stent in 3 (12%) patients were reported [3].
Zhou L et al., reported their experience of retroperitoneal LAN in 11 patients with a mean age of 55 years and mean stone size of 52 mm [Table/Fig-4]. The mean operative time was 139 minute with a mean warm ischemia time of 31 minute. No blood transfusion was needed and one patient with 8 mm residual calculus needed ESWL [7]. King S et al., reported robotic LAN in seven patients with a mean age of 47 years [Table/Fig-2]. The mean robotic time was 158 min with a mean warm ischemia time of 35 minutes and mean EBL of 121 ml. The mean LOH was three days and five out of seven patients had >90% clearance with two out of 7 (29%) having complete clearance [8].
Conclusion
Anatrophic nephrolithotomy thus is a valid approach for managing large staghorn calculi failed minimally invasive approaches, patients with comorbidities like COPD and achieves 80%-100% clearance without much secondary interventions. Renal function is preserved and with the emergence of laparoscopy and robotic assistance, postoperative stay is minimized with expedited recovery and comparable results with gold standard open surgery.
OT – Operative time; Postop LOH – Postoperative length of hospitalization
OT – operation time; SWL – shock wave lithotripsy