Pericardial Haemangioma: A Common Tumour in an Unusual Location: Case Report and Review of Literature
Rufus Sam Vargis1, Manjiri Phansalkar2, Somanath Padhi3, Dilip Phansalkar4, Sanjay R Nair5
1 Post Graduate, Department of Pathology, Pondicherry Institute of Medical Sciences, Pondicherry, India.
2 Professor, Department of Pathology, Pondicherry Institute of Medical Sciences, Pondicherry, India.
3 Associate Professor, Department of Pathology, Pondicherry Institute of Medical Sciences, Pondicherry, India.
4 Professor, Department of Radiology, Pondicherry Institute of Medical Sciences, Poindicherry, India.
5 Assistant Profesor, Department of Cardiothoracic Surgery, Pondicherry Institute of Medical Sciences, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rufus Sam Vargis, Room No. 204, Annex Block, Pondicherry Institute of Medical Sciences, Kalapet-605014, Pondicherry, India.
E-mail: rufusvargis@gmail.com
Overall incidence of primary cardiac tumour ranges from 0.0017% and 0.27% at autopsy. Cardiac haemangiomas are rare, and account for 2.8% of benign cardiac tumours. Pericardial haemangiomas, in particular are extremely rare. Pericardial haemangiomas are reported to present with a variety of symptoms such as dyspnea, palpitation, atypical chest pain. Other symptoms like obstruction of blood vessels, cardiac tamponade, or pericardial effusion may result due to compression of surrounding structures. Here, we report a case of pericardial haemangioma in a patient who presented with breathlessness and cough.
Cavernous haemangioma, Cardiac tumours, Tamponade
Case Report
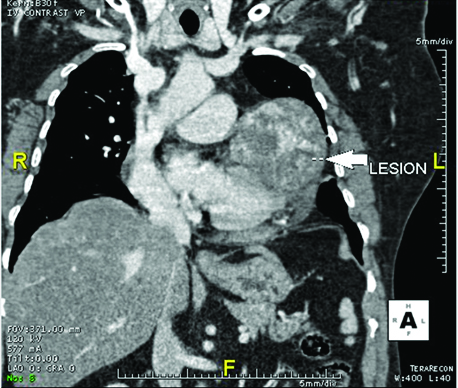
A 63-year-old female presented to pulmonary medicine OPD with complaints of breathlessness and cough for two weeks and intermittent fever for one week. She had pain in the left side of her chest for six months. She was a known case of diabetes mellitus but was not on any treatment. On admission, her blood pressure was 130/90 mmHg, pulse rate of 96/min, respiratory rate of 18/min and her SpO2 was 98% at room air. On examination, her heart sounds were normal (no murmurs heard), respiratory system examination revealed bilateral normal vesicular breath sounds with bilateral wheeze, central nervous system and per abdomen examination were unremarkable. A 2D ECHO done revealed a normal study with ejection fraction of 60%. Pulmonary function test showed a restrictive lung disease. Upon chest x-ray she was found to have a homogenous opacity in her left lung lower zone and CT scan revealed a pericardial mass in the posterior aspect with non-homogenous and irregular contrast enhancement in axial and coronal images, along with minimal pleural effusion [Table/Fig-1]. Decision for surgical removal of the mass was taken due to clinical symptom of breathlessness which could have been produced due to pressure effect on the lung due to the pericardial mass.
CT scan showing pericardial mass with non-homogenous and irregular contrast enhancement seen in axial and coronal images with minimal pleural effusion;
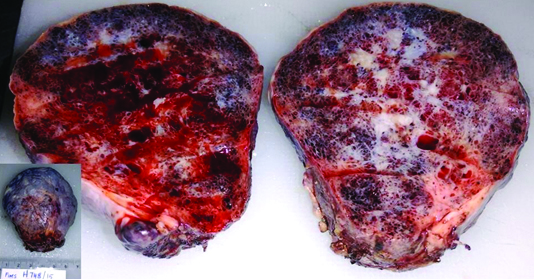
She underwent anterolateral thoracotomy and excision of the mass was done which was arising from the pericardium, in the posterior aspect. There was no extension of the mass into any cardiac chamber. The mass was sent for histopathological examination and gross examination revealed a soft cystic mass weighing 100 gm and measuring 7 x 6.5 x 5 cm. Outer surface appeared smooth and had a fibrous covering. Cut surface was hemorrhagic with oozing of blood and had spongy, cyanotic appearance. Spongy spaces were filled with blood. Central portion showed grey white areas [Table/Fig-2].
Cut section of lesion was hemorrhagic with oozing of blood and has spongy, cyanotic appearance. Spongy spaces are filled with blood. Inset Soft cystic mass, smooth outer surface with a fibrous covering.
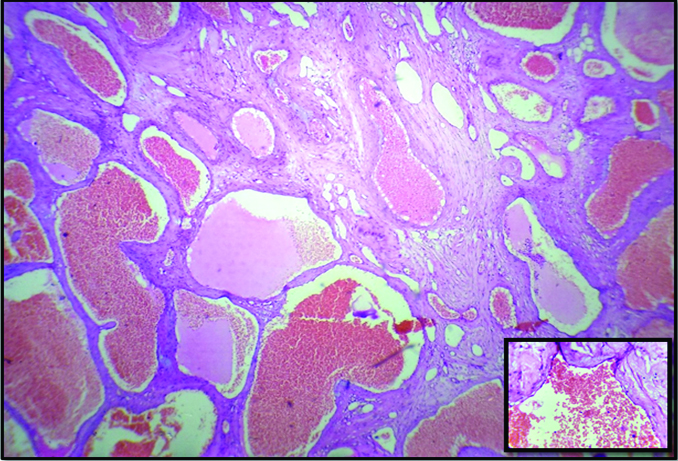
Microscopic examination showed a lesion covered by thick fibro-collagenous covering with focal flattened mesothelial lining on the surface. The lesion was composed of numerous irregular, cavernous spaces set in a loose fibrous stroma. Cavernous spaces had thin walls lined by single layered endothelium, few vessels showed smooth muscles [Table/Fig-3]. Most of the spaces were filled with blood, while occasional spaces showed fresh thrombi. Stroma showed focal myxoid change. The patient eventually died due to co-morbidities in the postoperational period.
Numerous cavernous spaces filled with blood. (H&E, 10X), Inset Cavernous spaces filled with blood and lined by single layer of endothelial cells. (H&E, 40X).
Discussion
The term haemangioma has been applied broadly to any benign, non-reactive vascular process with increase in normal or abnormal appearing vessels. The international society for the study of vascular anomalies has recommended that the term can be applied to lesions arising from cellular proliferation, composed of capillaries and which grow in disproportionate manner. However, commonly haemangiomas are classified as capillary and cavernous type [1].
Cardiac tumours are rare tumours [1]; of that pericardial haemangiomas are rarest primary tumours of the heart and comprise 2% to 5% of benign cardiac tumours. They arise from the endocardium, myocardium, or epicardium/pericardium and most commonly are found to arise from the ventricles followed by atria [2]. In the present case, the tumour was found to arise from the anterior aspect of pericardium and extending into the mediastinum.
The clinical presentation depends on the location and size of the haemangioma, and is associated with a wide variety of symptoms like dysrhythmia, heart failure, chest pain, blood vessel obstruction, effusion or respiratory symptoms like cough, breathlessness or dysphagia. Pericardial haemangiomas are clinically insignificant, and are diagnosed incidentally when patients present with other complaints, in most cases [3]. Less common presentations include consumption coagulopathy and constrictive pericarditis [4]. This case presented with respiratory symptoms which were-persistent cough and breathlessness.
Although pericardial tumours are rare, with the recent increased use of radiological methods in clinical practice, these tumours are being increasingly recognized, which permits early diagnosis and treatment. On literature review, 13 cases were found to the best of our knowledge, in the past 50 years. Details of these previously reported cases are given in the table [Table/Fig-4] [1-12].
Details of reported cases on pericardial hemangioma.
| Author | Year | Cases | Age of Patient | Clinical Features | Imaging Studies | Surgery | Histopathology | Outcome/Prognosis | Associations |
|---|
| Charles Wender JEA [4] | 1966 | 1 | 16, F | Cough | X-Ray Cardiomegaly | Pericardiectomy | Cavernous & Capillary | Well at discharge | Multiple sites-Pericardium, visceral Pleura and parietal pleura |
| Yoshikawa M et al., [3] | 1987 | 1 | Infant | Tachypnea | X-Ray-Enlarged heart, ECHO effusion | Thoracotomy | Capillary | Well at discharge | - |
| Kitagawa N et al., [5] | 2003 | 1 | Neonate | Cardiac effusion | - | Thoracotomy | - | Well at discharge | - |
| Ramasubbu K et al., [6] | 2004 | 1 | 44, M | Chest pain | ECHO – Bulge | Sternotomy | Capillary | - | - |
| Zeina AR et al., [2] | 2007 | 1 | 37, F | Syncope, Palpitations | X-Ray-Bulge, ECHO, CT | Thoracotomy | Cavernous | - | - |
| Wu G et al., [7] | 2009 | 1 | 2m, M | Respiratory Infections | X-Ray-Cardiomegaly, ECHO, CT, MRI | Nil | Cavernous | Regression of the Tumour | - |
| Ediae J et al., [8] | 2009 | 1 | 75, M | Murmur | MRI – Mass, CT | Thoracotomy | Cavernous | - | - |
| Leibetrau C et al., [9] | 2010 | 1 | 58, F | Pericardial Effusion | ECHO, CT, MRI | Sternotomy | Capillary | - | Dendroglioma |
| Omura K et al., [10] | 2010 | 1 | 78, F | Leg edema and exertional dyspnea | ECHO, MRI | Pericardiocentesis, Surgical resection | Capillary | - | - |
| Gupta N et al., [11] | 2013 | 1 | 40, M | Chest pain, Palpitation | ECHO, Doppler | Sternotomy | Cavernous | Well after 6months | - |
| Ben Yousseff A et al., [12] | 2014 | 2 | 24, F | Palpitation | ECHO – Mass | - | - | Well at discharge | - |
| 79, F | Hypertension | ECHO, MRI – Mass | - | - | - | - |
| Sabeti S et al., [1] | 2015 | 1 | 72, M | Incidental Finding | ECHO, USG, MRI | Open Heart Surgery | Cavernous | Died, Comorbidities | Associated with hepatic haemangiomas |
The diagnosis is made by transthoracic echocardiography, computed tomography, magnetic resonance imaging, or cardiac catheterization demonstrating tumour blush. The utility of echo-cardiography in diagnosis of haemangioma is limited. Although echocardiography can locate the tumour, MRI is superior in qualitative diagnosis of the tumour due to excellent contrast resolution [6]. In the present case, the patient had presented with symptoms of cough and breathlessness. The pericardial mass was found incidentally on CT imaging studies. On histopathological examination done on the excised mass, it was found to be a haemangioma which was arising from the pericardium. Pericardial haemangiomas are composed of vascular spaces that are lined by endothelial cells, and they are classified based on histology into three types: tumours composed of numerous dilated, thin-walled vascular spaces which are lined by flattened endothelium and are called cavernous type, the smaller capillary type is composed of capillary like vessels and lined by plump endothelial cells and the dysplastic malformed arteries and veins called the arteriovenous type [1]. The present tumour is found to be of cavernous type and is arising from the pericardium.
These pericardial haemangiomas are unpredictable, they can undergo varied growth rate ranging from dormancy, to accelerated growth, to spontaneous regression [11,12].
Treatment includes operation with removal of the tumour for diagnostic purposes and to prevent mechanical consequences of tumour growth [11,12].
Conclusion
Since pericardial haemangiomas are extremely rare tumours, with very few cases reported, the precise preoperative diagnosis is difficult. Use of radiological methods can be helpful in detecting these and help in early diagnosis and treatment.
Pathological features are similar to all cavernous haemangiomas of other sites, while they can be symptomatic in few patients due to the location of these tumours and present with pressure symptoms on the heart, lungs or blood vessels. This case is being reported for its extreme rarity.
[1]. Sabeti S, Zahedifard S, Soleimantabar H, Zarghampour M, Toutkaboni MP, Coexistence of pericardial and hepatic hemangiomasIran J Pathol 2015 10(2):169-72. [Google Scholar]
[2]. Zeina AR, Zaid G, Sharif D, Rosenschein U, Barmeir E, Huge pericardial hemangioma imagingCirculation 2007 115(10):315-18. [Google Scholar]
[3]. Yoshikawa M, Hayashi T, Sato T, Akiba T, Watarai J, Nakamura C, A case of pericardial hemangioma with consumption coagulopathy cured by radiotherapyPediatr Radiol 1987 17:149-50. [Google Scholar]
[4]. Charles wender JEA, Constrictive pericarditis associated with hemangioma of the pericardiumAm Heart J 1966 72(2):255-58. [Google Scholar]
[5]. Kitagawa N, Ohhama Y, Fukuzato Y, Take H, Shinkai M, Nish T, Pericardial hemangioma presenting fetal cardiac tamponade and postnatal bronchostenosisPediatr Surg Int [Internet] 2004 20(5):376-77. [Google Scholar]
[6]. Ramasubbu K, Wheeler TM, Reardon MJ, Dokainish H, Visceral pericardial hemangioma: Unusual location for a rare cardiac tumourJ Am Soc Echocardiogr 2005 18(9):7-8. [Google Scholar]
[7]. Wu G, Jones J, Sequeira IB, Pepelassis D, Congenital pericardial hemangioma responding to high-dose corticosteroid therapyCan J Cardiol [Internet] 2009 25(4):e139-40. [Google Scholar]
[8]. Ediae J, Lim PS, Addonizio VP, Kostacos E, Bell K, Litt HI, Pericardial hemangioma taking origin from the posterior wall of the left atriumAnn Thorac Surg. [Internet] 2009 87(6):e54-56. [Google Scholar]
[9]. Liebetrau C, Szalay Z, Von Gerlach S, Möllmann H, Nef H, Hamm C, Pericardial hemangioma vascularized via left anterior descendingClin Res Cardiol 2010 99(6):405-07. [Google Scholar]
[10]. Omura K, Onishi T, Yamawaki K, Omar AM, Kanzawa M, Ishida T, A rare case of pericardial hemangioma with bloody pericardial effusionJournal of Cardiology Cases 2010 2(1):e15-19. [Google Scholar]
[11]. Gupta N, Intrapericardial hemangioma: A case reportJ Clin Diagnostic Res 2013 7(1):169-70. [Google Scholar]
[12]. Ben Youssef A, Zairi S, Ouerghi S, Ayadi A, Bousnina M, Berraies F, Epicardial cavernous hemangioma: a two - case reportsTunis Med 2014 92:268-71. [Google Scholar]