CTS, an entrapment of the median nerve in the volar wrist area, is a common disorder. Although patient history and clinical examination give an indication of CTS, Nerve Conduction Velocity (NCV) measurement is the gold standard for diagnosis of CTS and should therefore be performed [1]. A proximal stimulation of the arm, shoulder or cervical spine in patients with CTS can sometimes provoke the typical symptoms of CTS [2]. Myofascial pain from Trigger Points (TPs) in infraspinatus muscle give rise to referred pain and parasthesia in shoulder, arm and hand and these symptoms may mimic the carpal tunnel symptoms in patients with normal nerve conduction studies [3]. However, in a recent multiple-blind, controlled study, we showed the validity of a new proximal test in patients with proven CTS: IsT [4]. With this test, a standardized pressure is exerted on a defined point on the lateral border of the infraspinatus muscle. We showed that this test can provoke symptoms in patients with proven CTS, as diagnosed with NCV of the median nerve, also in the absence of TPs (TPs as defined by Simons [5]). As control stimulation, exerting exactly the same pressure on the middle of the belly of the infraspinatus muscle (the typical place for provoking TP symptoms according to Simons) was not significantly associated with CTS symptoms. The IsT is performed by exerting a standardized pressure on the lateral angle of the infraspinatus muscle from a predefined angle for a maximum of 30 seconds [Table/Fig-1], with the subject in a sitting position with his/her arms on the thighs and forearms in a relaxed, supinated position. Investigating 64 arms with or without CTS according to NCV criteria, IsT showed no significant difference to the NCV (sensitivity: 69.7%, specificity: 87.1%, McNemar’s test for independence: p=0.18) and proved the significance of the IsT with regard to symptoms (Fisher’s-exact test: p<0.001) [4]. Possible mechanisms were discussed in our previous study and it could be that the IsT stimulates a latent TPs. This has been shown to induce sympathetic activation [6,7], leading to local reduction of arterial blood flow and decreasing pain threshold, but direct evidence for this mechanism in CTS is still lacking.
Independent from the underlying pathophysiology, a clinical test should not only be valid but also reliable. Moreover, in the case of CTS, it is common that professionals from more than one medical discipline (e.g., general practitioner, neurologist, surgeon, physiotherapist), each with his or her own expertise, form their own clinical opinion about a patient. Therefore, in the present study we tested the reliability of the IsT in the same group of subjects from the previous study when performed by two raters from different medical disciplines, within a time interval of two to four weeks, and at different localities.
Materials and Methods
In an inter-rater reliability study, subjects with and without possible CTS were investigated with the IsT by two raters in a blinded fashion, by a first rater in a physical therapy praxis and with an interval of two to four weeks, by a second rater in a Department of Neurology. All subjects were recruited from a patient collective that reported for treatment in a physical therapy practice because of ailments like knee or hip problems. No subject was referred because of CTS. During examination, they were asked whether they sometimes felt a tingling sensation in their fingers.
Participation was voluntary, and informed consent of subjects was obtained following detailed verbal and written instruction. Subjects could withdraw from the study at any time without having to state a reason or suffer any disadvantage as a result thereof. The study was approved by the local Ethics Committee of the Freiburg University and in accordance with the Helsinki Declaration of 1975, as revised in 2000.
Inclusion and exclusion criteria were the same as in our previous study [4]. Inclusion criteria for the arms in the CTS group were: Paresthesia in phalanges I-IV (I= thumb) at night, and/or when driving, cycling, reading a newspaper, knitting, or pursuing similar activities (one of the activities sufficed for inclusion), as well as recurrent symptoms in the last three months, with at least two times within the last two weeks. Also, recurring CTS symptoms after previous surgery with a symptom free interval of at least six months was permissible for inclusion.
Exclusion criteria for all arms of all subjects were: Recent operation or any unresolved condition in one hand, arm or shoulder, or known disc problems in the cervical or thoracic spine. To rule out painful conditions in the shoulders and neck, all subjects were asked to clasp their hands behind their backs and necks in order to examine the shoulders. To examine the cervical spine, all anatomical directions of movement of the Cervical Spine were tested (flexion, extension, lateral flexion, rotation). Additionally, the spurling test (The examiner turns the subject’s head to each side while extending and applying downward pressure to the top of the subject’s head) was performed.
Other exclusion criteria were: Any known disease of the central nervous system, e.g., stroke, Parkinson’s disease or multiple sclerosis; a disease with involvement of the peripheral nervous system, like polyneuropathy, or possible involvement, like rheumatic disorder; and fibromyalgia or pregnancy.
Symptoms could be either unilateral or bilateral in those subjects with symptoms, whereas all arms without symptoms (i.e., also those in subjects with contralateral symptoms) were assigned to the control group. None of the volunteers took regular analgesic drugs for CTS or any other painful conditions.
In all subjects, two separate neurologists (FA and RL) who were blinded to the symptoms of the subjects and the results of the raters performed ncv to determine whether a CTS was present according to the American Association of Electrodiagnostic Medicine [1]. All arms were examined with the IsT as described previously [4]. For determining whether the IsT was positive or negative in those subjects who had reported symptoms, only one of two statements from the subject was permissible: 1) “Yes, these are my symptoms”; 2) “No, these are not my symptoms”.
The IsT was performed by two experienced clinicians from different medical disciplines: Rater A (MM) a long-time physiotherapist and Rater B (MR) a long-time neurologist. The first examination by Rater A was undertaken at a physiotherapy practice in Freiburg, Germany, the second examination by Rater B at the Neurology Clinic of the Freiburg University Hospital, Germany. Rater B was blinded for the findings obtained by Rater A. Intentionally, a period of two to four weeks was left between the examinations by the two raters, reflecting the average waiting period for referral.
Statistical Analysis
Cohen’s kappa (κ) coefficient was calculated from a contingency table as a measure of inter-rater reliability for Rater A and Rater B.
The kappa score is influenced, however, by prevalence (prevalence index = PI) and bias (bias index = BI), factors to be considered in the interpretation. The PI varies from -1 to +1, and 0 applies if + and - responses are equally likely. The BI varies from 0 to 1, with 0 indicating no bias.
Since subjects with unilateral symptoms serve as their own control, the Chi-square test does not apply and the McNemar test was used to investigate dependencies between arms. In four subjects, only one arm was included and no contralateral control arm was available, so the McNemar test included 60 arms from 30 subjects. This test was also used to compare the two raters.
Results
Thirty-four subjects aged 35-86 years (mean: 59.12±14.11; n=29 female, n=5 male), participated in the study. In these subjects, 31 arms fulfilled the inclusion criteria with regard to possible CTS symptoms. Of the 68 arms in all 34 subjects, four arms (two right and two left) were not included for further analysis on account of recent surgery or unilateral localized pain in one shoulder. Thus, a remaining total of 64 arms could be examined.
Symptoms indicative of possible CTS were reported in 16 subjects on the left side according to the inclusion criteria, [Table/Fig-2]. All 16 arms and an additional one showed an NCV compatible with CTS. From these, Rater A was able to provoke symptoms with the IsT in 13 cases and Rater B in the same subjects and in one additional case. On the right side, 15 subjects reported symptoms and all arms and an additional one showed NCV results compatible with CTS. From these, Rater A could provoke symptoms in 11 cases and Rater B in the same subjects and in one additional arm.
Overview of results: Symptoms (+) / no symptoms (-): Report of presence (+) or absence (-) of typical symptoms by subjects during inclusion in the study for the left or right arm. No of hits: symptoms were recognized by the subjects as typical for their complaint (+), or no such symptoms could be provoked by IsT (-). CTS+ / CTS -: presence (+) or absence (-) of CTS according to NCV criteria.
| Arm | Symptoms + / no Symptoms - | Rater A No. of hits | Rater B No. of hits | CTS + / CTS – |
|---|
| left | 16+ | 13+ | 14+ | 17+ |
| right | 15+ | 11+ | 12+ | 16+ |
| left | 16- | 19- | 18- | 15- |
| right | 17- | 21- | 20- | 16- |
| Total | 64 | 64 | 64 | 64 |
No symptoms were reported in 16 subjects on the left side. Rater A and Rater B could not provoke symptoms in these arms, nor in an additional three and two arms, respectively (overlap of Rater A and B: 15 arms). Of these 16 arms, 15 had a normal NCV. No symptoms were reported by 17 subjects on the right side. Rater A and rater B could not provoke symptoms in an additional four and three arm, respectively (overlap of Rater A and B: 12 arms). In these 17 arms, 16 had normal NCV.
To calculate inter-rater reliability, results from Rater A were compared against those from Rater B [Table/Fig-3]. Analysis based on the kappa calculation produced a kappa score of κ=0.868. Proportional agreement produced a score of 0.93, a BI of -0.03 and PI of -0.21. No statistical dependencies could be ascertained between the measurements of Rater A and Rater B by the McNemar test (p=0.6171).
Ist: Infraspinatus provocation Test. Positive: The Ist provoked symptoms that were recognized by the subjects. Negative: No such symptoms could be provoked with the IsT. Calculation with Cohen-Kappa-Test. Kappa: κ=0.868; Proportional agreement (0.93); BI (-0.03); PI (-0.21); McNemar-test p=0.6171
| Arms | | Rater B | | |
|---|
| Positive | Negative | Total |
|---|
| Rater A | Positive | 23 | 1 | 24 |
| Negative | 3 | 37 | 40 |
| Total | 26 | 38 | 64 |
Likewise, no significant dependencies were found between the left and right arm from either rater (Rater A: p=0.4533, Rater B: p=0.5023) in those 30 subjects in which both arms could be examined [Table/Fig-4].
Comparison of IsT between right and left arm for Rater A and B. The McNemar test could only be performed for subjects in which both arms were included (in four out of 34 subjects, only one arm was included, resulting in 30 subjects = 60 arms).
| RaterA/B | | Right Arm | | |
|---|
| Positive | Negative | Total |
|---|
| Left Arm | Positive | 14/14 | 10/12 | 24/26 |
| Negative | 6/8 | 30/26 | 36/34 |
| Total | 20/22 | 40/38 | 60/60 |
In each cell, the first number refers to Rater A, the second to Rater B. Example: The cell “left arm positive” and “right arm positive” means that in seven subjects, both arms tested positive for the IsT, resulting in 14 arms from the same subjects, both for Rater A and Rater B. McNemar’s test for the right and left arm: Rater A: p=0.4533. Rater B: 0.5023. Therefore, no significant dependencies for right and left arms in the same subjects were found (p>0.05).
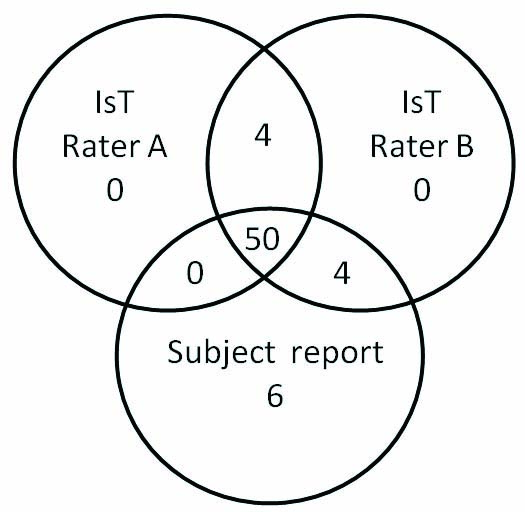
[Table/Fig-5] illustrates the congruence of the IsT for Raters A and B and the report of the subjects (symptoms or lack of symptoms). In those cases with incongruent findings, we did not find a discernable pattern.
Display of the total number of positive and negative concordances of Rater A and B, compared with the report of the subjects at inclusion regarding possible CTS. In 50 arms (overlap of Rater A, Rater B and subject report), the result of the IsT from both raters corresponded to the report of the subjects at inclusion (either symptoms suggestive of CTS or no such symptoms).
Discussion
In 50 out of 64 arms, the presence or absence of symptoms indicated by the subjects was in accordance with the results of IsT from both raters [Table/Fig-2]. A high level of inter-rater agreement could be proven statistically: the kappa score of κ=0.868, which lies between 0.81-1.0, is interpreted as almost perfect. A value of 93% was found for proportional agreement. The PI, with an outcome of -0.21, is in a range which indicates that the probability of positive and negative responses is almost equal. The BI at -0.03, shows that the probability of error can be classified as very low. The McNemar test was also unable to ascertain a dependency of the results of the two raters (p=0.6171) [Table/Fig-3]. For neither rater there was an indication of a dependency between arms of subjects [Table/Fig-4].
Nonetheless, there were still 14 out of 64 arms in which there was no complete congruence between the testimony of the subjects and the results of IsT from the two raters [Tabel/Fig-5]. The time interval of two to four weeks between the examinations of Rater A and Rater B was introduced on purpose to simulate everyday situations. The initial diagnostics are usually performed by a medical practitioner or therapist and the second examination by a neurologist, who assumes responsibility for instrumental diagnostic measures. Time of measurement does play a role [8] and might have caused the discrepancy of results in four arms between Rater A and Rater B. It is worth mentioning, though, that the opposite sides in these four subjects always agreed between the raters. However, also a time period that is too short might influence results, since the performance of a test in itself could have a therapeutic effect or deteriorate symptoms.
Further factors of influence could be the technique of the examiner as well as the baseline position of the subject: these may influence the anatomical conditions and certainly prevent the equal exertion of the pressure direction and force [8,9]. In this study, the baseline position of the subjects was standardized and the present results apply exclusively to such a position. Furthermore, it should be taken into account that the baseline position of the examiner will inevitably change depending on the side to be tested. A right-handed individual might find it easier to exert pressure on the right scapula rather than on the left one. However, the pressure point is also very easily found with the other hand, and the results did not reveal any significant difference between the right and left sides – neither for Rater A nor for Rater B [Table/Fig-4].
Other factors to be considered are the environment and hence, the locality of the examination. An individual may feel comfortable or uncomfortable in certain surroundings and mental stress could increase the activity of the sympathetic nervous system [10] or increase muscular tension, and in turn soft-tissue resistance. These aspects were not investigated in this study. But there is one report which confirms the influence of the sympathetic nervous system on TPs, including the shoulder [6]. Since the IsT might stimulate a latent TPs in the infraspinatus (although at an atypical location), it cannot be excluded that this factor played a role in our study.
Several studies have demonstrated that the inter-rater reliability for the identification of TPs (like tenderness, a palpable taut band or pain provocation) varies [11] and depends on the experience of the investigator [12-14]. However, we do not think that this factor plays a role in our study. For the IsT, no such palpation or experience is necessary and the correct location for the pressure point of IsT can easily be found after a few instructions by any person with medical training. As we reported before, no TPs according to the definition of Simons were found in the infraspinatus muscle of the present subjects and exerting the same pressure on the middle of the belly of the infraspinate muscle could not provoke the CTS symptoms in the patients [4].
One remaining question is whether the IsT can be applied only under the conditions covered by the described inclusion and exclusion criteria, or also irrespective of such. Hence, the IsT should be investigated for its general validity, to find out if it can similarly be employed in the presence of affections like polyneuropathy or rheumatic disease.
Conclusion
Under standard conditions, the IsT appears to be a useful test for confirming CTS, once shoulder and cervical spine symptoms have been ruled out. A high level of inter-rater reliability could be proven statistically for the IsT procedure. Therefore, the IsT appears to be not only a valid, but clearly also a reliable test, which can be used in everyday clinical use irrespective of timing, locality and medical background of the examiner.
In each cell, the first number refers to Rater A, the second to Rater B. Example: The cell “left arm positive” and “right arm positive” means that in seven subjects, both arms tested positive for the IsT, resulting in 14 arms from the same subjects, both for Rater A and Rater B. McNemar’s test for the right and left arm: Rater A: p=0.4533. Rater B: 0.5023. Therefore, no significant dependencies for right and left arms in the same subjects were found (p>0.05).