Uncovering Metabolic Syndrome among Chronic Obstructive Pulmonary Disease Patients in a Tertiary Care Hospital, India
Kamlesh Kumar Gupta1, Jitendra Singh2, Pradeep Gupta3, ML Patel4, Vivek Kumar5, Shyam Chand Chaudhary6
1 Associate Professor, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
2 Senior Resident, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
3 Junior Resident, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
4 Associate Professor, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
5 Additional Professor, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
6 Additional Professor, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jitendra Singh, Senior Resident, Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India.
E-mail: drjitengsvm@gmail.com
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is known to cause various systemic problems including Metabolic Syndrome (MetS). MetS is a group of cardiovascular risk factors. By assessing MetS, one can assess the cardiovascular disease risk. There is increasing evidence of MetS in COPD patients. However, the frequency of MetS and its individual components are not still been clearly shown which is likely to vary in different population.
Aim
To know the extent of association of metabolic syndrome and its components in patients with COPD.
Material and Methods
This study was designed as an analytical case control study. Ninety cases of COPD satisfying the inclusion criteria and 45 healthy volunteer subjects as controls were recruited over 18 months duration. Simple random sampling method was used to select all cases attending outdoor and indoor medicine department. All subjects (cases and controls) were matched for age, sex, occupation and socioeconomic status. Prior to participation in the study, written informed consent was taken from all subjects. All included subjects underwent a detailed history, clinical examination and laboratorial analysis. All subjects were assessed for MetS by using National Cholesterol Education Program-Third Adult Treatment Panel (NCEP ATP III) and International Diabetic Federation (IDF) criteria.
Results
The present study demonstrated Metabolic Syndrome (MetS) in COPD according to NCEP ATP III and IDF criteria as 14 (15.56%) and 30 (33.33%) while there was no association of MetS with controls. The frequency of its component such as abdominal obesity, systolic blood pressure, diastolic blood pressure, elevated triglyceride, reduced HDL-C and elevated fasting glucose respectively was 71 (78.89%), 25 (26.67%), 12 (13.33%), 18 (20%), 23 (25.56%) and 17 (18.78%) respectively. Dyslipidemia was found in 36 (40%) cases of COPD including 16 (17.78%) cases of elevated LDL cholesterol.
Conclusion
Our study concluded that MetS is frequent in COPD patients as compared to general population. Therefore, a comprehensive medical approach to screen all COPD patients for MetS should be done there to lower the significant risk of cardiovascular events in patients with COPD.
Cardiovascular risk, Diabetes mellitus, Dyslipidemia, Hypertension, Obesity
Introduction
According to the Global initiative for Chronic Obstructive Lung Disease (GOLD), COPD is characterized by persistent airflow limitation which is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases [1]. Studies have described that significant health changes occur as pulmonary functions deteriorate [2]. The prevalence of COPD is rising worldwide and it is the fourth leading cause of death worldwide. Its overall prevalence is estimated to be 4%-5% in our country [1,3]. The unrelated disorders in COPD patients are relatively under investigation. Patients with moderate to severe COPD often have multi organ disease like skeletal muscle wasting, lung cancer, pulmonary hypertension, ischemic heart disease, endothelial dysfunction, congestive cardiac failure, metabolic syndrome, obstructive sleep apnea, depression, vitamin D deficiency and osteoporosis [4]. However, the exact mechanism responsible for these comorbidities is not fully understood, though some studies believe that comorbidities in COPD are probably due to systemic inflammation [5]. MetS is an emerging clinical challenge which is also called as insulin resistance syndrome or syndrome X [2]. It is recognized by the findings of abdominal obesity, elevated blood pressure, elevated triglyceride, atherogenic dyslipidemia, and high blood glucose and/or insulin resistance. According to IDF, MetS is a cluster of the most dangerous heart attack risk factors. It is also defined to be associated with prothrombotic and proinflammatory states. It is estimated that 20%-25% adult population of world have MetS and these peoples have three times more risk to have a heart attack or stroke as compared to general population [6]. The elevated levels of serum cortisol due to chronic stress in COPD lead to abdominal obesity, insulin resistance, and lipid abnormalities [7]. But the definite aetiology of the MetS is not established yet. A study had shown that smoking cessation reduces the rate of decline in FEV1 in COPD patient while there is no role of pharmacological intervention to modify the progression of disease [2]. Therefore, it is important to study patients with COPD for the possible correlation with MetS and to correlate the prevalence of MetS with stages of COPD. With this background we planned this study. This study was effort to evaluate the presence of the MetS in COPD patients.
Materials and Methods
This study was designed as analytic case control study, conducted in Department of Medicine, King George’s Medical University, Lucknow, Uttar Pradesh, India from July 2014 to December 2015. All the patients with COPD attending outdoor and indoor of general medicine department were selected by simple random sampling method for this study and normal healthy individuals without COPD were taken as control. Written consent was taken from all the cases and controls. Ethical committee clearance was taken from institution.
Inclusion criteria:
Age 40 to 70 years of either sex;
Diagnosed case of COPD irrespective of duration of illness or treatment;
No signs of exacerbation of COPD;
Use of systemic corticosteroid in the preceding three months;
Newly diagnosed case with spirometric findings (FEV1/ FVC<0.7, and FEV1≤80% of predicted).
Exclusion criteria:
Seriously ill individuals;
History of coronary artery disease and/or decompensated cardiovascular disease and stroke;
Inflammatory comorbid illnesses such as inflammatory bowel disease, rheumatologic disease etc;
Respiratory disease other than COPD;
Patient immobilized for more than six months or bedridden;
Not fulfilling inclusion criteria;
Not willing individuals.
A detailed clinical history, physical examination and relevant blood investigations were carried out in all subjects (90 cases and 45 controls). Pulmonary Function Test (PFT) was done by using PK MORGAN SPIRO 232 drum based spirometry in sitting position and at room temperature from 10 am to 2 pm in Department of Pulmonary Medicine.
The diagnosis of COPD was made according to the GOLD criteria [Table/Fig-1] [1]. MetS was identified according to NCEP ATP III and new IDF criteria [Table/Fig-2] [6].
Classification of COPD according to GOLD criteria [1].
| GOLDstage | GOLDstage | Severity Symptoms | Spirometry |
|---|
| 0 | At risk | Sputum production | Normal |
| I | Mild | With or without chronic cough or sputum production | FEV1/FVC <0.7 and FEV1 80% predicted |
| II | Moderate | With or without chronic cough or sputum production | FEV1/FVC <0.7 and 50%FEV1<80% predicted |
| III | Severe | With or without chronic cough or sputum production | FEV1/FVC <0.7 and 30%FEV1<50% predicted |
| IV | Very severe | With or without chronic cough or sputum production | FEV1 <30% predicted orFEV1<50% predicted with respiratory failure or signs of right heart failure |
The new IDF definition for Metabolic syndrome [6].
| Characteristics | NCEP:ATP III | IDF |
|---|
| Waist Circumference (WC) | > 102 cm in men,> 88cm in women | ≥ 90 cm in men,≥ 80cm in women |
| Triglycerides | ≥ 150 mg/dl | ≥ 150 mg/dl |
| HDL-Cholesterol | < 40 mg/dl in men,< 50 mg/dl in women | < 40 mg/dl in men,< 50 mg/dl in women |
| Blood Pressure | Systolic BP ≥ 130 mmHg or Diastolic BP ≥ 85 mm Hg or use of antihypertensive medication | Systolic BP ≥ 130 mmHg or Diastolic BP ≥ 85 mm Hg or use of antihypertensive medication |
| Fasting plasma glucose | ≥ 100 mg/dl or use of hypoglycaemic agent | ≥ 100 mg/dl or use of hypoglycaemic agent |
| Metabolic Syndrome | Three criteria | WC + two criteria |
Statistical Analysis
Data was analysed online by using GraphPad software version QuickCalcs. The results of this study were presented in mean±SD and percentages. Mean and standard deviation were computed for all continuous variables and comparison was done using student’s t-test. Differences in the prevalence between cases and controls were tested by chi-square tests for statistical significance. Level of significance were as not significant (ns) (p-value ≥ 0.05), significant (s) (p-value 0.01 to 0.05), very significant (vs) (p-value 0.001 to 0.01), highly significant (hs)/extremely significant (es) (p-value 0.0001 to 0.001) respectively.
Results
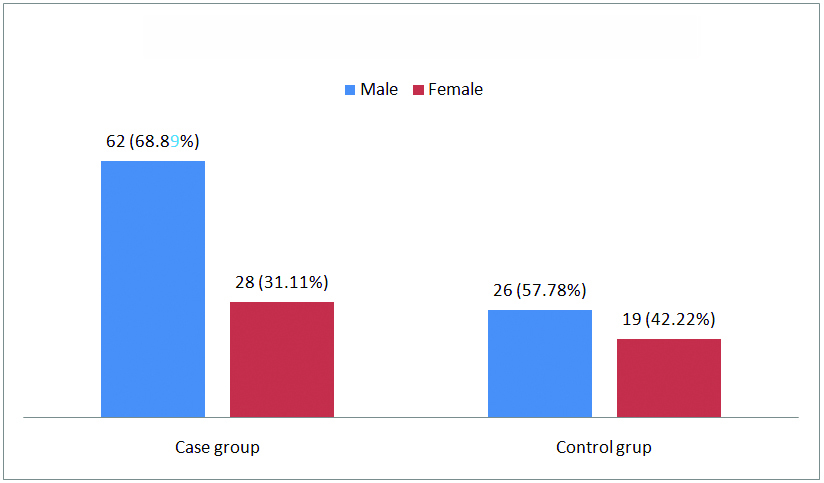
All the cases and controls were matched for age, sex, body mass index, occupation and socioeconomic status. Out of 90 cases (COPD group), 62 (68.89%) were males and 28 (31.11%) were females, whereas in control group there were 45 subjects which included 26 (57.78%) males and 19 (42.22%) females [Table/Fig-3]. The reason for difference in sex distribution may be due to that India is male prevalent country.
Gender wise distribution of subjects.
Most of the subjects were from rural areas in cases: 63 (70%) and control 27 (60%). Majority of male patients were farmer: 43 (47.78%) by occupation while 18 were females and had history of chullah cooking [Table/Fig-4].
Socioeconomic and lifestyle related characteristics of subjects.
| Characteristics | Cases (n=90) | Control (n=45) |
|---|
| Residence |
| Rural | 63(70%) | 27(60%) |
| Urban | 27(30%) | 18(40%) |
| Occupation |
| Farmer | 43(47.78%) | 17(37.78%) |
| Labourer | 27 (30%) | 13 (28.89%) |
| Official | 12 (13.33%) | 9 (20%) |
| Businessmen | 8 (8.89%) | 6 (13.33%) |
| History of chullah cooking | Male | 2/62 (3.22%) | 0 |
| Female | 18/28 (64.29%) | 1/19 (5.06%) |
The mean age in case group was 53.07±7.16 years and 54.49±7.60 years in control group. There were no statistically significant differences between the case and control group with respect to mean age (p-value = 0.2892), body mass index (p-value =0.2011) and waist circumference (0.0957) whereas, triglycerides, systolic BP, diastolic BP, fasting glucose and LDL cholesterol had statistically significant differences between the case and control group [Table/Fig-5].
Anthropometric, clinical and biochemical characteristics of subjects.
| Parameters | Cases (n=90) | Control (n=45) | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Mean age (year) | 53.07±7.16 | 54.49±7.60 | 0.2892[ns] |
| BMI (kg/m2) | 23.29±3.08 | 22.59±2.78 | 0.2011[ns] |
| WC (cm) | 94.21±9.04 | 91.56±7.80 | 0.0957[ns] |
| Triglycerides (mg/dl) | 137.11±39.34 | 119.69±16.73 | 0.0052[vs] |
| HDL cholesterol (mg/dl | 50.24±12.31 | 52.11±6.67 | 0.3436[ns] |
| Systolic BP (mmHg) | 127.33±3.21 | 118.98±7.81 | <0.0001[hs] |
| Diastolic BP (mmHg) | 81.73±3.18 | 80.04±2.32 | 0.0019[vs] |
| Fasting glucose (mg/dl) | 101.23±17.38 | 95.06±5.59 | 0.0220[s] |
| LDL cholesterol (mg/dl) | 62.16±24.72 | 48.56±22.92 | 0.0025[vs] |
Waist Circumference (WC), Triglycerides (TG), HDL cholesterol (HDL), Systolic BP (SBP), Diastolic BP (DBP), Fasting Blood Glucose (FBS), Metabolic Syndrome (MetS). Mean and standard deviation were computed for all continuous variables and comparison was done using unpaired t-test.
Among 90 cases, 36 (40%) had history of smoking including 34 (54.84%) males and 2 (7.14%) females. Dyslipidemia was present in 36 (40%) cases which was distributed gender wise as 24 (38.71%) males and 12 (42.86%) females. According to NCEP ATP III and IDF, there were 14 (15.56%) and 30 (33.33%) cases fulfilling the criteria of MetS. While there was no MetS in control. Out of 30 cases of MetS by using IDF, males were dominant by 24 (38.71%) and rest were females [Table/Fig-6].
Personal, clinical and biochemical characteristics of cases.
| Parameters | Cases (n=90) | Control (n=45) | Chi- square | p-value |
|---|
| Total | Male | Female | Total | Male | Female |
|---|
| Smoker | 36 | 34 | 2 | 0 | 0 | 0 | 24.545 | 0.0001 (es) |
| Abdominal obesity (IDF criteria) | 71 | 47 | 24 | 33 | 14 | 19 | 0.523 | 0.4694 (ns) |
| TG (≥ 150 mg/dl) | 18 | 12 | 6 | 1 | 0 | 1 | 7.840 | 0.0051 (vs) |
| HDL-C (<40 mg/dl in men, <50mg/dl in women) | 23 | 16 | 7 | 2 | 1 | 1 | 8.861 | 0.0029 (vs) |
| SBP (≥ 130 mm Hg) | 25 | 20 | 5 | 2 | 2 | 0 | 10.208 | 0.0014 (vs) |
| DBP (≥ 85 mm Hg) | 12 | 10 | 2 | 0 | 0 | 0 | 6.585 | 0.0103 (s) |
| FBS (≥ 100 mg/dl) | 17 | 12 | 5 | 3 | 1 | 2 | 3.551 | 0.0595 (ns) |
| LDL (≥ 100 mg/dl) | 16 | 9 | 7 | 0 | 0 | 0 | 9.076 | 0.0026 (vs) |
| Dyslipidemia | 36 | 24 | 12 | 3 | 1 | 2 | 16.226 | 0.0001 (es) |
| MetS (IDF criteria) | 30 | 24 | 6 | 0 | 0 | 0 | 19.286 | 0.0001 (es) |
| MetS (NCEP ATP III criteria) | 14 | 11 | 3 | 0 | 0 | 0 | 7.810 | 0.0052 (vs) |
Differences in the prevalence between cases and controls were tested by chi-square tests with bi-variate test for statistical significance.
Discussion
COPD is a major cause of morbidity and mortality worldwide and is likely to be the third leading cause of death by the year 2020 [8]. According to the GOLD criteria, COPD is divided into four stages depending upon the severity of symptoms and spirometric findings [Table/Fig-1] [9]. Besides the combination of frequent symptoms such as cough, sputum production, and progressive exertional breathlessness, COPD has fair deed of published data on the significant extra pulmonary manifestations [10] such as metabolic disorders (type 2 diabetes mellitus, MetS, dyslipidemia, cachexia, obesity), musculo-skeletal (skeletal muscle wasting, osteopenia and steoporosis), cardiovascular disease (ischemic heart disease, hypertension, pulmonary hypertension, corpulmonale), cancer (small cell and non small cell cancer lung cancer), obstructive sleep apnea, and psychiatric illness (depression and anxiety disorders).
Over the last couple of decades, studies had shown significant relationship of MetS to COPD and several proposed pathogenic mechanisms explaining MetS in COPD are as [10,11]:
Systemic inflammation- It is a more authoritative pathophy-siological mechanism (spill over hypothesis). There is a spill over of peripheral lung inflammation into systemic circulation resulting in increased level of various inflammatory markers (IL-1β, IL-6, IL-8, and TNF-α). Thus, these systemic inflammatory markers are responsible to develop various co-morbidities in COPD patients;
Adipose tissue inflammation- it is one of the important contributing factors for systematic inflammation. Decreased unit blood supply of adipose tissue mass and insufficient oxygenation due to poor neovascularisation leads to relative tissue hypoxia and increased inflammatory response. Inflammation of adipose tissue is related to adverse effect on insulin signalling pathways;
Physical inactivity- As COPD progresses beyond the GOLD stages II, the physical activities decrease, and which can lead to weight gain and obesity. The relationship between physical inactivity and systemic inflammation has been observed, thus predisposing to develop Mets;
Effect of steroid- The use of steroid either in inhaled or oral form is frequent in COPD patients which is important contributing factor to produce different parameters of MetS;
Hypogonadism- Longitudinal studies have established that hypogonadism is a risk factor of MetS. Low testosterone level causes diminished energy level, muscle and bone mass. Hypoxia, hypercapnea and use of steroids are three possible causes of hypogonadism in COPD patients.
A conclusion of many studies done in different parts of world has shown a prevalence of MetS in COPD as 25.6% to 60.9% [10,12,13]. The present study demonstrated MetS in COPD as 30 (33.33%) and frequency of its component such as abdominal obesity, systolic blood pressure, diastolic blood pressure, elevated triglyceride, reduced HDL-c and elevated fasting glucose respectively was 78.89%, 26.67%, 13.33%, 20%, 25.56% and 18.78% respectively. Some studies have found that obesity is more common in COPD as compared to the general population [14]. A study conducted in Netherlands on 317 subjects showed 18% overall prevalence of obesity which was more in subjects with mild to moderate COPD (stage I and II) [15]. A meta-analysis of 22 studies concluded that patients with a lower BMI had a higher mortality rate when compared with normal BMI subjects while overweight and obese subjects had a lower risk of mortality [16]. So obesity in COPD is referred as “Reverse Epidemiology of Obesity” [17]. Hypertension is well recognized in COPD and its possible patho mechanism are hypoxia related vasoconstriction, free radical injury, endothelial dysfunction, and arterial stiffness [17,18]. Many large studies have demonstrated incidence of hypertension from 6% to 53% [10,19].
A study had concluded that reduced lung function is an important risk factor for the development of diabetes in COPD [20]. The association of COPD with diabetes is being increasingly recognized. It is demonstrated that approximately 3% to 12% subjects with COPD had diabetes [21]. On other hand, Diabetes mellitus is known for widespread hormonal, metabolic, and microvascular abnormalities which leads to disturbances of the function of many organ systems. Chronic hyperglycaemia causes non-enzymatic glycosylation of proteins such as collagen, elastin etc., leading to basement membrane thickening and microangiopathy. Due to micrangiopathy in alveoli, lung volumes and capacities restrict [22-24]. Most of the studies showed inconclusive pattern of dyslipidemia in COPD patient. The present study had shown 40% cases of dyslipidemia in COPD patients. The finding of dyslipidemia i.e, elevated TG and decreased HDL level were similar with many previous studies [25,26]. In contrast, many studies have revealed elevated HDL [2,5,27]. Elevated LDL was also reported in this study, favoured by a south Indian study [28]. The findings of dyslipidemia in present study are different from many studies which might be explained by the difference in lifestyle and socioeconomic status of the two populations.
Limitation
Relative small sample size was limitation of study. Further studies would be needed using a case control methodology and with a longitudinal design to determine whether there is actually an independent association between COPD and Cardiovascular Disease.
Conclusion
The findings of this study showed significant association of MetS in COPD. MetS has potential risk for cardiovascular disease in these patients. Therefore, there should be a comprehensive medical care approach for COPD patients to adequately assess and address the various components of MetS. Timely detection and management of MetS might be definitely helpful to lower morbidity and mortality rate of cardiovascular disease and its consequences.
Waist Circumference (WC), Triglycerides (TG), HDL cholesterol (HDL), Systolic BP (SBP), Diastolic BP (DBP), Fasting Blood Glucose (FBS), Metabolic Syndrome (MetS). Mean and standard deviation were computed for all continuous variables and comparison was done using unpaired t-test.
Differences in the prevalence between cases and controls were tested by chi-square tests with bi-variate test for statistical significance.
[1]. Global Strategy for the Diagnosis, Management and Prevention of COPD Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016 Accessed on Nov 21 2016www.goldcopd.org [Google Scholar]
[2]. Hosny H, Abdel-Hafiz H, Moussa H, Soliman A, Metabolic syndrome and systemic inflammation in patients with chronic obstructive pulmonary diseaseEgyptian Journal of Chest Diseases and Tuberculosis 2013 62(1):85-89. [Google Scholar]
[3]. McKay AJ, Mahesh PA, Fordham JZ, Majeed A, Prevalence of COPD in India: A systematic reviewPrim Care Respir J 2012 21:313-21. [Google Scholar]
[4]. Murali Mohan BV, Sen T, Ranganath R, Systemic manifestations of COPDJ Assoc Physicians India 2012 60(Suppl 44-7) [Google Scholar]
[5]. Lazovic B, Stajic Z, Mazic S, Đelić M, Prevalence of metabolic syndrome in patients suffered from chronic obstructive pulmonary diseaseTimok Medical Gazettes 2012 37(4):229-32. [Google Scholar]
[6]. International diabetes federation (IDF). The IDF consensus worldwide definition of the metabolic syndrome 2006 [Google Scholar]
[7]. Redelmeier DA, Tan SH, Booth GL, The treatment of unrelated disorders in patients with chronic medical diseasesN Engl J Med 1998 338:1516-20. [Google Scholar]
[8]. Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, BOLD Collaborative Research GroupInternational variation in the prevalence of COPD (the BOLD Study): A population-based prevalence studyLancet 2007 370:741-50. [Google Scholar]
[9]. Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Global Initiative For Chronic Obstructive Lung DiseaseGlobal Strategy For The Diagnosis, Management, And Prevention Of Chronic Obstructive Pulmonary Disease: GOLD Executive SummaryAm J Respir Crit Care Med 2007 176:532-55. [Google Scholar]
[10]. Naik D, Joshi A, Paul TV, Thomas N, Chronic obstructive pulmonary disease and the metabolic syndrome: Consequences of a dual threatIndian J Endocr Metab 2014 18:608-16. [Google Scholar]
[11]. Barnes PJ, Chronic obstructive pulmonary disease: Effects beyond the lungsPLoS Med 2010 7:e1000220 [Google Scholar]
[12]. Park BH, Park MS, Chang J, Kim SK, Kang YA, Jung JY, Chronic obstructive pulmonary disease and metabolic syndrome: A nationwide survey in KoreaInt J Tuberc Lung Dis 2012 16:694-700. [Google Scholar]
[13]. Díez-Manglano J, Barquero-Romero J, Almagro P, Cabrera FJ, LópezGarcía F, Montero L, Working Group on COPD, Spanish Society of Internal Medicine. COPD patients with and without metabolic syndrome: Clinical and functional differencesIntern Emerg Med 2014 9:419-25. [Google Scholar]
[14]. García-Olmos L, Alberquilla A, Ayala V, García-Sagredo P, Morales L, Carmona M, Comorbidity in patients with chronic obstructive pulmonary disease in family practice: A cross sectional studyBMC Fam Pract 2013 14:11 [Google Scholar]
[15]. Steuten LM, Creutzberg EC, Vrijhoef HJ, Wouters EF, COPD as a multicomponent disease: Inventory of dyspnoea, underweight, obesity and fat free mass depletion in primary carePrim Care Respir J 2006 15:84-91. [Google Scholar]
[16]. Cao C, Wang R, Wang J, Bunjhoo H, Xu Y, Xiong W, Body mass index and mortality in chronic obstructive pulmonary disease: A meta-analysisPLoS One 2012 7:e43892 [Google Scholar]
[17]. Wang Y, Bai C, Wang X, COPD-associated vascular pathology: A future targeting areaExpert Rev Respir Med 2008 2:297-99. [Google Scholar]
[18]. Maclay JD, McAllister DA, Mills NL, Paterson FP, Ludlam CA, Drost EM, Vascular dysfunction in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med 2009 180:513-20. [Google Scholar]
[19]. Fumagalli G, Fabiani F, Forte S, Napolitano M, Marinelli P, Palange P, INDACO project: A pilot study on incidence of comorbidities in COPD patients referred to pneumology unitsMultidiscip Respir Med 2013 8:28 [Google Scholar]
[20]. Engström G, Janzon L, Risk of developing diabetes is inversely related to lung function: A population-based cohort studyDiabet Med 2002 19:167-70. [Google Scholar]
[21]. Sidney S, Sorel M, Quesenberry CP, JrDeLuise C, Lanes S, Eisner MD, COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care ProgramChest 2005 128:2068-75. [Google Scholar]
[22]. Singh J, Gupta KK, Himanshu D, Patel ML, Mishra A, Kant S, Study of pulmonary functions in patients with type 2 diabetes mellitus and its correlation with microvascular complicationsInternational Journal of Medicine and Medical Sciences 2014 47:1558-62. [Google Scholar]
[23]. Singh J, Gupta KK, Himanshu D, Dinkar A, Atam V, Kant S, To study the effect of glycemic control and duration of disease on pulmonary function tests and diffusion capacity in type 2 diabetes mellitusInt J Res Med Sci 2015 3:224-28. [Google Scholar]
[24]. Singh J, Gupta KK, Himanshu D, Dinkar A, Atam V, Pulmonary function tests and diffusion capacity in type 2 diabetes and their possible correlation with proteinuriaJournal of Medical Science and Clinical Research 2014 2:3091-98. [Google Scholar]
[25]. Acharyya A, Shahajahan MD, Mesbah FB, Dey SK, Ali L, Association of metabolic syndrome with chronic obstructive pulmonary disease in an Indian populationLung India 2016 33(4):385-90. [Google Scholar]
[26]. Dave L, Garde S, Ansari OA, Shrivastava N, Sharma VK, A Study of association between metabolic syndrome and COPDJournal of Evolution of Medical and Dental Sciences 2014 3(22):6183-88. [Google Scholar]
[27]. Tisi GM, Conrique A, Barrett-Connor E, Grundy SM, Increased high density lipoprotein cholesterol in obstructive pulmonary disease (predominant emphysematous type)Metabolism 1981 30:340-46. [Google Scholar]
[28]. Niranjan MR, Dadapeer K, Rashmi K, Lipoprotein profile in patients with chronic obstructive pulmonary disease in a tertiary care hospital in South IndiaJ Clin Diagn Res 2011 5:990-93. [Google Scholar]