Recurrent Optic Nerve Pilocytic Astrocytoma: A Rare Case
Sudha Girish Menon1, Vuppalapati Nishant Janardhana Raju2, Sulatha V Bhandary3, Krishna Rao Addoor4
1 Assistant Professor, Department of Ophthalmology, Kasturba Medical College, Manipal, Karnataka, India.
2 Junior Resident, Department of Ophthalmology, Kasturba Medical College, Manipal, Karnataka, India.
3 Professor, Department of Ophthalmology, Kasturba Medical College, Manipal, Karnataka, India.
4 Professor, Department of Ophthalmology, Kasturba Medical College, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vuppalapati Nishant Janardhana Raju, Junior Resident, Department of Ophthalmology, Kasturba Medical College, Manipal, Udupi, Karnataka-576104, India.
E-mail: nishant.janardhan@gmail.com
Pilocytic astrocytoma is a low grade glioma that affects mostly children and young adults and can occur anywhere in the central nervous system. Pilocytic astrocytoma of the optic nerve is an equally indolent subtype that is often associated with Neurofibromatosis Type I (NFI). A 40-year-old male presented with left sided axial proptosis and exposure keratopathy. MRI revealed a mass in left proximal orbit, extending posteriorly abutting the chiasma and the right optic nerve on MRI. Enucleation of the left eye along with near total excision of intracranial part of the mass was performed. Histopathology report was suggestive of pilocytic astrocytoma (WHO Grade I). Interestingly, his records showed evidence of surgery for removal of the optic nerve pilocytic astrocytoma twice (27 years and six years ago). We hereby, present an unusual case of recurrent pilocytic astrocytoma of the optic nerve in absence of NFI.
Complete loss of vision, Enucleation, Optic nerve glioma
Case Report
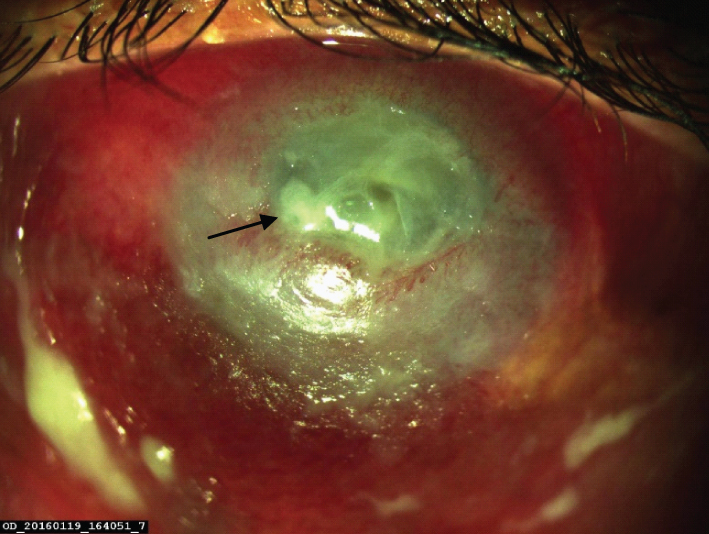
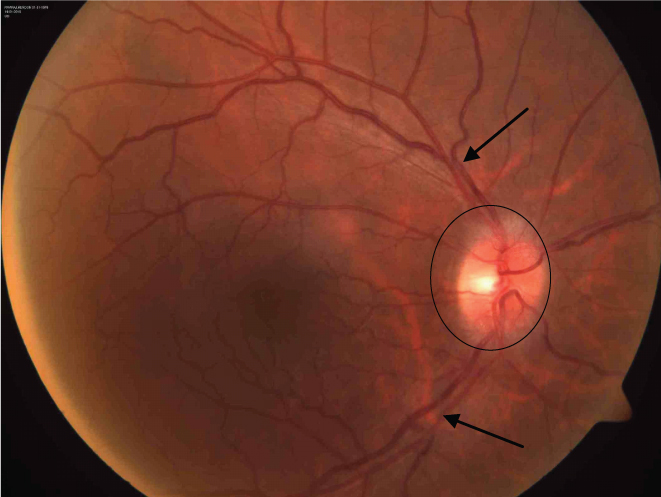
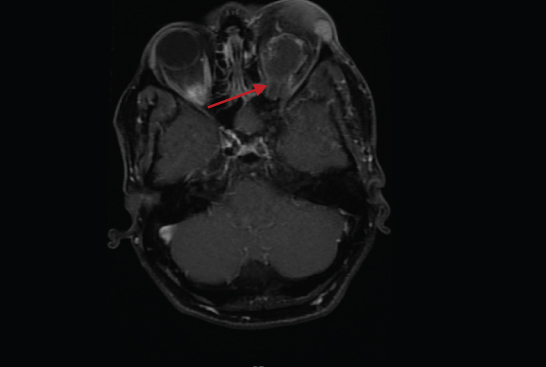
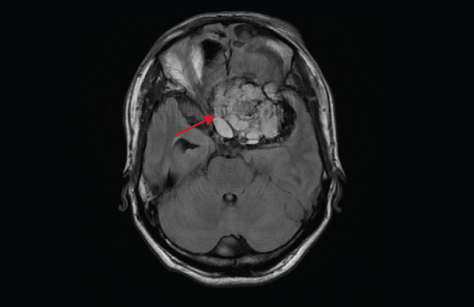
A 40-year-old male presented to the Ophthalmology Outpatient Department with left eye progressive, painful proptosis and complete loss of vision since 10 days. He had been operated twice, 27 years and six years back for optic nerve pilocytic astrocytoma. Neither patient nor previous records reveal prior history of radiotherapy. On examination, patient denied perception of light in the left eye, showing severe axial proptosis (Hertel exophthalmometry showed 5 mm of proptosis) with the limitation of motility in all gaze directions and severe exposure keratopathy causing circumciliary congestion, diffuse corneal keratinization with central and paracentral thinning and ulceration [Table/Fig-1]. Right eye visual acuity was 6/6, with the normal anterior segment and the fundus examination revealed oedema of the optic disc [Table/Fig-2]. The clinical picture was suggestive of recurrence of optic nerve pilocytic astrocytoma with raised intracranial pressure. Blood counts were normal. MRI orbit revealed left axial exophthalmos with mass in left proximal orbit, hypo to isointense on T1 [Table/Fig-3], hyperintense on T2. MRI cranium showed a 5.5 cm x 4.5 cm x 5 cm mass distal to left orbital apex abutting the chiasma and the right optic nerve, displacing carotids and cavernous sinus along with postoperative fibrotic changes [Table/Fig-4]. Inflammatory orbital pseudotumour, thyroid orbitopathy, infective orbital inflammations were considered as differential diagnosis keeping painful axial proptosis in mind. Considering painful blind eye, enucleation of the left eye was performed. The neurosurgery team through left frontal craniotomy performed near total excision of intracranial part of the tumour with left orbital roof excision and orbital decompression of tumour. The whole affected left optic nerve was removed along with Bronson ray exteriorization of frontal sinus with pericranium. Histopathology report was suggestive of pilocytic astrocytoma (WHO Grade I). Patient was put on tablet phenytoin 100 mg TID, tablet dexamethasone 4 mg OD for two weeks, tablet pantaprazole 40 mg OD for two weeks, tablet diclofenac sodium 75 mg BD for one week and eye ointment ciprofloxacin TID for two weeks. On follow up, one month after enucleation and near total excision of tumour, left eye socket was healthy and left orbital swelling resolved (tablet phenytoin 100 mg TID was continued, rest medications were discontinued). The patient was then advised yearly follow up.
Clinical photograph of left eye (OS) showing axial proptosis causing severe exposure keratopathy with corneal ulceration (arrow).
Fundus photograph of right eye (OD) showing optic disc oedema (circle) with dilated and tortuous veins (arrows).
MRI orbit showing left axial exophthalmos with mass in left proximal orbit, hypo to isointense on T1 (arrow).
MRI cranium showing 5.5 cm x 4.5 cm x 5 cm mass appearing hyperintense on T2 distal to left orbital apex abutting the chiasma and the right optic nerve, displacing carotids and cavernous sinus along with postoperative fibrotic changes (arrow).
Discussion
Pilocytic astrocytomas comprise 1.5%–3.5% of all orbital tumours and 66% of all optic nerve tumours [1]. Majority of optic pathway pilocytic astrocytomas (75%) occur in children of less than 12 years of age. The most common site of pilocytic astrocytoma is optic nerve in children and optic chiasm in young adults [2]. Pilocytic astrocytoma is well documented to be associated with NFI. Patients with NFI are more prone to develop pilocytic astrocytoma, characteristically involving the optic nerve or chiasm. Pilocytic astrocytoma accounts up to 15%–21% of all NFI patients. Optic pathway pilocytic astrocytoma without the features of NFI is a rare entity [3].
A study conducted by Czyzyk E et al., showed that clinical presentation in patients who presented optic pathway gliomas as sporadic tumours is more severe than in those associated with NFI [3]. Similarly, our patient too did not have NFI and the clinical picture was severe with loss of vision, proptosis, features of raised intracranial pressure (vomiting, papilloedema) and multiple recurrences. The time gap between primary diagnosis and first recurrence is longer for patients with NF1 association, when compared to patients who do not have NF1 association [4]. But in our case, optic nerve pilocytic astrocytoma did not have any NFI association, but time gap between primary diagnosis and recurrences was long (21 years and 6 years). A study stated that recurrence rates are low with gross total resection when compared to partial resection. Recurrences are more common within four years of the primary surgery [5]. Interestingly in our case during its first occurrence, it was subjected to gross total resection. But 21 years later we observed recurrence.
A study suggested that optic pathway gliomas patients, who are symptomatically stable, are to be managed conservatively with imaging and regular follow ups. On the flip side, patients who have radical course with the evidence of hydrocephalus are to be managed by surgical resection for the tumours if located in the optic nerve and radiation therapy if optic chiasm was involved [6]. In our case, the initial diagnosis was made when the patient was 13-year-old. The tumour was restricted only to the optic nerve and was treated by tumour decompression via transforaminal approach. Twenty one years later the tumour recurred, which is a prolonged period for tumour recurrence for which repeat decompression was carried out via transcranial approach. Six years later the second tumour recurrence occurred, which is a very rare phenomenon. During the second recurrence, the presentation was found to be aggressive causing severe proptosis with exposure keratopathy and no perception of light in the left eye resulting in the painful blind eye. MRI revealed tumour involvement up to the chiasma displacing the carotids and the cavernous sinus.
Conclusion
Optic nerve pilocytic astrocytoma and NF1 share a very close association, but in our case patient had no features of NF1. Recurrent optic nerve pilocytic astrocytoma with remission period of 21 years, without NF1 association, is a very rare entity. In cases of optic nerve pilocytic astrocytoma, thorough workup, timely intervention and imaging with regular reviews avoids visual deprivation.
[1]. Dutton JJ, Gliomas of the anterior visual pathwaySurvey of Ophthalmology 1994 38(5):427-52. [Google Scholar]
[2]. Alvord Jr EC, Lofton S, Gliomas of the optic nerve or chiasm: outcome by patients’ age, tumour site, and treatmentJournal of Neurosurgery 1988 68(1):85-98. [Google Scholar]
[3]. Czyzyk E, Jóźwiak S, Roszkowski M, Schwartz RA, Optic pathway gliomas in children with and without neurofibromatosis 1Journal of Child Neurology 2003 18(7):471-78. [Google Scholar]
[4]. Gutmann DH, Hedrick NM, Li J, Nagarajan R, Perry A, Watson MA, Comparative gene expression profile analysis of neurofibromatosis 1-associated and sporadic pilocytic astrocytomasCancer Research 2002 62(7):2085-91. [Google Scholar]
[5]. Bowers DC, Krause TP, Aronson LJ, Barzi A, Burger PC, Carson BS, Second surgery for recurrent pilocytic astrocytoma in childrenPediatric Neurosurgery 2001 34(5):229-34. [Google Scholar]
[6]. Colosimo C, Cerase A, Maira G, Regression after biopsy of a pilocytic opticochiasmatic astrocytoma in a young adult without neurofibromatosisNeuroradiology 2000 42(5):352-56. [Google Scholar]