An Unusual Presentation of B Cell Acute Lymphoblastic Leukaemia in a Child
Pushpa Gurudas Kini1, Sandeep Kumar2, Adel Moideen3, Adharsh Tulasidhar Narain4, Akkineni Veena5
1 Professor, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Assistant Professor, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Senior Resident, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Senior Resident, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Junior Resident, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sandeep Kumar, Assistant Professor, Department of Paediatrics, Kasturba Medical College, Manipal University, Manipal-576104, Karnataka, India.
E-mail: bksandydoc@gmail.com
Hepatosplenomegaly, Leukaemia cutis, Skin infiltration
Acute Lymphoblastic Leukaemia (ALL) is one of the most common haematological malignancies seen in children. Children with acute leukaemia mostly present with pallor, bone pain, bleeding manifestations and hepatosplenomegaly. Skin infiltration is common in myeloid leukaemia/ lymphoma and rarely in neuroblastoma stage IV S [1,2]. However, B cell leukaemia presenting with skin lesions is extremely rare and only limited case reports are available [3]. We report an adolescent girl presenting with nodular skin lesions and was diagnosed to have B cell ALL.
A 13-year-old girl presented with multiple dark hyper pigmented skin nodules on the limbs, face, trunk and abdomen noticed since two months. There was no history of bone pain or skin bleeds. The family history was not significant. Growth and development was normal. On examination, the height was 145 cm (between 3rd and 15th centile) and weight was 28 kg; body mass index 13.3 Kg/m2) (3rd centile for age). Vitals were stable. There were multiple dark, hyper pigmented nodular lesions measuring 1 cm-1.5 cm present over limbs, face and trunk [Table/Fig-1]. Pallor was present in the lower palpebral conjunctiva and oral mucosa. There was no lymphadenopathy, bony tenderness or skin bleeds. Except for hepatosplenomegaly, systemic examination was unremarkable.
Clinical photograph showing multiple hyperpigmented nodular lesions over the face and trunk.

Investigations revealed haemoglobin of 7 g/dL, total leukocyte count of 4300 cells/cumm (neutrophils 45%, lymphocytes 49%, monocyte 6%) and platelet count of 1.4 lacs/cumm. There were no blasts or abnormal cells in the peripheral smear. Serum Lactate Dehydrogenase (LDH) level was 1210 IU/L. In the presence of anaemia, hepatomegaly and nodular skin lesions a provisional diagnosis of acute leukaemia was considered.
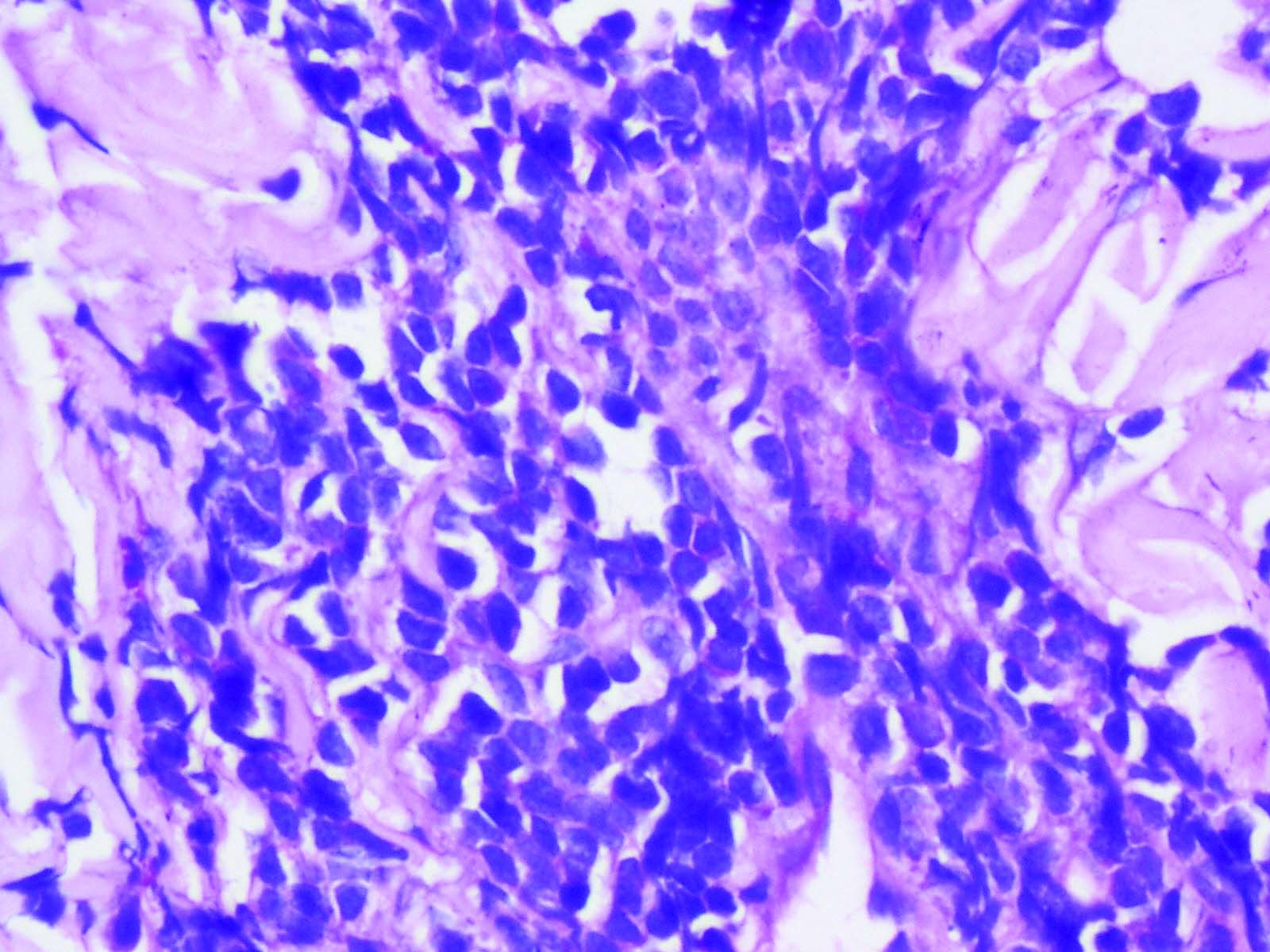
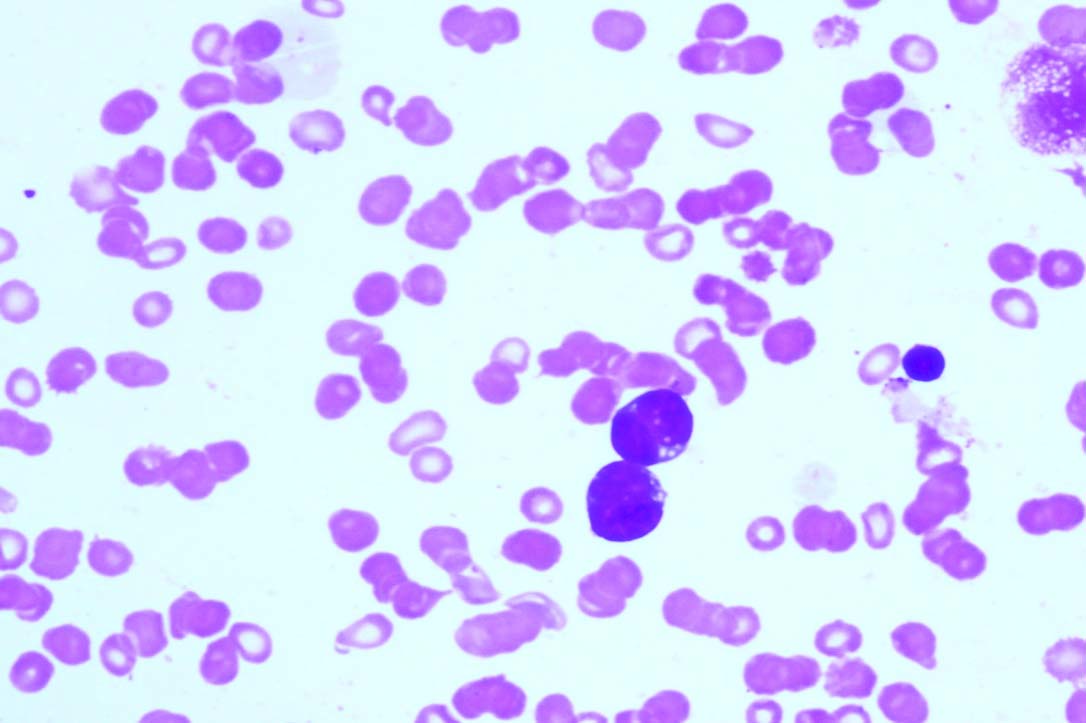
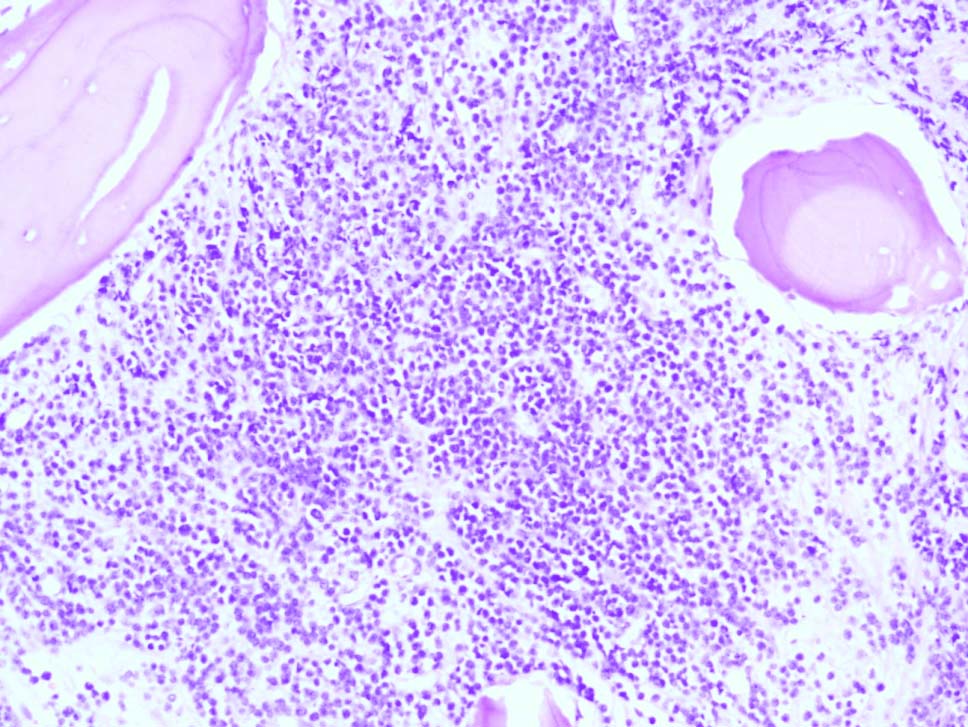
Punch biopsy from nodular skin over back revealed infiltration of diffuse sheets and nests of atypical lymphoid cells with foci of karyorrhexis and scanty cytoplasm suggestive of high grade lymphoma/leukaemia [Table/Fig-2]. Immunohistochemistry showed CD20 positivity with high Ki67 index (98%). Bone marrow aspiration and biopsy subsequently done revealed acute lymphoblastic leukaemia [Table/Fig-3,4]. Flow cytometry confirmed the diagnosis of B cell ALL. She was started on chemotherapy as per Hunger protocol, consisting of prednisolone, doxorubicin, vincristine and L-asparaginase along with weekly intrathecal methotrexate [4]. Skin lesions showed regression within one month. Bone marrow study done during the post induction phase showed remission. Repeat punch biopsy of the skin from the back was normal.
Skin biopsy showing infiltration of diffuse sheets and nests of atypical lymphoid cells (H&E; magnification x40).
Bone marrow aspiration picture showing lymphoblasts (Leishman stain, magnification x40).
Bone marrow biopsy picture showing diffuse infiltration of lymphoblasts (H&E; magnification x20).
Leukaemia Cutis (LC) is the term used to describe the cutaneous infiltration of neoplastic leukocytes or their precursors into the epidermis, the dermis, or the subcutis, resulting in clinically identifiable skin lesions [5,6]. It can occur in any type of leukaemia. It is more commonly seen in acute monocytic, myelomonocytic and the T-cell type of leukaemia. The incidence of LC varies from 2%-3% [5]. Children with LC commonly have concomitant systemic leukaemia, but rarely cutaneous involvement precedes marrow involvement. LC may present in variable forms, papules or nodules being the most frequent lesions, followed by infiltrated plaques, generalized cutaneous eruption and erythroderma [6]. LC has to be differentiated from nonspecific cutaneous conditions associated with leukaemia such as petechiae, purpura, and leucocytoclastic vasculitis. Prompt diagnosis can be ascertained by the skin biopsy of suspicious lesions and confirmed by bone marrow study. The course and prognosis of leukaemic patients presenting with LC is similar to those who present without LC. In a study conducted in Austria leukaemic patients who presented with LC had shorter duration of remission and high serum LDH levels [7].
LC is a differential diagnosis in a child presenting with generalized nodular skin eruptions. This case report highlights the rarity of the clinical presentation of acute leukaemia and skin lesion as a marker for early diagnosis of ALL. In this case, the punch biopsy of the skin lesion provided the early diagnosis of acute leukaemia which was later confirmed by bone marrow biopsy. Thus, to conclude, metastatic skin lesions are common in myeloid leukaemia, neuroblastoma and lymphoma and are unusual in acute lymphoid leukaemia. The biopsy form these lesions help to clinch the diagnosis.
[1]. Cho-Vega JH, Medeiros LJ, Prieto VG, Vega F, Leukaemia cutisAm J Clin Pathol 2008 129(1):130-42. [Google Scholar]
[2]. Schleiermacher G, Rubie H, Hartmann O, Bergeron C, Chastagner P, Mechinaud F, Treatment of stage 4s neuroblastoma – report of 10 years’ experience of the French Society of Paediatric Oncology (SFOP)British Journal of Cancer 2003 89(3):470-76. [Google Scholar]
[3]. Joshi K, Panchal H, Parikh S, Modi G, Talele A, Anand A, Aleukemic leukaemia cutis presenting as a sole sign of relapsed paediatric acute lymphoblastic leukaemiaIndian J Hematol Blood Transfus 2016 32:46 [Google Scholar]
[4]. Hunger SP, Lu X, Devidas M, Camitta BM, Gaynon PS, Winick NJ, Improved survival for children and adolescents from 1990-2005: a report from the children’s oncology groupJ Clin Oncol 2012 30:1663-69. [Google Scholar]
[5]. Longacre TA, Smoller BR, Leukaemia cutis. Analysis of 50 biopsy-proven cases with an emphasis on occurrence in myelodysplastic syndromesAm J Clin Pathol 1993 100(3):276-84. [Google Scholar]
[6]. Rao AG, Danturty I, Leukaemia cutisIndian Journal of Dermatology 2012 57(6):504 [Google Scholar]
[7]. Agis H, Weltermann A, Fonatsch C, Haas O, Mitterbauer G, Mullauer L, A comparative study on demographic, hematological, and cytogenetic findings and prognosis in acute myeloid leukaemia with and without leukaemia cutisAnn Hematol 2002 81(2):90-95. [Google Scholar]