Increase in heart rate and blood pressure in response to pneumoperitoneum produced during laparoscopic cholecystectomy is a challenging situation for a practising anaesthesiologist [1,2]. Without adequate control of sympathetic response there is a chance of increase in morbidity of the patient during the perioperative period hampering the speedy recovery of the patient.
Over the years, many drugs have been used to control this sympathetic response unique only to laparoscopic surgeries. Use of propofol, fentanyl, esmolol and midazolam has been tried with varying degree of success [3,4]. Dexmedetomidine, a highly selective α2 receptor agonist compared to α1 receptor (1620:1) having sedative and analgesic properties seems to be apt enough to control this sympathetic response as well as provide a stable haemodynamics during extubation and in the postoperative period. Activation of α2 receptors in the locus coeruleus of the brain stem reduces the central sympathetic output and increases the firing of the inhibitory neurons. It does this by inhibiting the release of catecholamine and vasopressin [5-7] thereby, producing its anxiolytic sedative and analgesic effect.
Propofol a 2-6 diisopropylphenol has high lipid solubility, which allows for a rapid induction and recovery from anaesthesia, as well as good haemodynamic maintenance when used during the intraoperative period [8]. It produces its anaesthetic effect by positive regulation of GABA, an inhibitory neurotransmitter through ligand gated GABA a receptors. The result is decrease in cardiac output with little or no change in heart rate.
We aimed to compare the effectiveness of dexmedetomidine in attenuating the haemodynamic response to pneumoperitoneum using only the maintenance dose (0.2-0.7 μg/kg/hr) with that of propofol (1.5-4.5 mg/kg/hr) with both drugs being used in infusion form. Our research hypothesis postulates that using dexmedetomidine in maintenance dose is sufficient to ensure good haemodynamic stability in response to pneumoperitoneum in patients undergoing laparoscopic cholecystectomy.
Materials and Methods
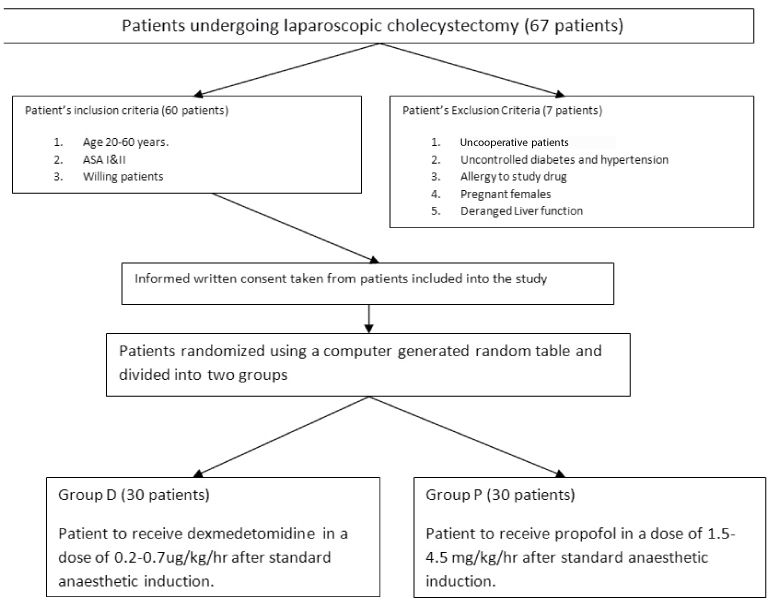
The study was a prospective randomized control trial conducted at Sikkim Manipal Institute of Medical Science, Gangtok, India, after obtaining clearance from the Institute Ethical Committee. Written informed consent was taken before enrolling the patient into the study. After thorough pre anaesthetic check up 60 ASA I and II patients undergoing laparoscopic cholecystectomy between the ages of 20 and 60 years of both sexes were randomly divided into two groups of 30 patients each using a computer generated random table, with Group D to receive dexmedetomidine infusion and Group P to receive propofol infusion. Sample size was based on previous study [9] and determined using MedCalc software version 16.2.1 with the power of the study ≥0.8. Patients with history of allergy to the study drugs, uncontrolled diabetes and hypertension, pregnant females and those with deranged liver function test were not included in the study [Table/Fig-1]. Surgical procedures lasting more than one hour due to technical difficulty were also excluded from the study.
Flowchart of inclusion/exclusion criteria.
In the operating room, a 20 G intravenous line was secured and after applying standard monitoring device (non invasive blood pressure, electro cardiogram, percent saturation of arterial oxygen, end tidal carbon dioxide monitor) and premedication with inj. glycopyrrolate 0.01 mg/kg to reduce airway secretions, all patients were induced with 3-5 mg/kg bodyweight of thiopentone and airway secured with appropriate sized endotracheal tube after giving inj. Fentanyl 2 μg/kg and inj. Succinylcholine 2 mg/kg. Anaesthesia was maintained with a mixture of oxygen and nitrous oxide in 50:50 ratio and isoflurane to maintain a minimum alveolar concentration of 1.0. Loading dose of inj. atracurium 0.5 mg/kg b.w was given soon after securing the airway and repeat dosing guided by end tidal carbon dioxide graph monitoring.
Group D received injection dexmedetomidine infusion (diluted with 24 ml of preservative free normal saline to achieve a dilution of 4 μg/ml) in a dose range of 0.2 to 0.7 μg/kg/hr while Group P received injection propofol infusion in a dose range of 1.5–4.5 mg/kg/hr. Both the drugs were started immediately after securing the airway and titrated to ensure heart rate and systolic blood pressure did not rise more than 30% of the pre pneumoperitoneum value. Titration was done by starting the drug at the midpoint of the dose range and titrated upwards or downwards depending on the increase or decrease in haemodynamic parameters respectively. The infusions of both the drugs were stopped at the end of pneumoperitoneum. Loading dose of dexmedetomidine was avoided as per the study design. The intraabdominal pressure of pneumoperitoneum was kept constant at 12 mmHg. The study drugs could not be blinded from the anaesthesiologist performing the study in view of the physical nature of the drug (propofol being white in colour) and need to adjust the dosing as per clinical response.
Haemodynamic parameters were noted just before establishing the pneumoperitoneum and every two minutes after establishing the pneumoperitoneum for the first 10 minutes and subsequently every 10 minutes till the end of pneumoperitoneum using an automated multi channel monitor. Failure to control the haemodynamic response even after the highest dose of infusion drugs was described as 30% increase in Systolic Blood Pressure (SBP) or Heart Rate (HR) to that of the pre pneumoperitoneum value and was rescued with bolus dose of inj. fentanyl 0.5 μg/kg b.w. and inj. esmolol 10 mg bolus dose respectively.
Hypotension was described as fall in SBP below 90 mmHg and treated with bolus dose of injection mephenteramine 6 mg while bradycardia was described as fall in heart rate below 50 bpm and treated with injection atropine 0.6 mg in divided dose.
After the establishment of spontaneous respiration and reversal of residual effect of muscle relaxant by inj. neostigmine 0.04 mg/kg b.w, patients were extubated once they started responding. Post extubation sedation assessment was done in each group using Ramsey’s sedation score [10] [Table/Fig-2].
Ramsey’s sedation score [10].
| Score | Description | Definition |
|---|
| 1 | Awake | Anxious and agitated or restless or both |
| 2 | Awake | Cooperative, oriented, tranquil |
| 3 | Awake | Responsive to command only |
| 4 | Asleep | Brisk response to light glabellar tap or loud auditory stimulus |
| 5 | Asleep | Sluggish response to light glabellar tap or loud auditory stimulus |
| 6 | Asleep | No response to light glabellar tap or loud auditory stimulus |
Patient sedation monitor- patent EP 1793735A2- Google patents.
Data recording was done for changes in haemodynamic parameters before and after establishment of pneumoperitoneum, Total Duration of Pneumoperitoneum (TDOP), Mean Dose of Study Drug used (MDOD), number of rescue doses of inj. fentanyl and inj. esmolol needed during the procedure, time to extubation after stopping the study drug (TTE), haemodynamic parameters on extubation, any incidence of side effects, post extubation sedation score using Ramsey’s Sedation score (PERS) and Time To Ramsey’s Score of 2 post extubation (TTRS2).
Statistical Analysis
Data was analysed using IBM SSPE statistical software version 23. Mean±SD and Student’s t-test was used for statistical analysis and comparison of age, weight, haemodynamic parameters, TDOP, MDOD,TTE, PERS and TTRS2 between the two groups with a p-value of <0.05 considered significant. Chi-square test was used for qualitative data analysis (sex, ASA grading).
Results
In terms of the demographic profile including patients’ age, sex weight and ASA status, the two groups analysed were similar with no statistically significant difference [Table/Fig-3]. The mean duration of pneumoperitoneum was 40.633±12.77 minutes in Group D while in Group P the mean duration was 42.77±10.66 minutes (p-value = 0.485) [Table/Fig-4].
| Criterion | Group D | Group P | p-value (< 0.05) |
|---|
| Age (years) | 38.733±10.18 | 43.333±13.51 | 0.142 |
| Sex (M:F) | 23:7 | 21:9 | - |
| Weight (Kgs) | 64.4±8.20 | 66.40±7.15 | 0.257 |
| ASA (i:ii) | 25:5 | 22.8 | - |
Group D= Dexmedetomidine; Group P= Propofol; ASA= American society of Anaesthesiologist: Student’s t-test was used for analysis of Age and weight with a p-value of < 0.05 considered significant while Chi-square test was used for evaluation of sex and ASA status.
Summary of various parameters analysed.
| Criterion | Group D | Group P | p-value (<0.05) |
|---|
| TDOP(mins) | 40.633±12.77 | 42.77±10.66 | 0.485 |
| MDOD | 0.504±0.09 Mg/kg/hr | 3.19±0.7 mg/kg/hr | - |
| TTE (mins) | 15.233±3.26 | 14.97±3.35 | 0.756 |
| PERS (3:4:5) | 17:9:4 | 22:7:1 | |
| TTRS2 (mins) | 14.27±5.08 | 11.33±4.54 | 0.02 (significant) |
| Hypotension | 2 | 1 | - |
| RDOF | 0 | 2 | - |
Group D= Dexmedetomidine; Group P= Propofol; TDOP: Total Duration of Pneumoperitoneum; MDOD: Mean Dose of Drug; TTE: Time to Extubation; PERS: Post Extubation Ramsey’s Sedation Score 3, 4 and 5; TTRS2 : Time to Ramsey’s score 2 post extubation, RDOF: Rescue Dose of Fentanyl. Student’s t-test was used for analysis of age, weight, TDOP, TTE and TTRS2 with a p-value of < 0.05 considered significant while Chi-square test was used for evaluation of sex of the patient, ASA grading and PERS.
Mean values of all haemodynamic parameters have been listed in the tables below [Table/Fig-5,6,7 and 8]. Heart rate prior to establishing pneumoperitoneum was statistically significant (p-value = 0.017) which could be due to avoidance of sedatives as pre-medication in the preoperative period to avoid interference with Ramsey’s sedation score in the postoperative period.
Comparison of mean heart rate between two groups.
| Criterion | Group D | Group P | p-value < 0.05) |
|---|
| Pre -op | 90.7 | 83.4 | 0.017 (significant) |
| 2 MIN | 90.2 | 84.6 | 0.069 |
| 4 MIN | 89.5 | 84.8 | 0.112 |
| 6 MIN | 88.6 | 84.4 | 0.088 |
| 8 MIN | 87.9 | 84 | 0.141 |
| 10 MIN | 88.3 | 83.7 | 0.073 |
| 20 MIN | 87.1 | 83.3 | 0.139 |
| 30 MIN | 87.2 | 83.3 | 0.153 |
| 40 MIN | 86.4 | 80.9 | 0.119 |
| 50 MIN | 82.09 | 78.8 | 0.39 |
| 60 MIN | 78.0 | 76.5 | 0.614 |
| POST OP | 87.3 | 88.9 | 0.533 |
Group D= Dexmedetomidine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Comparison of mean systolic blood pressure between two groups.
| Criterion | Group D | Group P | p-value (< 0.05) |
|---|
| Pre -op | 117.7 | 116.8 | 0.743 |
| 2 MIN | 115.9 | 118.8 | 0.278 |
| 4 MIN | 113.1 | 119.8 | 0.110 |
| 6 MIN | 117.4 | 121 | 0.148 |
| 8 MIN | 117.8 | 120.9 | 0.274 |
| 10 MIN | 116.7 | 119.4 | 0.285 |
| 20 MIN | 112.4 | 115.1 | 0.372 |
| 30 MIN | 114.1 | 114.5 | 0.89 |
| 40 MIN | 109.8 | 113.8 | 0.225 |
| 50 MIN | 109.2 | 111.57 | 0.556 |
| 60 MIN | 105.5 | 120.5 | 0.446 |
| POST OP | 125.7 | 133.2 | 0.003 (significant) |
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Comparison of mean diastolic blood pressure between two groups.
| Criterion | Group D | Group P | p-value (< 0.05) |
|---|
| Pre -op | 73.3 | 71.8 | 0.535 |
| 2 MIN | 72.9 | 73.8 | 0.751 |
| 4 MIN | 71.7 | 74.3 | 0.259 |
| 6 MIN | 73.4 | 74.4 | 0.70 |
| 8 MIN | 73.2 | 72.7 | 0.831 |
| 10 MIN | 71 | 70.5 | 0.847 |
| 20 MIN | 69.2 | 68.8 | 0.849 |
| 30 MIN | 68.8 | 68.8 | 0.997 |
| 40 MIN | 66.3 | 67 | 0.805 |
| 50 MIN | 65.18 | 65.143 | 0.991 |
| 60 MIN | 63.0 | 73.5 | 0.561 |
| POST OP | 74.4 | 76.2 | 0.413 |
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Comparison of mean MAP between the two groups.
| Criterion | Group D | Group P | p-value (<0.05) |
|---|
| Pre -op | 89.5 | 87.9 | 0.512 |
| 2 MIN | 88.9 | 90.5 | 0.510 |
| 4 MIN | 88.6 | 91.5 | 0.210 |
| 6 MIN | 89.7 | 92.1 | 0.295 |
| 8 MIN | 89.4 | 90.8 | 0.554 |
| 10 MIN | 87.7 | 89 | 0.529 |
| 20 MIN | 85.2 | 86.2 | 0.670 |
| 30 MIN | 85.2 | 86 | 0.702 |
| 40 MIN | 81.8 | 84.6 | 0.305 |
| 50 MIN | 80.64 | 82.64 | 0.572 |
| 60 MIN | 78.5 | 91.5 | 0.492 |
| POST OP | 93.1 | 97.5 | 0.052 |
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Mean systolic blood pressure in the postoperative period was significantly higher (p-value=0.003) in propofol group (133.2 mmHg) compared to dexmedetomidine group (125.7 mmHg) which suggested a better attenuation of haemodynamic parameters by dexmedetomidine compared to propofol.
Changes in rest of the haemodynamic parameters during the intraoperative period were similar in both the groups (statistically insignificant) although the decrease in heart rate was slightly more in group dexmedetomidine compared to group propofol.
In propofol group, there was an increase in heart rate and blood pressure above the baseline value in the first six minutes after establishment of pneumoperitoneum followed by gradual decline thereafter [Table/Fig-5,6 and 7]. The same pattern of change was not observed in the dexmedetomidine group with overall gradual decrease in heart rate and blood pressure throughout the intraoperative period.
The time to extubation was 15.233±3.26 minutes in dexmedetomidine group and 14.97±3.336 minutes in propofol group (statistically insignificant). However, the time to Ramsey’s score of two post extubation was statistically significant in propofol group (11.33± 4.54 minutes) compared to dexmedetomidine group (14.27±5.06 minutes) (p-value = 0.02).
The mean dose of dexmedetomidine used was 0.504± 0.09 μg/kg/hr while the mean dose of propofol used was 3.19±0.7 mg/kg/hr. The two groups could not be compared statistically due to different dosing of the study drugs. We found that it was economical to use dexmedetomidine compared to propofol as maintenance drug in the intraoperative period {Rs 77.3 for dexmedetomidine Vs Rs 146.5 for propofol (calculated using the mean dose of two drugs, mean body weight of two groups, mean duration of pneumoperitoneum and maximum retail price of the two study drugs as quoted by manufacturers)} owing to the smaller volume of dexmedetomidine required compared to propofol.
Two patients in group dexmedetomidine had fall in systolic blood pressure >30% of baseline value and was treated with single dose of inj. Mephenteramine 6 mg while in propofol group the same happened in one patient and was accordingly treated.
Two patients in group propofol required single bolus rescue dose of fentanyl 30 μg in the intra operative period during dissection of the gall bladder from the liver bed. No rescue dose of fentanyl was needed for dexmedetomidine group.
Discussion
In this study we found out that dexmedetomidine infusion in maintenance dose (0.2-0.7 μg/kg/hr) can effectively attenuate the haemodynamic parameters in response to pneumoperitoneum in patients undergoing laparoscopic cholecystectomy while avoiding the side effects of using the loading dose of dexmedetomidine such as hypotension, bradycardia and prolonged time to extubation.
In short duration, surgical procedures done under general anaesthesia, it is imperative to ensure a good haemodynamic control during the intraoperative period and smooth early extubation in order to maximise operation theatre time utilization and improve the yield. Pneumoperitoneum produced during laparoscopic cholecystectomy presents the anaesthesiologist a unique situation of high sympathetic nervous stimulation as a result of stretching of abdominal wall [1].
Dexmedetomidine, a highly selective α2 agonist has central sympatholytic and peripheral vasoconstrictive effects, as a result of which there is a dose dependent decrease in blood pressure and heart rate. It also decreases serum norepinephrine concentrations which adds to its haemodynamic effect. It blunts the sympathetic function by activating the receptors in the medullary vasomotor center thereby, decreasing the central sympathetic outflow and a reduction in blood pressure and heart rate without any side effects like respiratory depression or postoperative nausea and vomiting. There is also stimulation of parasympathetic outflow as a result of activation of receptors in the locus coeruleus of the brainstem [5-7].
A study conducted by Shah V et al., compared dexmedetomidine and propofol for haemodynamic changes and depth of anaesthesia (using BIS monitor) during laparoscopic surgery [9]. In their study dexmedetomidine was used in both loading and maintenance dose and found it to be superior to propofol for haemodynamic control. In our study, the attenuation of haemodynamic parameters was similar with both propofol and dexmedetomidine even though, the latter was used only in maintenance dose. However, since our study did not involved the use of BIS monitor, we cannot comment whether the depth of anaesthesia achieved was the similar in both the studies.
GR Manne et al., used dexmedetomidine in doses of 0.2 μg/kg/hr and 0.4 μg/kg/hr to assess its effect on haemodynamic stress response, sedation and postoperative analgesic requirement in patients undergoing laparoscopic surgeries and found that the attenuation of haemodynamic response and reduction in postoperative analgesic requirement was maximal when dexmedetomidine was used in the dose of 0.4 μg/kg/hr [11]. In our study we found that the mean dose of dexmedetomidine infusion used was 0.504±0.09 μg/kg/hr which is consistent with the findings of the above cited study.
A study conducted by Shah A et al., established the haemodynamic attenuating capability of propofol used as an infusion in the dose of 1.5-4.5 mg/kg/hr during the intraoperative period in patients undergoing laparoscopic cholecystectomy [12]. The findings of our study are similar to the one conducted by Shah A et al. The mean dose used in our study was 3.19±0.7 mg/kg/hr.
Limitation
Limitations include a small sample size and restriction of the duration of surgery to less than one hour. Further studies are required for assessing the effect of dexmedetomidine on haemodynamic parameters when the duration of laparoscopic surgery is prolonged due to technical difficulties.
Conclusion
Considering the fact that due to technological advances, laparoscopic cholecystectomy has become a very short duration surgical procedure and at the same time since the perils of pneumoperitoneum continues to challenge anaesthesiologist, use of dexmedetomidine in maintenance dose (0.2-0.7 μg/kg/hr) avoiding the loading dose will help the anaesthesiologist immensely in tackling this simple yet complicated issue.
Patient sedation monitor- patent EP 1793735A2- Google patents.
Group D= Dexmedetomidine; Group P= Propofol; ASA= American society of Anaesthesiologist: Student’s t-test was used for analysis of Age and weight with a p-value of < 0.05 considered significant while Chi-square test was used for evaluation of sex and ASA status.
Group D= Dexmedetomidine; Group P= Propofol; TDOP: Total Duration of Pneumoperitoneum; MDOD: Mean Dose of Drug; TTE: Time to Extubation; PERS: Post Extubation Ramsey’s Sedation Score 3, 4 and 5; TTRS2 : Time to Ramsey’s score 2 post extubation, RDOF: Rescue Dose of Fentanyl. Student’s t-test was used for analysis of age, weight, TDOP, TTE and TTRS2 with a p-value of < 0.05 considered significant while Chi-square test was used for evaluation of sex of the patient, ASA grading and PERS.
Group D= Dexmedetomidine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.
Group D= Dexmedetomdine Group; Group P= Propofol group; p-value = <0.05 statistically significant by student’s t-test.