Does Change in Thread Shape Influence the Pull Out Strength of Mini Implants? An In vitro Study
Aniruddh V. Yashwant1, S. Dilip2, R. Krishnaraj3, K. Ravi4
1 Senior Lecturer, Department of Orthodontics and Dentofacial Orthopaedics, Indira Gandhi Institute of Dental Sciences, Mahatma Gandhi Medical College Campus, Sri Balaji Vidyapeeth University, Pillaiyarkuppam, Puducherry, India.
2 Professor, Department of Orthodontics and Dentofacial Orthopaedics, SRM Dental College, Ramapuram, Chennai, India.
3 Professor, Department of Orthodontics and Dentofacial Orthopaedics, SRM Dental College, Ramapuram, Chennai, India.
4 Professor and Head, Department of Orthodontics and Dentofacial Orthopaedics, SRM Dental College, Ramapuram, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aniruddh V. Yashwant, Senior Lecturer, Department of Orthodontics and Dentofacial Orthopaedics, Indira Gandhi Institute of Dental Sciences, Mahatma Gandhi Medical College Campus, Sri Balaji Vidyapeeth University, Pillaiyarkuppam, Puducherry–607 402, India.
E-mail: aniruddhyashwant@yahoo.com
Introduction
Mini implants form a valuable source for absolute anchorage thereby helping in achieving ideal treatment outcome. Stability of the mini implant is one of the important factors affecting the success of mini implants. Thread shape is a critical factor in the engineering design of mini implant, which affects the primary stability.
Aim
To evaluate the effects of thread shape on the pull out strength of mini implants.
Materials and Methods
Mini implants of five different designs in thread shape (reverse buttress, buttress, 75° joint profile with flutes, trapezoidal and trapezoidal fluted) were used with 10 screws in each group. The mini implants were loaded on to the polyurethane foam block (Sawbones pacific research lab, USA) perpendicular to the surface and the pull out strength was tested using the Instrom testing machine. The control group consisted of mini implants with reverse buttress thread shape. One-way ANOVA and Tukey post-hoc tests were used to compare the pull out strength of the mini implants within as well as between the different groups.
Results
The mean in the pull out tests ranged from 13.45 N (trapezoidal) to 61 N (trapezoidal fluted). The tukey post-hoc tests showed a statistically significant difference of 34.5 N between the control group and the trapezoidal fluted group. The level of statistical significance showed p< 0.05
Conclusion
Trapezoidal fluted mini implants showed the highest pull out strength when compared to mini implants with other thread designs used in this study. Further studies with the use of Finite Element Method (FEM) and foam blocks of higher density would be required to evaluate the performance of this new thread design.
Anchorage, Stability, Trapezoidal fluted
Introduction
The term “anchorage” in orthodontics is defined as the nature and degree of resistance to displacement offered by an anatomic unit when used for effecting tooth movement [1]. Over the years, various methods have been used for achieving anchorage in orthodontics such as Begg’s differential force and anchor bends, headgears, lingual arches and the lacebacks and bendbacks in the McLaughlin, Bennett, Trevisi (MBT) philosophy. Yet, the pursuit for a true anchorage device continued over the decades. Temporary Anchorage Devices (TADs) have revolutionized the field of orthodontics in the present scenario [2,3]. The various TADs used in contemporary orthodontics include mini implants, onplants, miniplates, zygomatic implants and palatal implants. Mini implants are the most commonly used temporary anchorage devices. They show numerous advantages over other TADs such as lower cost structure, ease of insertion and removal and versatility of placement [4-8].
Stability of mini implants can be either primary or secondary. Primary or short term stability is determined by mechanical retention of the screw in bone (bone properties), engineering design and placement technique. Secondary or long term stability is determined by bone characteristics, bone turnover and by limiting micromovements. Over time, primary stability decreases and secondary stability increases. Clinical success of the mini implant is dependent upon the combination of primary and secondary stability [9-11].
The factors in the design of the mini implant, which affect its stability, are pitch of the screw threads, length, diameter, taper of the mini implant, form of the tip and surface of the thread. Various in vitro studies have shown the importance of these factors affecting the stability of mini implants [12-18]. The aim of this study was to evaluate the effects of thread shape on the pull out strength of mini implants. The research hypothesis was that changing the thread shape influences the pull out strength of mini implants.
Materials and Methods
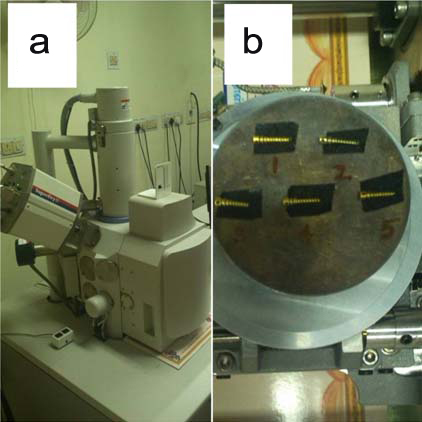
This in vitro comparative experimental study on thread design of mini implants was done at SRM dental college, Ramapuram, Chennai, India, in the year of 2014 over a period of six months. Fifty Titanium Grade V mini implants of dimension 1.5 mm x 8 mm, self-drilling type were manufactured by incorporating five different thread shapes. The mini implants to be used for this study were evaluated using Scanning Electron Microscope (SEM) at Anna University, Chennai [Table/Fig-1a,b] to check if the different thread shapes had been accurately designed by the manufacturer. The five different thread shapes of the mini implants used in this study were [Table/Fig-2a-e]:
(a) Scanning electron microscope, Anna University, Chennai; (b) Mini implants mounted on SEM platform for evaluation of thread design.
(a) SEM view of reverse buttress thread design; (b) SEM view of buttress thread design; (c) SEM view of 75° joint profile with flutes thread design; (d) SEM view of trapezoidal thread design; (e) SEM view of trapezoidal fluted thread design.
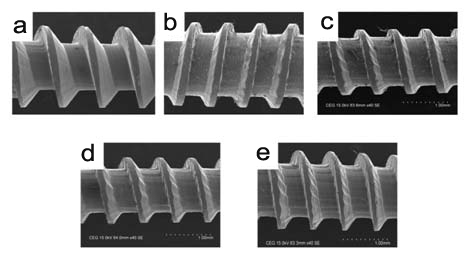
Reverse buttress [Table/Fig-2a]
Buttress [Table/Fig-2b]
75° joint profile with flutes [Table/Fig-2c]
Trapezoidal [Table/Fig-2d]
Trapezoidal fluted [Table/Fig-2e]
The five groups of different thread shapes with 10 mini implants in each group were then subjected to pull out test. The control group consisted of mini implants with reverse buttress thread shape [19]. To ensure the uniformity of evaluating the pull out strength, a synthetic polyurethane foam block was used (procured from Sawbones Pacific Research Laboratories, Washington, USA). The specifications of the block were dimensions of 13 cm x 18 cm x 4 cm and density of 0.20 gm/cc (12.5 pcf). All the mini implants were self drilled on to the polyurethane foam block perpendicular to the surface at 1 cm intervals [Table/Fig-3a].
(a) Self drilling of the mini implants onto the polyurethane foam block at 1 cm intervals; (b) Mini implant secured on to the loading arm of Instrom machine using ligature wire (0.018”); (c) Unloading/pull out of the mini screw from the synthetic foam block when vertical force is applied; (d) Graph obtained from the auto instrument software (load in kN vs sisplacement in mm).
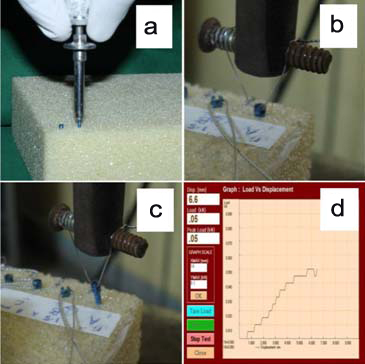
The pull out test for the mini implants was performed at Metmech laboratories, Chennai. The pull out test is one of the invasive methods used to evaluate mini implant stability, design of dental implants and also to test the mechanical interface between the implant and the bone [20-22]. It is the force required to pull out the mini implant from the bone/artificial foam block when applied vertical to the surface of the bone/artificial foam block. The polyurethane foam block used in this study was loaded and clamped on to the Instrom testing machine. The loading arm was oriented perpendicular to the screw head to apply a pull out force parallel to the long axis of the mini implant. The mini implants were secured to the loading arm using ligature wires (0.018”) of 5 cm length [Table/Fig-3b] to eliminate any bias out of using varying lengths of ligature wires which may influence the pull out force values [23]. The loading arm was then moved at a rate of 10 mm per minute to facilitate pull out of the mini implants [19]. In this study, pullout strength was measured as the peak force recorded in the auto Instrument software when the mini-implant dislodged from the synthetic bone support [Table/Fig-3c].
This was repeated for each of the mini implant and with unloading of each mini implant, a graph (Load in KN vs Displacement in mm) was simultaneously plotted using auto Instrument software [Table/Fig-3d].
Statistical Analysis
Descriptive statistics involved the calculation of mean, standard deviation and standard error of mean for the pull out tests [Table/Fig-4]. One-way ANOVA and Tukey post-hoc tests were used to compare the pull out strength of the mini implants within as well as between the different groups [Table/Fig-5]. The level of significance was p<0.05. The statistical analysis was done using Statistica software (StatSoft, Inc. USA).
Mean, standard deviations, standard error of mean values of pull out tests (ANOVA applied).
| S.No | Type of Thread Design of Mini implant | N | Mean | Std. Deviation | Std. Error of Mean | p-value |
|---|
| 1 | Reverse buttress | 10 | 27.40 | 3.273 | 1.035 | <0.001* |
| 2 | Buttress | 10 | 26.50 | 2.321 | 0.734 |
| 3 | 75° joint profile | 10 | 26.70 | 5.334 | 1.687 |
| 4 | Trapezoidal | 10 | 13.45 | 2.967 | 0.938 |
| 5 | Trapezoidal fluted | 10 | 61.00 | 8.097 | 2.560 |
denotes significant level of significance
Means for groups in homogeneous subsets (Tukey post hoc test).
| Group | N | Subset for alpha = 0.05 |
|---|
| 1 | 2 | 3 |
|---|
| 4 | 10 | 13.45 | | |
| 2 | 10 | | 26.50 | |
| 3 | 10 | | 26.70 | |
| 1 | 10 | | 27.40 | |
| 5 | 10 | | | 61.00 |
| Sig. | | 1.000 | 0.994 | 1.000 |
Results
The pull out values for the mini implants with different thread designs were noted as observed in the auto instrument software. The mean in the pull out tests ranged from 13.45 N (trapezoidal) to 61 N (trapezoidal fluted) as shown in [Table/Fig-4]. The Tukey post-hoc tests showed a statistically significant difference of 34.5 Newton between the control group and the trapezoidal fluted group [Table/Fig-5].
Discussion
One of the most important aspects of successful orthodontic treatment is catering to anchorage needs based on individual patients’ requirements. Mini implants are used in the current scenario to provide absolute anchorage. Stability of the mini implants forms the core for successful orthodontic treatment using mini implants. The design and stability of orthodontic mini implants are inter-related. Implant body surface area, cross-sectional area, and volume, the insertion torque, stability, and stress are related to the thread size and profile. Tighter pitch near the head and larger diameter of the mini implant ensure better primary stability [16,24].
Thread shape is one of the important factors to be taken into account when a mini implant, which will be subject to early loading, is designed. Thread shape factor is defined as the ratio between the thread depth to the pitch of the screw. The thread shape factor is influenced in a relation such that mini implants with smaller pitch and greater depth show greater pull out strength in synthetic materials mimicking bone [19,25-27].
In this study, the mini implants were tested for stability using forces applied perpendicular to the surface of the synthetic polyurethane foam block. This was done because angulating the mini implant to the bone block has an effect on the pull out strength as it ensures greater surface area of the mini implant in contact with the foam block [27]. According to Devlin H et al., the density of posterior maxilla, being 0.31 gm/cc, is considered least among all the sites for implant placement [28]. The density of the polyurethane foam block (0.20 gm/cc or 12.5 pcf) used in this study can be deemed to mimic the worst possible clinical scenario. Previous in vitro studies by Gracco A et al., and Alrbata RH et al., have used two layered foam blocks of greater densities (30 to 50 pcf) [19,27].
There are several techniques for evaluating the stability of mini implants. The non invasive methods, such as radiographic analysis, finite element analysis, percussion test, pulsed oscillation waveform, impact hammer method and resonance frequency analysis, are those wherein the bone implant interface is not disturbed. The invasive methods include histologic and histomorphometric technique, cutting torque resistance analysis, reverse/removal torque value, insertion torque analysis and pull out test.
According to Salmoria KK et al., pull out tests are more efficient (easier to show difference) than insertion torque analysis and hence, they are more commonly used for evaluating the different designs in mini implants [29]. Hence, in this study, insertion torque analysis was not done and only the pull out test was performed for the mini implants with different thread shapes.
For the first time, a trapezoidal fluted thread shaped mini implant was tested for pull out strength and this mini implant showed the highest value of pull out strength (75 N). Trapezoidal thread design with flutes had better primary stability than the control group (reverse buttress). The results of this study also showed that among the mini implants with different thread shapes, the lowest pull out strength was observed in the trapezoidal group.
Previous studies have shown that mini implants with asymmetric thread design (with 45 leading and 90 trailing angles) have shown better pull out strengths [30-32]. In the study by Wu JH et al., the pull out values of the mini implants was in the range of 109 to 139 N/cm [23]. The mean values in the pullout tests in the study by Gracco A et al., ranged from 170 N to 192 N [19]. When comparing with these studies, the mean values of this study were significantly lower (13.5 N to 61 N). This could be attributed to the fact that in the above mentioned studies the foam block used were of considerably higher density or the foam block used was bi-layered (upper layer with higher density and lower layer of the block of lesser density).
Limitation
The key limitation of this study is that only one density of polyurethane foam block was used. Further, in vitro studies with foam blocks of higher densities would be required to check the efficacy of the trapezoidal fluted mini implants. This study could not mimic the clinical environment wherein the stability of the mini implant is influenced by the contact with cortical bone. Hence, pull out tests would be needed to assess how these different thread types will perform when pulled out from foam blocks of varying densities or higher densities (40 pcf-60 pcf).
Conclusion
For the effective use of mini implants in contemporary orthodontics, the thread shape of mini implants is one of the most important factors to achieve ideal primary stability. In this study, trapezoidal fluted mini implants showed the highest pull out strength. This thread design might produce higher primary stability thereby ensuring for better clinical success by the use of these mini implants. Hence, clinicians for routine use of mini implants might favour this thread design during orthodontic treatment. Further studies using FEM analysis and foam blocks of different densities may be required to establish the performance of the trapezoidal fluted design when compared to the other thread designs.
*denotes significant level of significance
[1]. Graber TM, Orthodontics: Principles and practice 1996 3rd edPhiladelphiaSaunders [Google Scholar]
[2]. Kanomi R, Mini-implant for orthodontic anchorageJ Clin Orthod 1997 36:763-67. [Google Scholar]
[3]. Costa A, Raffainl M, Melsen B, Miniscrews as orthodontic anchorage: a preliminary reportInt J Adult Orthod Orthognath Surg 1998 13:201-09. [Google Scholar]
[4]. Kim JW, Ahn SJ, Chang YI, Histomorphometric and mechanical analyses of the drill-free screw as orthodontic anchorageAm J Orthod Dentofacial Orthop 2005 128:190-94. [Google Scholar]
[5]. Carillo R, Buschang PH, Opperman LA, Franco PF, Rossouw PE, Segmental intrusion with mini-screw implant anchorage: a radiographic evaluationAm J Orthod Dentofacial Orthop 2007 132(5):576:e1-6. [Google Scholar]
[6]. Baumgaertel S, Razavi MR, Hans MG, Mini-implant anchorage for the orthodontic practitionerAm J Orthod Dentofacial Orthop 2008 133(4):621-27. [Google Scholar]
[7]. Reynders R, Ronchi L, Bipat S, Mini-implants in orthodontics: a systemic review of the literatureAm J Orthod Dentofacial Orthop 2009 135:564:e1-19. [Google Scholar]
[8]. Kuroda S, Sugawara Y, Deguchi T, Kyung HM, Takano-Yamamoto T, Clinical use of miniscrew implants as orthodontic anchorage: success rates and postoperative discomfortAm J Orthod Dentofacial Orthop 2007 131:09-15. [Google Scholar]
[9]. Miyawaki S, Koyama I, Inoue M, Mashima K, Sugahara T, Takano-Yamamoto T, Factors associated with the stability of titanium screws placed in the posterior region for orthodontic anchorageAm J Orthod Dentofacial Orthop 2003 124:373-78. [Google Scholar]
[10]. Park HS, Jeong SH, Kwon OW, Factors affecting the clinical success of screw implants used as orthodontic anchorageAm J Orthod Dentofacial Orthop 2006 130:18-25. [Google Scholar]
[11]. Moon CH, Lee DG, Lee HS, Im JS, Baek SH, Factors associated with the success rate of orthodontic miniscrews placed in the upper and lower posterior buccal regionAngle Orthod 2008 78:101-06. [Google Scholar]
[12]. Lin JC, Liou EJ, Yeh CL, Evans CA, A comparative evaluation of current orthodontic miniscrew systemsWorld J Orthod 2007 8:136-44. [Google Scholar]
[13]. Motoyoshi M, Yoshida T, Ono A, Shimizu N, Effect of cortical bone thickness and implant placement torque on stability of orthodontic mini-implantsInt J Oral Maxillofac Implants 2007 22:779-84. [Google Scholar]
[14]. Yu WJ, Kyung HM, Torque and mechanical failure of orthodontic micro-implant influenced by implant design parametersKorean J Orthod 2007 37:171-81. [Google Scholar]
[15]. Wilmes B, Ottenstreuer S, Su YY, Drescher D, Impact of implant design on primary stability of orthodontic mini-implantsJ Orofac Orthop 2008 69:42-50. [Google Scholar]
[16]. Kim YK, Kim YJ, Yun PY, Kim JW, Effects of the taper shape, dual-thread, and length on the mechanical properties of mini-implantsAngle Orthod 2009 79:908-14. [Google Scholar]
[17]. Su Y, Wilmes B, Honscheid R, Drescher D, Comparison of self-tapping and self-drilling orthodontic mini-implants: an animal study of insertion torque and displacement under lateral loadingInt J Oral Maxillofac Implants 2009 24:404-11. [Google Scholar]
[18]. Pithon MM, Figueiredo DS, Oliveira DD, Mechanical evaluation of orthodontic mini-implants of different lengthsJ Oral Maxillofac Surg 2013 71(3):479-86. [Google Scholar]
[19]. Gracco A, Giagnorio C, IncertiParenti S, AlessandriBonetti G, Siciliani G, Effects of thread shape on the pullout strength of miniscrewsAm J Orthod Dentofacial Orthop 2012 142(2):186-90. [Google Scholar]
[20]. Sakin Ç, Aylikci Ö, Techniques to measure miniscrew implant stabilityJ Orthod Res 2013 1:05-10. [Google Scholar]
[21]. Haas R, Haidvogl D, Dortbudak O, Mailath G, Part II: Biomechanical findingsClin Oral Implants Res 2002 13:581-86.https://www.ncbi.nlm.nih.gov/pubmed/7ter m=Haas+R%2C+Haidvogl+D%2C+Dortbudak+AO%2C+Mailath+G [Google Scholar]
[22]. Pfeiffer M, Gilbertson LG, Goel VK, Griss P, Keller JC, Ryken TC, Effect of specimen fixation method on pullout tests of pedicle screwsSpine J 1996 21:1037-44. [Google Scholar]
[23]. Wu JH, Wang HC, Chen CM, Lu PC, Lai ST, Lee KT, Pullout strengths of orthodontic palatal mini-implants tested in vitroJournal of Dental Sciences 2011 6:200e-04. [Google Scholar]
[24]. Heidemann W, Gerlach KL, Gro“bel KH, Ko“llner HG, Drill free screws: a new form of osteosynthesis screwJ Cranio Maxillofac Surg 1998 26:163-68. [Google Scholar]
[25]. Migliorati M, Signori A, Silvestrini-Biavati A, Temporary anchorage device stability: an evaluation of thread shape factorEur J Orthod 2012 34(5):582-86. [Google Scholar]
[26]. Chang JZ, Chen YJ, Tung YY, Chiang YY, Lai EH, Chen WP, Lin CP, Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implantsAm J Orthod Dentofacial Orthop 2012 141(3):279-88. [Google Scholar]
[27]. Alrbata RH, Ha DW, Yu W, Kyung HM, Optimal asymmetric thread for orthodontic microimplants: Laboratory and clinical evaluationAngle Orthod 2015 85(4):585-90. [Google Scholar]
[28]. Devlin H, Horner K, Ledgerton D, A comparison of maxillary and mandibular bone mineral densitiesJ Prosthet Dent 1998 79(3):323-27. [Google Scholar]
[29]. Salmoria KK, Tanaka OM, Guariza-Filho O, Camargo ES, de Souza LT, Maruo H, Insertional torque and axial pull-out strength of mini-implants in mandibles of dogsAm J Orthod Dentofacial Orthop 2008 133:790:e15-22. [Google Scholar]
[30]. Carano A, Lonardo P, Velo S, Incorvat¡ C, Mechanical propertles of three different commercially available miniscrews for skeletal anchorageProg Orthod 2005 6:82-97. [Google Scholar]
[31]. Hou SM, Hsu CC, Wang JL, Chao CK, Lin J, Mechanical tests and finite element models for bone holding power of tibial locking screwsClin Biomech 2004 19:738-45. [Google Scholar]
[32]. Tencer AF, Asnis E, Harrington RM, Chapman JR, Asnis SE, Kyle RF, Biomechanics of cannulated and non cannulated screwsCannulated screw fixation: principles and operative techniques 1996 New YorkSpringer:15-40. [Google Scholar]