Serous Microcystic Adenoma of Pancreas: A Case Series from a Tertiary Care Centre in Southern India
K Rajasree Varma1, Saji Francis2, PP Sathi3, C Saikiran Reddy4
1 Senior Resident, Department of Pathology, Government Medical College, Kozhikode, Kerala, India.
2 Associate Professor, Department of Pathology, Government Medical College, Kozhikode, Kerala, India.
3 Professor, Department of Pathology, Government Medical College, Kozhikode, Kerala, India.
4 Senior Resident, Department of Pathology, Government Medical College, Kozhikode, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Rajasree Varma, Government Medical College, Kozhikode-673008, Kerala, India.
E-mail: rajasreevarmak@gmail.com
Serous microcystic adenoma is a rare exocrine tumour of the cystic neoplasm of pancreas seen predominantly in the elderly population. The first patient was a 56-year-old diabetic woman with abdominal pain, constipation and loss of weight since two months. The second patient was a 73-year-old female with complaints of abdominal pain and back pain since one year. The third patient was a 72-year-old diabetic man with complaints of burning sensation in the right lumbar region since two months. Clinical and laboratory examinations were normal. The radiological examinations of the first two patients showed multiloculated cystic lesion in the pancreas and of the third patient was suggestive of islet cell tumour. The histopathological examination of the three patients showed multiple cysts of varying sizes lined by cuboidal epithelium, showing no atypia. All the three patients were diagnosed as serous microcystic adenoma of pancreas. On follow up, all three patients had no recurrence. Serous epithelial neoplasms need to be differentiated from their non-neoplastic counterparts and other neoplastic lesions with cystic changes, in view of the differences in management. Serous microcystic adenomas have excellent prognosis.
Cystic neoplasm, Multiloculated cyst, Whipples resection
Case Series
Serous microcystic adenomas are rare exocrine tumours of pancreas involving 6% of the pancreatic cystic tumours. These tumours are mostly seen in elderly females, especially in the sixth decade. Majority of lesions are associated with diabetes mellitus. Most of the tumours involve the body and tail of pancreas. Preoperative diagnosis is obtained by Contrast Enhanced Computed Tomography (CECT) imaging. Mostly the lesions have a benign course but malignant transformation can rarely occur. We report a case series of serous microcystic adenomas reported in our institute.
Case 1
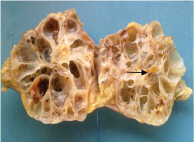
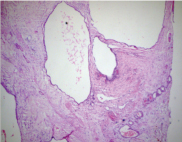
A 56-year-old female patient presented with complaints of abdominal pain, fatigue, loss of weight and constipation since two months. She was a diabetic on oral hypoglycaemic agents since 10 years. Clinical examination was normal. Lab investigations: Haemoglobin (Hb)-12.4g/dl; Total Leucocyte Count (TLC)- 7100/mm3; Platelet count-2.28 lac/ mm3; RBS-139 mg/dl; SGOT-21 IU/ml; SGPT-22 IU/ml; ALP-86 IU/ml. CT scan revealed a multiloculated cystic neoplasm involving the neck of pancreas, measuring 3 x 4 cm, with extension into head of pancreas. The patient underwent median pancreatectomy with pancreatojejunostomy and jejuno-jejunostomy. Gross examination of the specimen revealed a nodulo-cystic mass measuring 5 x 4 x 2 cm. Cut section of the lesion showed a multiloculated cystic lesion filled with brownish fluid and areas of calcification [Table/Fig-1]. Histopathological examination showed a lesion composed of cysts of varying sizes separated by fibrous stroma. The cysts were lined by cuboidal cells and flattened cells [Table/Fig-2]. The patient was discharged after seven days of surgery. She was followed up and was asymptomatic.
Gross examination of lesion showing multiloculated cystic lesion with areas of calcification.
Histopathological examination of lesion showing cysts lined by flattened epithelium (H&E 10X).
Case 2
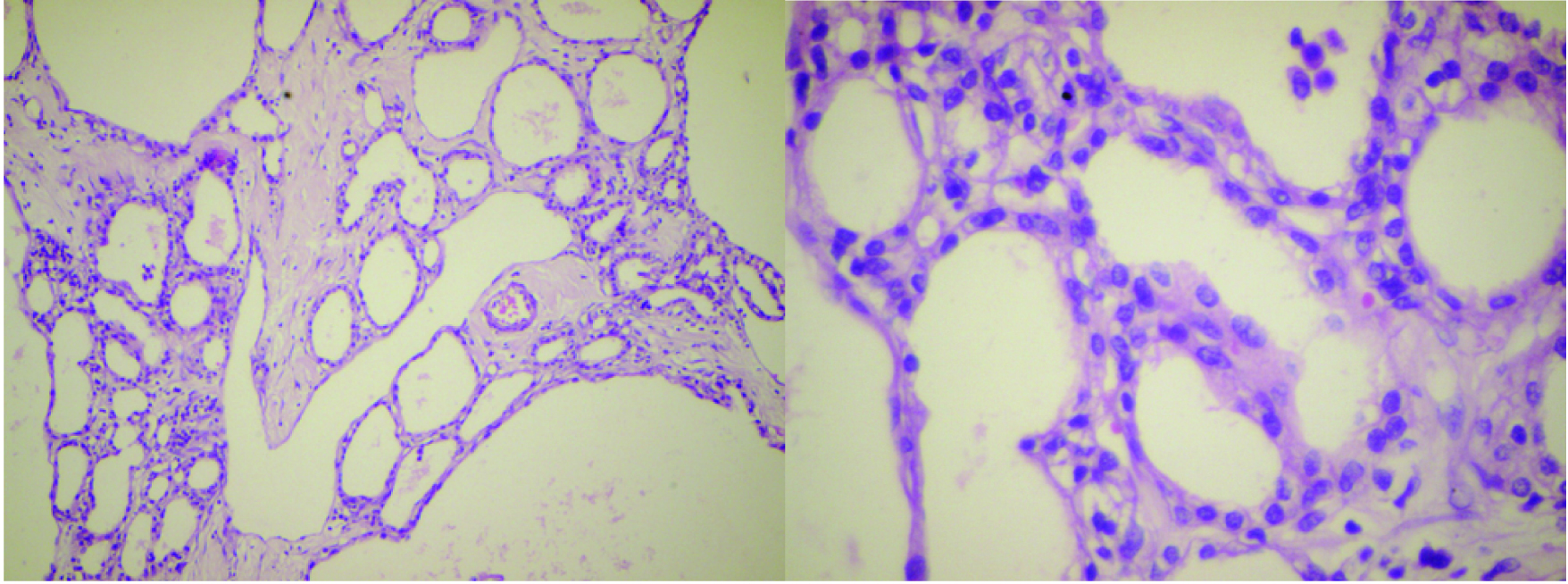
A 73-year-old female patient presented with complaints of abdominal pain and back pain since one year. No history of jaundice, melena or hematemesis. She was on medication for hypertension for four years. Clinical examination was normal except for vague fullness in the abdomen. Laboratory Investigations: Hb-12.8 g/dl; TLC-12200/mm3;Platelet count- 3.34 lac/ mm3; Total bilirubin-0.6 mg/dl; Conjugated bilirubin- 0.1 mg/dl; SGOT- 28 IU/ ml; SGPT-21 IU/ml; ALP-68 IU/ml. CECT scan showed a large 16 x 14 cm heterogeneously enhancing lesion in the body and tail of pancreas. Tail of pancreas was atrophic with mass effect on splenic vein. The patient underwent distal pancreatectomy and splenectomy. Gross examination showed a large cystic mass measuring 17 x 15 x 9 cm. Cut section showed a multiloculated cystic lesion with tiny cystic spaces and a central fibrotic scar [Table/Fig-3]. Histopathological examination showed a multiloculated cystic lesion composed of tiny cysts lined by cuboidal cells showing no atypia [Table/Fig-4a&b]. On follow up, the patient was asymptomatic and had no recurrence.
Gross examination showing multiloculated cystic lesion with a central fibrotic scar.

a) Histopathological examination of lesion showing multiple cysts of varying size (H&E 10X); b) Histopathological examination of lesion showing cyst lined by cuboidal cells with no atypia (H&E 40X).
Case-3
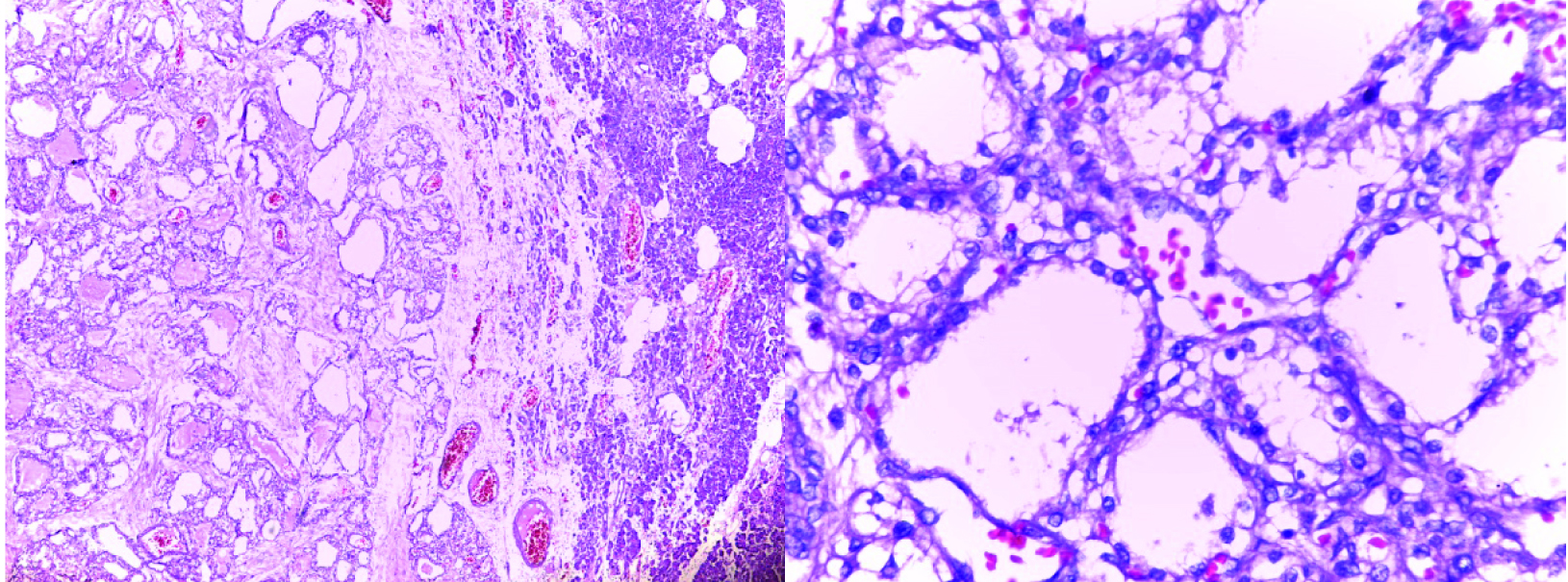
A 72-year-old male patient presented with complaints of burning sensation in the right lumbar region since two months. He was a diabetic on insulin for eight years. No history of loin pain, dysuria, melena or vomiting. Clinical examination was normal. Laboratory investigations: Hb-12.9 g/dl; TLC-9000/mm3; Platelet count-2.38 lac/mm3;Total bilirubin-0.2 mg/dl; Conjugated bilirubin-0.1 mg/dl; SGOT-13 IU/ml; ALP-49 IU/ml. Contrast enhanced CT scan showed a well defined intensely enhancing lesion measuring 2.8 x 1.9 x 1.8 cm involving the body of pancreas. No calcification or necrosis, possibly islet cell tumour. The patient underwent spleen preserving distal pancreatectomy. Gross examination of the specimen revealed a portion of pancreas with a grey brown well circumscribed nodule measuring 3 x 2 x1.7 cm. The lesion on sectioning had a spongy appearance with very tiny cystic spaces [Table/Fig-5]. Histopathological examination of the lesion showed multiple cystically dilated spaces lined by cuboidal epithelium, separated by fibrous stroma. No cellular atypia or necrosis [Table/Fig-6a&b]. The patient was followed up and had no recurrence.
Gross examination showing well circumscribed lesion with tiny cystic spaces.

a) Histopathological examination showing cysts of varying sizes (H&E 10X); b) Histopathological examination of lesion showing cysts lined by cuboidal epithelium (40X).
Discussion
Serous microcystic adenomas are uncommon cystic neoplasms of pancreas constituting around 6% of cystic pancreatic tumours. The World Health Organization defines it as a benign neoplasm composed of numerous small cysts lined by uniform glycogen-rich cuboidal epithelial cells, disposed around a central stellate scar. It accounts for 1-2% of all exocrine pancreatic tumours [1]. Serous cystadenomas show a 3:1 female preponderance with a peak age of incidence in elderly population. About two thirds of the patients present with symptoms secondary to local mass effects, including abdominal pain, jaundice, vomiting and loss of weight [2]. Gao Y et al., had reported a patient with serous microcystic adenoma who presented with recurrent bilateral lower back discomfort [3]. The remaining one third of the cases is incidentally diagnosed during radiological examinations [3].
Serous microcystic adenomas are usually found to be associated with diabetes mellitus. This may be either due to islet cell damage caused by tumour or an incidental finding in the elderly age group [4]. Majority of serous microcystic adenomas occur in the body and tail of pancreas. Association with Von Hippel Lindau syndrome was found in a study done by Vortmeyer AO et al., [5].
Radiologically serous adenomas have three typical morphological patterns- polycystic, oligocystic and honey comb pattern [6]. In the polycystic pattern, there are multiple cysts each measuring 2 cm or smaller, separated by fibrous septae, which coalesce to form a central scar. In the oligocystic pattern, cysts are fewer in number(less than six) but they are larger. In the honeycomb pattern there are numerous tiny cysts which are difficult to be distinguished individually during radiological examination. The polycystic form is the most common pattern. Apart from these, some tumours may show atypical radiological features like multiple septations, wall enhancement or calcification and mural nodules or papillary projections [7].
If radiological examinations cannot reliably differentiate serous microcystic tumours from other cystic lesions, then Endoscopic ultrasound-guided Fine Needle Aspiration (FNA) can be performed. The fluid obtained will be scanty and paucicellular. Carcino Embryonic Antigen (CEA) levels can be assessed in the FNA fluid and value <5 ng/ml is very useful in differentiating serous cystadenomas from mucinous cystic lesions of pancreas [7].
Macroscopically, serous microcystic adenomas are single, well circumscribed cystic lesions of variable size ranging from 1-25 cm. The tumour has a spongy appearance on cut section. The lesion is composed of multiple tiny cysts of variable sizes, separated by fibrous septae coalescing to form central stellate scar [8]. In histopathology sections, cysts are lined by cuboidal or flattened epithelial cells showing minimal atypia and contain intracytoplasmic glycogen [9].
In Immunohistochemistry, the cells are positive for cytokeratin 7, 8, 18 and 19, focally positive for CA 19-9, Cam 5.2, neuron specific enolase,α inhibin and mucin 6 [10]. However, immunohistochemical studies are not routinely done as the radiological and histopathological studies can accurately provide the diagnosis.
The cystadenomas almost always have a benign course. The malignant transformation is considered only if the tumour shows distant metastases or lympho-vascular or peri-neural invasion [11]. Some cases with malignant transformation also showed nuclear atypia and invasion of adjacent structures. Case reports have documented lymph node, splenic, neural, perineural, stomach, lung, adrenal, peritoneal, and mesenteric invasions [12].
Serous cystic tumours, if smaller than 4 cm, usually do not require surgery. Larger tumours are usually excised to prevent complications like mass effect on adjacent structures, haemorrhage into cyst and gastrointestinal obstruction. The type of surgery depends on the location of the tumour. For tumours in tail of pancreas, distal pancreatectomy is the preferred procedure. However, for tumours on the head and uncinated process, whipples resection is often needed [13,14].
Conclusion
Cystic lesions of pancreas include both non-neoplastic and neoplastic cysts. The predominant cystic epithelial neoplasms of pancreas are serous cystadenomas, mucinous cystic tumours and cystic degeneration in malignant epithelial tumours. Solid variant of serous microcystic adenoma has very tiny cysts and may be mistaken for solid tumours like adenocarcinoma or neuroendocrine tumour. The differentiation of serous cystadenoma from other cystic tumours as well as from non-neoplastic cysts is very important because of the great difference in their management. Serous cystadenomas usually have an indolent course, with very few cases reported to have malignant transformation. Smaller serous tumours usually require only conservative treatment. Excision is usually curative for larger tumours or symptomatic cases.
[1]. Morohoshi T, Held G, Kloppel G, Exocrine pancreatic tumours and their histological classification. A study based on 167 autopsy and 97 surgical casesHistopathology 1983 7:645-61. [Google Scholar]
[2]. Pyke CM, van Heerden JA, Colby TV, Sarr MG, Weaver AL, The spectrum of serous cystadenoma of the pancreas. Clinical, pathologic, and surgical aspectsAnn Surg 1992 215:132-39. [Google Scholar]
[3]. Gao Y, Zhang JP, Zhu P, Serous cystadenoma of the pancreas with atypical clinical manifestations: A case reportMolecular and Clinical Oncology 2016 4(4):584-86. [Google Scholar]
[4]. Yasuhara Y, Sakaida N, Uemura Y, Senzaki H, Shikata N, Tsubura A, Serous microcystic adenoma (glycogen-rich cystadenoma) of the pancreas: study of 11 cases showing clinicopathological and immunohistochemical correlationsPathol Int 2002 52(4):307-12. [Google Scholar]
[5]. Vortmeyer AO, Lubensky IA, Fogt F, Linehan WM, Khettry U, Zhuang Z, Allelic deletion and mutation of the von Hippel-Lindau (VHL) tumour suppressor gene in pancreatic microcystic adenomasAm J Pathol 1997 151:951-56. [Google Scholar]
[6]. Sarr MG, Murr M, Smyrk TC, Yeo CJ, Fernandez-del-Castillo C, Hawes RH, Primary cystic neoplasms of the pancreas: neoplastic disorders of emerging importance—current state-of the-art and unanswered questionsJ Gastrointest Surg 2003 7:417-28. [Google Scholar]
[7]. Khalid A, Brugge W, ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cystsAm J Gastroenterol 2007 102:2339-49. [Google Scholar]
[8]. Choi JY, Kim MJ, Lee JY, Lim JS, Chung JJ, Kim KW, Typical and atypical manifestations of serous cystadenoma of the pancreas: Imaging findings with pathologic correlationAJR Am J Roentgenol 2009 193:136-42. [Google Scholar]
[9]. Goldsmith JD, Cystic neoplasms of the pancreasAm J Clin Pathol 2003 119(Suppl):S3-16. [Google Scholar]
[10]. Kosmahl M, Wagner J, Peters K, Sipos B, Kloppel G, Serous cystic neoplasms of the pancreas: an immunohistochemical analysis revealing alpha-inhibin, neuron-specific enolase, and muc6 as new markersAm J Surg Pathol 2004 28:339-46. [Google Scholar]
[11]. Zhu H, Qin L, Zhongetal M, Carcinoma ex microcystic adenoma of the pancreas: a report of a novel form of malignancy in serous neoplasmsAm J Surg Pathol 2012 36:305-10. [Google Scholar]
[12]. Wu CM, Fishman EK, Hruban RK, Schlott WD, Cameron JL, Serous cystic neoplasm involving the pancreas and liver: An unusual clinical entityAbdominal Imaging 1999 24(1):75-77. [Google Scholar]
[13]. Garcea G, Ong SL, Rajesh A, Neal CP, Pollard CA, Berry DP, Cystic lesions of the pancreas. A diagnostic and management dilemmaPancreatology 2008 8:236-51. [Google Scholar]
[14]. Sahani DV, Saokar A, Hahn PF, Brugge WR, Fernandez-Del Castillo C, Pancreatic cysts 3 cm or smaller: how aggressive should treatment be?Radiology 2006 238:912-19. [Google Scholar]