Lymphangitic Pulmonary Metastasis: A Rare Finding in Gastric Carcinoma
James Benjamin Gleason1, Justin Dolan2, Anas Hadeh3
1 Fellow, Department of Pulmonary and Critical Care Medicine, Cleveland Clinic, Florida, 2950; Cleveland Clinic, Boulevard, Weston, FL 33331, USA.
2 Fellow, Department of Pulmonary and Critical Care Medicine, Cleveland Clinic, Florida, 2950; Cleveland Clinic, Boulevard, Weston, FL 33331, USA.
3 Attending Physician, Department of Pulmonary and Critical Care Medicine, Cleveland ClinicFlorida, 2950; Cleveland Clinic, Boulevard, Weston, FL 33331, USA.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. James Benjamin Gleason, Department of Pulmonary and Critical Care Medicine, Cleveland Clinic, Florida, 2950; Cleveland Clinic, Boulevard, Weston, FL 33331, USA.
E-mail: gleasoj@ccf.org
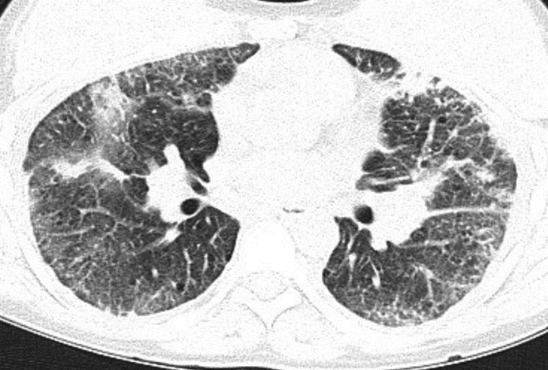
Computed tomography, Interstitial lung disease, Lymphangitic spread
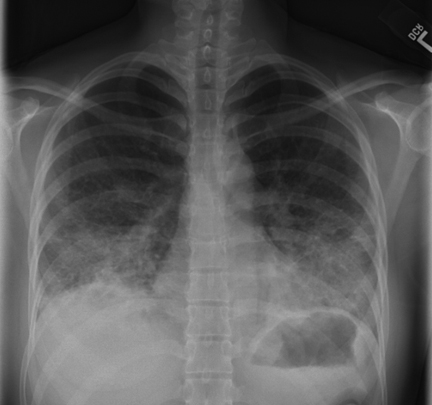
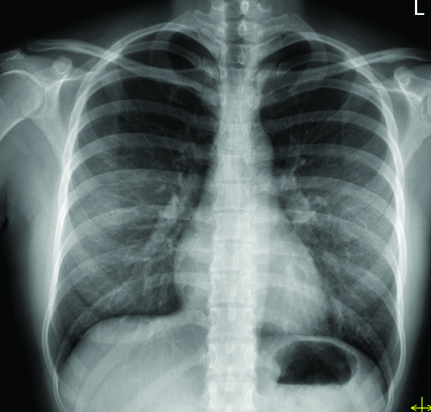
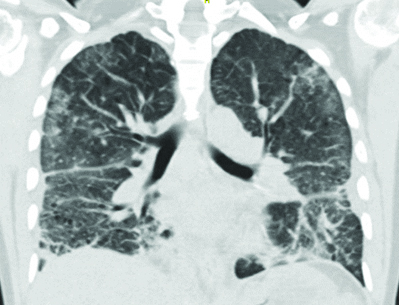
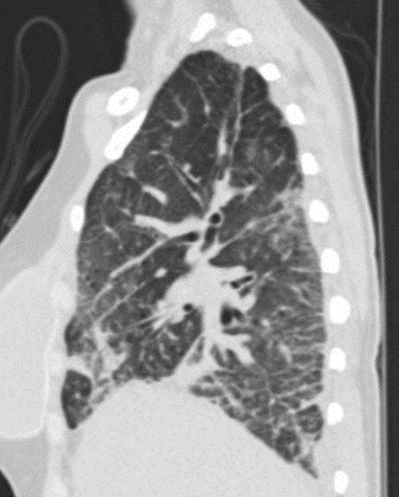
A 39-year-old female presented to Cleveland Clinic Florida Emergency Department with the chief complaint of dyspnoea and discovery of an abnormal chest x-ray performed on arrival. Her chest x-ray demonstrated bilateral mid and lower lung zone opacities [Table/Fig-1] which were new in the last three months when compared to a previous radiograph performed for similar symptoms [Table/Fig-2]. A Computed Tomography (CT) scan of the chest showed bilateral interstitial and ground glass opacities with a peripheral and basilar predominance [Table/Fig-3,4]. There were also thin walled cysts in a peribronchovascular distribution [Table/Fig-5] and borderline mediastinal adenopathy. She reported her dyspnoea and non-productive cough to have been present for three months. Initially a native of Venezuela she moved to the United States of America as a young child. Medical, surgical, and family histories were non-revealing. She had no travel, no pets and had never smoked cigarettes. She was a nail manicurist by trade and had limited exposures to various hazardous chemicals.
Anteriorposterior chest x-ray demonstrating patchy bilateral interstitial opacities in the lower lung fields;
Anteriorposterior chest x-ray performed before the onset of the patients symptoms. Here no interstitial opacities can be seen;
CT scan of the chest, coronal view, demonstrating bilateral patchy peribronchial and interstitial opacities.
CT scan of the chest, sagittal view, demonstrating bilateral patchy peribronchial and interstitial opacities with a basilar predominance;
CT scan of the chest, axial view, again demonstrating diffuse bilateral interstitial opacities with the presence of few small thin walled peribronchovascular cysts.
Infectious, allergic and autoimmune serological evaluations were negative. Respiratory cultures including fungal, mycobacterial and bacterial studies were negative and she was started on a trial of parenteral methylprednisolone 60 mg every eight hours with transition to oral prednisone 40 mg daily for an unclassified Interstitial Lung Disease (ILD). She underwent Video-Assisted Thoracoscopic Surgery (VATS) with wedge biopsy of the right lower lobe which identified the interstitial infiltrates to be lymphangitic spread of poorly differentiated adenocarcinoma confirming a diagnosis of Pulmonary Lymphangitic carcinomatosis (PLS). Upper endoscopy, as part of the systemic evaluation for malignancy, was performed and identified gastric lesions which were biopsy proven to be primary gastric adenocarcinoma.
Pulmonary metastasis is exceedingly rare in gastric carcinoma, representing less than 1% of remote metastasis [1,2]. Of those with pulmonary metastasis, the vast majority show hematogenous spread pattern (53%, multiple variable sized pulmonary nodules or masses), followed by pleural metastasis (35%, pleural thickening or effusion) and least commonly, lymphatic spread comprising only one quarter of the pulmonary metastases [1]. This patient belonged to a low risk population for gastric carcinoma [3] and her diagnosis was unexpected effectively highlighting the vast array of conditions which may mimic ILD.
[1]. Kong JH, Lee J, Yi CA, Park SH, Park JO, Park YS, Lung metastases in metastatic gastric cancer: pattern of lung metastases and clinical outcomeGastric Cancer 2012 15(3):292-98. [Google Scholar]
[2]. Koga S, Takebayashi M, Kaibara N, Nishidoi H, Kimura O, Kawasumi H, Pathological characteristics of gastric cancer that develop hematogenous recurrence, with special reference to the site of recurrenceJournal of Surgical Oncology 1987 36(4):239-42. [Google Scholar]
[3]. Schlansky B, Sonnenberg A, Epidemiology of noncardia gastric adenocarcinoma in the United StatesThe American Journal of Gastroenterology 2011 106(11):1978-85. [Google Scholar]