Adult onset nephrotic syndrome differs from paediatric nephrotic syndrome. The recurrence rates and response to steroids are more variable in adult onset nephrotic syndrome compared to paediatric nephrotic syndrome [1]. With the advent of renal biopsy, it is possible to have a good understanding of nephrotic syndrome in terms of specific diagnosis, prognosis and therapy [2]. Adult onset nephrotic syndrome is broadly divided into primary and secondary types with further subdivisions. However, the nephron reacts to variety of injurious agents with limited number of histopathological patterns of injury. Because of this a clinical syndrome can be associated with several histopathological patterns or single histopathological pattern may be linked to more than one syndrome. It is difficult to differentiate minimal lesions of glomerulonephritis from early membranous glomerulonephritis, IgA nephropathy and Focal Segmental Glomerosclerosis (FSGS) under light microscopy. In such cases, IF helps to straighten the diagnosis. Besides this, it can also enlighten on the pathogenesis of nephrotic syndrome. Some classifications of nephrotic syndrome are based on light microscopy but supplemented by electron microscopy and IF. In the present study, our aim was to determine a role of IF in evaluating definite subtyping and diagnosis of adult onset nephrotic syndrome and attempting clinicopathological correlation.
Materials and Methods
Clinical study and laboratory data:
This study was observational and hospital based. It was done in the Department of Pathology in collaboration with Department of Medicine of BJ Govt Medical College and Sasoon General Hospital, Pune. After clearance from Institutional Ethics Committee and obtaining informed consent, 52 prospectively registered patients of adult onset nephrotic syndrome, during a period of June 2012 to June 2014 were enrolled in the study. Patients with abnormal bleeding time and clotting time were excluded from the study.
Definition of adult onset nephrotic syndrome:
For the purpose of the study, adult onset nephrotic syndrome was defined as proteinuria greater than 3.5g/24 hours, serum albumin <25g/l, clinical evidence of peripheral oedema and patients presenting with these parameters for the first time after 18 years of age.
The patients were thoroughly evaluated clinically with special reference to urinary output, oedema, hypertension, history of diabetes, malaria, tuberculosis, collagen vascular diseases and nephrotoxic drug therapy. Routine urine analysis with microscopic examination of the sediment and urinary total proteins, haemoglobin, platelet count, bleeding time, clotting time, serum urea, serum creatinine were carried out. All patients were investigated with postprandial blood sugar levels. HBsAg, anti hepatitis C and HIV serology was also done. Selected patients with suspicion of systemic lupus erythematosus were investigated for antinuclear antibodies.
All patients were subjected to USG guided percutaneous renal biopsy under local anaesthesia with a 16 gauge biopsy gun, to obtain two cores of renal tissue. Patients were observed for 24 hours for biopsy related complications.
One core of biopsy was preserved in 10% formalin and processed for light microscopy and sectioned at 2 microns thickness and stained with haematoxylin and eosin stain and special stains like gomori methenamine silver, congo red, masson’s trichrome, Periodic Acid-Schiff (PAS) etc. Another core was preserved in phosphate buffer saline for IF and transported in cold box. It was then frozen sectioned at 4 microns on cryostat. IF was done by direct method using antibodies against IgG, IgM, IgA and C3. It was interpreted in terms of intensity, pattern and type of fluorescence. Clinicopathologic correlation was attempted.
Statistical Analysis
Data was expressed using descriptive statistics.
Results
The predominant age group affected was 18-47 years with 41 cases (78.85%) falling in this group. There was male preponderance with 32 males and 20 females with male:female ratio of 1:0.63.
On final light microscopy and IF evaluation the cases of adult onset nephrotic syndrome could be classified into primary and secondary categories. The results of IF examination have been given in [Table/Fig-1,2,3,4,5 and 6].
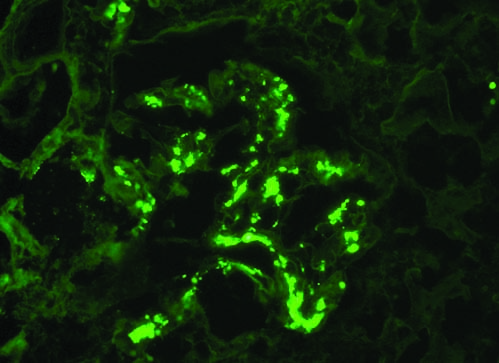
MPGN showing granular deposits - Immunofluorescence - Immunoglobulin G positive (40X).
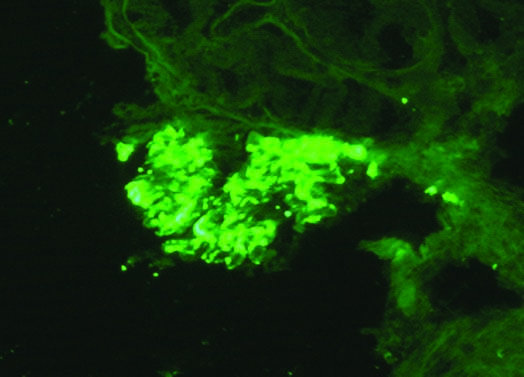
IgA nephropathy: Mesangial positive Immunofluorescence - Immunoglobulin A positive (40X).
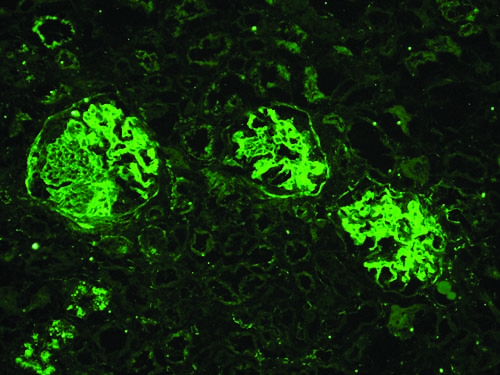
Lupus nephritis: Immunofluorescence Complement 3 positive (10X).
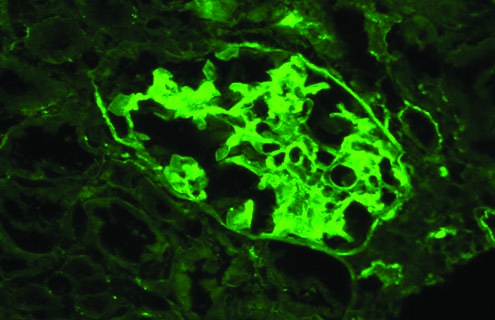
Lupus nephritis: Immunofluorescence - Immunoglobulin G positive (40X).
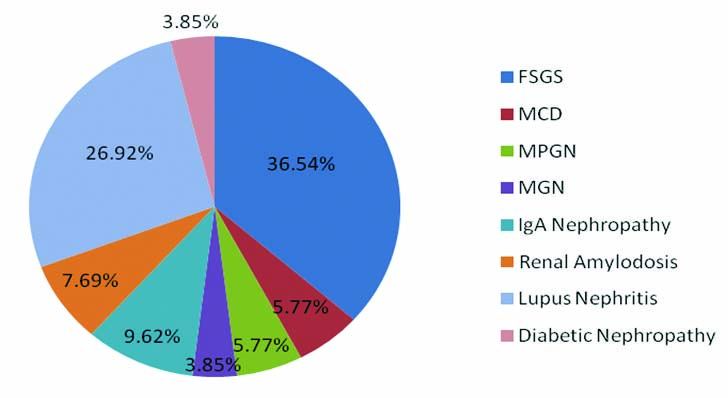
Pie diagram depicting classification of cases of adult onset nephrotic syndrome.
FSGS- Focal Segmental Glomerulosclerosis, MCD- Minimal Change Disease, MPGN- Membranoproliferative Glomerulonephritis, MGN - Membranous Glomerulonephritis.
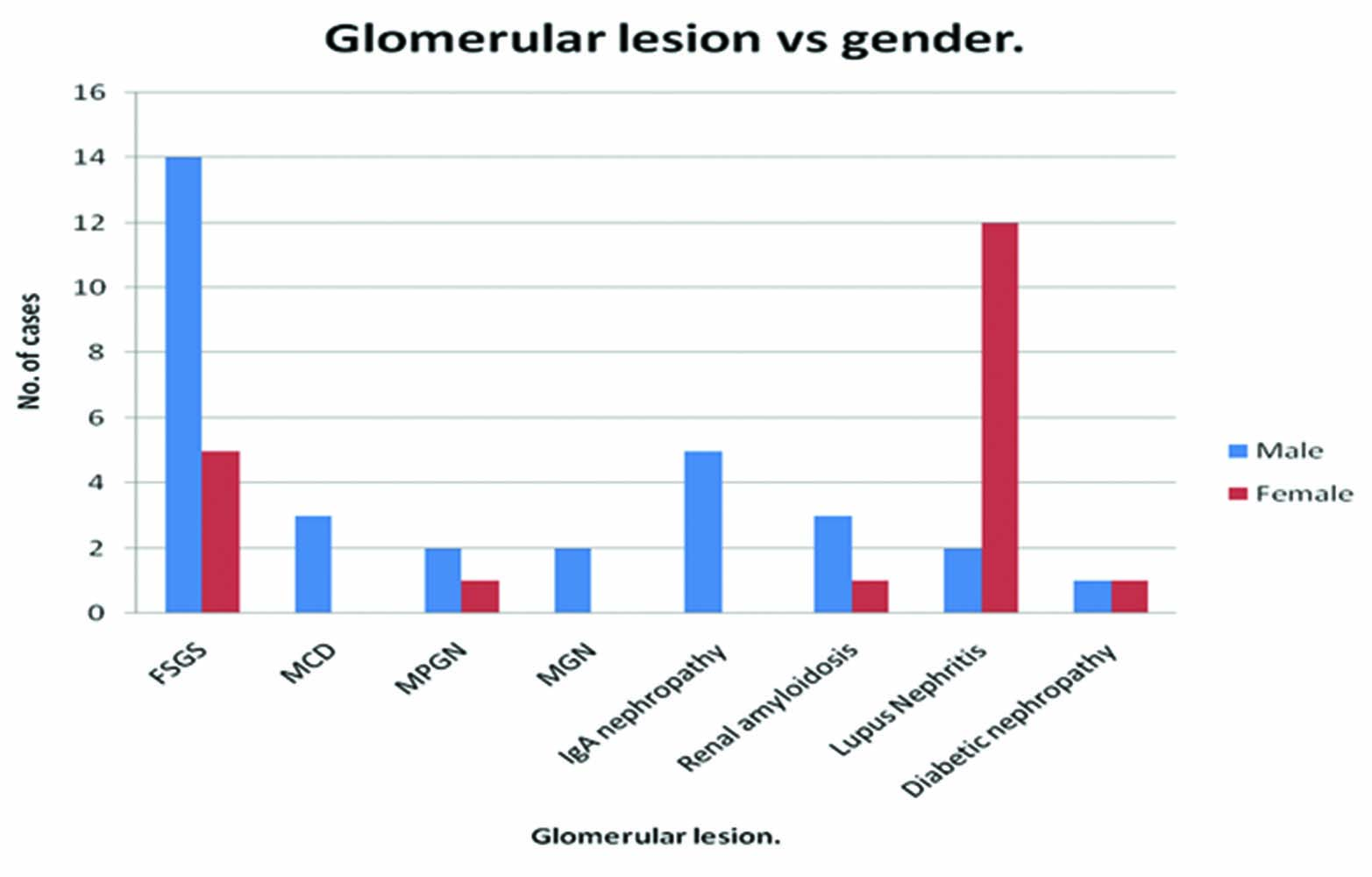
Bar diagram showing gender wise distribution of various glomerular lesions in adult onset nephrotic syndrome.
FSGS- Focal Segmental Glomerulosclerosis, MCD- Minimal Change Disease, MPGN- Membranoproliferative Glomerulonephritis, MGN - Membranous Glomerulonephritis.
There were 32 cases (61.5%) of primary adult onset nephrotic syndrome and 20 cases (38.5%) of secondary adult onset nephrotic syndrome. Among the primary causes, FSGS (n=19) followed by IgA nephropathy (n=5) were the most common types. Among the secondary causes, lupus nephritis (n=14) followed by renal amyloidosis (n=4) were the most common types. Overall comparing the distribution of various subtypes of adult onset nephrotic syndrome FSGS (n=19) and lupus nephritis (n=14) were the most common [Table/Fig-5].
While comparing, gender wise distribution of various glomerular lesions in adult onset nephrotic syndrome, it was found that the most common lesion in males was FSGS while in females was lupus nephritis [Table/Fig-6].
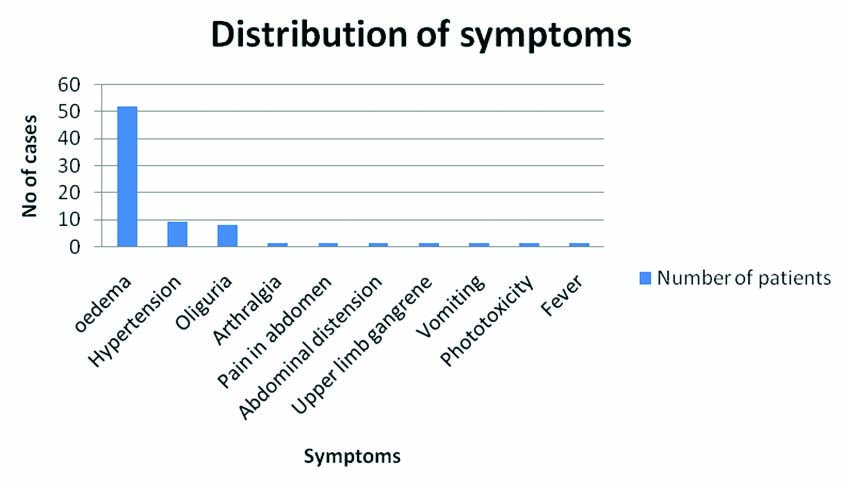
Clinical presentation of various cases of adult onset nephrotic syndrome showed that the most common symptom was oedema (n=52) followed by hypertension (n=9) and oliguria (n=8) [Table/Fig-7].
Bar diagram showing clinical presentation of adult onset nephrotic syndrome.
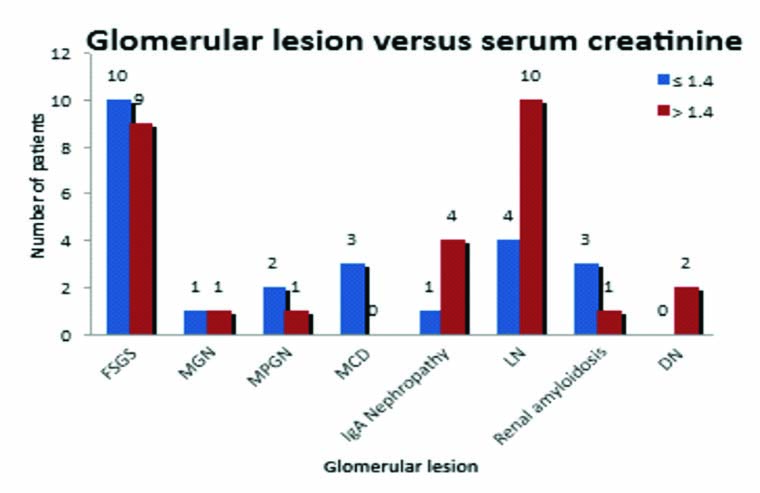
In the present study progession towards renal failure was considered if serum creatinine was >1.4 mg/dl. It was found that all the patients of diabetic nephropathy, 80% cases of IgA nephropathy and 47.36% of patients with FSGS progressed to renal failure [Table/Fig-8].
Serum creatinine in various classes of adult onset nephrotic syndrome.
The DIF was negative in all cases of FSGS, MCD and renal amyloidosis and one case of lupus nephritis and diabetic nephropathy. All cases of MPGN showed IgG positivity which helped in subtyping these cases as Type I MPGN. Out of two cases of MGN, one case was positive for IgG and other for IgM. Also four cases of lupus nephritis showed positivity for all four antibodies used i.e., full house IF. In one case of lupus nephritis and diabetic nephropathy, non specific IF was noted [Table/Fig-9].
Clinicopathological correlation of various classes of glomerulopathies in adult onset nephrotic syndrome.
| IgG | IgM | IgA | C3 | All negative | All positive (full house) |
|---|
| FSGS (n=19) | - | - | - | - | 19 (100%) | - |
| MCD (n=3) | - | - | - | - | 3 (100%) | - |
| MPGN (n=3) | 3 (100%) | 1 (33.3%) | - | 2 (66.6%) | - | - |
| MGN (n=2) | 1 (50%) | 1 (50%) | - | - | - | - |
| IgA nephropathy (n=5) | - | - | 5 (100%) | - | - | - |
| Renal amylodosis (n=4) | - | - | - | - | 4 (100%) | - |
| Lupus nephritis (n=14) | 13 (92.8%) | - | 1 (7.14%) | 1 (7.14%) | 1 (7.14%) | 4 (28.1%) |
| Diabetic nephropathy (n=2) | 1 (50%) | - | - | - | 1 (50%) | - |
FSGS- Focal Segmental Glomerulosclerosis, MCD- Minimal Change Disease, MPGN- Membranoproliferative Glomerulonephritis, MGN- Membranous Glomerulonephritis.
Discussion
The role of IF in evaluation of glomerular diseases most of which present as nephrotic syndrome need not be re-emphasized [3]. Immunologically mediated injury is an invariable mechanism of most of the glomerulopathies and detection of antibody mediated damage of renal tissue can be done by using IF microscopy. There can be two important mechanisms of this reaction. When antibody combines with intrinsic antigen of glomerulus, it imparts linear IF. On the other hand, when there is deposition of either in situ or circulating immune complexes formed with endogenous or extrinsic antigens, it shows a granular appearance [4].
FSGS is a heterogeneous disorder and may be present in primary form, secondary lesion and a complicating lesion. Its aetiology and pathogenesis is controversial. According to one school of thought, it’s a non specific change in broad range of primary and secondary glomerulopathies, while others believe it to be a separate entity or progression of MCD. In the present study, none of the cases of FSGS showed positive IF, thus helping us to differentiate them from IgA nephropathy, which have light microscopic features similar to FSGS. Careful clinicopathologic correlation has shown that none were associated with positive viral serology thereby ruling out possibility of secondary FSGS. A total of eight cases with microscopic haematuria can be attributed to complication of other type of glomerulopathy, particularly part of MCD spectrum and this possibility is most tenable in view of negative IF. Interestingly, 11 out of 19 cases (57.89%) of FSGS showed evidence of progression to renal failure, indicated by either raised serum creatinine (n=7) and/or raised blood urea nitrogen (n=4). Such clinical presentation in view of negative IF, endorses the view that FSGS can be a progression of minimal change glomerulopathy. Alternatively these and other cases can be considered FSGS as a separate entity as clinical features did not allow us to think of other non glomerular tubulointerstitial pathology [2].
There were three cases of MPGN on clinicopathologic correlation and light microscopic features, all belonged to MPGN Type I. IF particularly that for IgG helped in confirming the diagnosis.
There were two cases of MGN. On clinicopathological correlation, both were primary MGN. One of it showed IF for IgG and the other showed for IgM [5].
Multiple or full house IF was seen in four cases, all of which belonged to WHO class IV lupus nephritis. The other significant IF findings noted in lupus cases were presence of coarse granular IF for IgG in 13 cases. Negative IF was noted in one case graded as Grade I lupus nephritis. Diagnosis of lupus nephritis was based on clinicpathologic correlation and light microscopy findings. IF did not help additionally in diagnosis. Interestingly one case was negative for IF; such an occurrence has been mentioned in literature [6]. There were four cases of full house IF positivity which is well known to be associated with Class IV lesion of WHO classification of lupus nephritis. Positive granular IF explains the immune complex deposition which in case of SLE is due to circulating immune complexes.
Cases of renal amyloidosis as expected showed negative IF. Since IF for kappa and lambda chains was not used, these cases were bound to show negative IF.
Only one case out of two cases of diabetic nephropathy showed negative IF. The other case demonstrated ’non specific’ diffuse localisation of IgG which is considered to represent trapping of plasma proteins following mesangial or basement membrane dysfunction.
The frequency of various glomerulopathies in adult onset nephrotic syndrome in various studies is summarized in the [Table/Fig-10] [7-10].
The frequency of various glomerulopathies in adult onset nephrotic syndrome in various studies [7-10].
| AR Reshi et al., [7] | Narasimhan B et al., [8] | Kazi Ji et al., [9] | Rathi M et al., [10] | Present Study |
|---|
| FSGS | 16.89% | 17% | 39.87% | 27.20% | 36.54% |
| MCD | 43.79% | 11.6% | 14.82% | 13.19% | 5.77% |
| MPGN | 2.06% | 3.7% | 4.71% | 15.93% | 5.77% |
| MGN | 13.4% | 9.8% | 26.58% | 21.70% | 3.85% |
| IgA Nephropathy | 1.37% | 8.6% | 2.53% | 1.65% | 9.62% |
| Renal Amylodosis | 0.68% | - | - | 3.30% | 7.69% |
| Lupus Nephritis | 3.1% | 6.5% | - | 6.87% | 26.92% |
| Diabetic Nephropathy | 4.48% | 2.5% | - | 0.28% | 3.85% |
| Others | 14.13% | 29.6% | 7.14% | - | - |
Limitation
The study was conducted on 52 patients and this investigation should be carried out on more patients for better correlation. The other limitations are that it is a single centre based study, retrospective in nature and absence of electron microscopy to correlate our findings in a better way.
Conclusion
To summarize, IF helped in differentiating MCD from IgA nephropathy which had almost normal light microscopic appearance except for mild increase in mesangial cellularity. It also helped in endorsing 19 cases of FSGS to be a progression of minimal change glomerulopathy. We could also conclude that cases of MPGN were of Type 1 MPGN. Thus, IF was of great help in diagnosing exact type of glomerulopathy in adult onset nephrotic syndrome and provided insight in its pathogenesis.
FSGS- Focal Segmental Glomerulosclerosis, MCD- Minimal Change Disease, MPGN- Membranoproliferative Glomerulonephritis, MGN- Membranous Glomerulonephritis.