India is one of the most populous countries in the world. The adolescent population in India constitutes about one fifth of the total Indian population. Adolescent phase is a transitional phase in life and the adolescents are neither child nor adult at this stage and are full of energy, have significant drive and new ideas. The relatively lower death rate and relatively good health status of the adolescents has always been a misleading measure to adolescent health and thus given lesser priorities. In order to respond effectively to the needs of adolescent health and development, it is important to place adolescence in a life-span perspective within dynamic sociological, cultural and economic realities. For this, government of India has started a national programme known as “Rashtriya Kishor Swathya Karyakram” in 2014. However, India as a country does not have an adolescent health policy till date and hence the country requires a national adolescent health policy. The key priorities should include sexual and reproductive health, nutritional problems (both under and over nutrition), substance abuse, mental health, road traffic accidents, intentional violence and non-communicable diseases. In addition to key priorities, the policy draft should include pertinent components such as a preamble, guiding principles, coordinating agencies, monitoring and evaluation, research and documentation components.
Intentional violence, Rashtriya kishor swathya karyakram, Road traffic accidents, Sexual and reproductive health, Substance abuse
Introduction
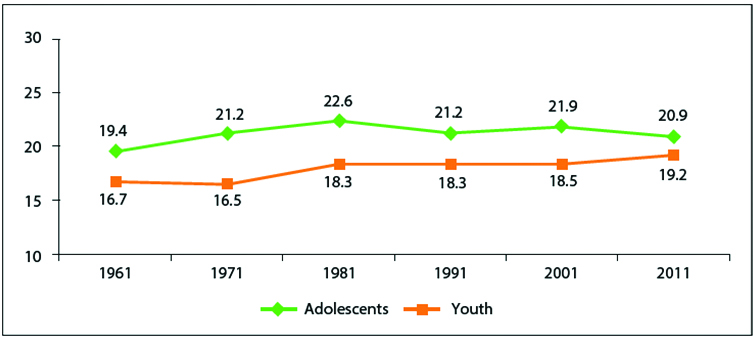
India is one of the most populous countries in the world. Adolescents (10–19 years) constitute about one-fifth of India’s population. Furthermore the young people (10–24 years) constitute about one-third of the total population. In absolute number, as per 2011 census, there are 253 million adolescents in India [1]. This represents a huge opportunity which has the capacity to transform the social and economic fortunes of the country. The large share of adolescent and youth population in India make it necessary that the nation ensures this group becomes a vibrant, constructive force that can contribute to sustainable and inclusive growth of the country. The knowledge, attitude, skills and competencies of today’s youth are essential to whether, and how well, the demographic dividend is successfully leveraged [2]. The [Table/Fig-1] delineates the proportion of adolescent and youth population in India (1961-2011).
Trends in proportion of adolescent and youth population in India (1961-2011).
#Source-Census India, 2011 [1].
Adolescent phase is a transitional phase in life and the adolescents are neither child nor adult at this stage and are full of energy, have significant drive and new ideas. The relatively lower death rate and relatively good health status of the adolescent has always been a misleading measure to adolescent health and thus given lesser priorities. However during the recent days Indian government is putting lot of emphasis on the health and wellbeing of adolescents. At the Summit on the Call to Action for Child Survival, in February 2013, the country launched its new ambitious Reproductive, Maternal, Newborn, Child and Adolescent Health strategy, known as RMNCH+A, to hasten mortality reduction amongst the India’s most vulnerable women and children.
The country has every reason to take the lead in adolescent health as it has a huge 243 million adolescent population, comprising over 21 percent of the country’s total population. Furthermore, India is yet to meet the MDG 4 (under-5 mortality rate) and MDG 5 (maternal mortality rate) [2].
Investments in adolescent health is going to have an immediate, direct and positive impact on India’s health goals and on the achievement of the MDGs, especially goals 1, 2, 3, 4, 5 and 6. Furthermore this, at the same time, will enhance economic productivity, effective social functioning and overall population development. However, a considerable section of adolescent population in India face challenges to their healthy development owing to a number of factors, that includes structural poverty, social discrimination, negative social norms, inadequate education, and early marriage and child-bearing, especially in the marginalized and under-served sections of the population [2]. One of the study revealed that low utilization of maternal health services resulted in low adolescent health outcomes [3]. The lack of adolescent-centric health policy and pertinent interventions results in early child bearing in India especially in the age group of 15 to 19 year [4,5]. Moreover several researchers have identified a wide range of adolescent health issues in India that includes under nutrition and over nutrition, stress and anxiety, consumption of tobacco, alcohol and other substance use, high risk sexual behaviours and intentional violence [6-9] that needs special attention by the government bodies. The [Table/Fig-2] gives a brief description of adolescent population in India.
Adolescent population India.
| Adolescents (10-19 years of age) in india |
|---|
| Population | 253 million |
| Decadal growth (2001-11) | +12.5% |
| Sex ratio | 898 (882) |
#Source-Census India, 2011[1].
In order to respond effectively to the needs of adolescent health and development, it is important to place adolescence in a life-span perspective within dynamic sociological, cultural and economic realities. For this government of India has started a national programme known as “Rashtriya Kishor Swathya Karyakram” in 2014. However, India as a country does not have an adolescent health policy till date and hence the country requires a national adolescent policy [10].
Preamble
Recognizing that
An adolescent is any person between the ages of 10-19 years;
Adolescence is an integral part of life with a value of its own;
Adolescents, both male and female, are not a homogenous group and their different needs need different responses, especially the female adolescents need special attention owing to their complex reproductive changes happening during this period so also the males, as are mostly forgotten;
A long term, sustainable, multi-pronged, integrated and inclusive approach is necessary for the health and development of adolescents of both genders;
Reaffirming that
The phase of adolescence is unique and is a link between childhood and adulthood;
Special interventions are required to diminish or eliminate conditions that affect the health status of adolescents;
All adolescents have the right to receive the health and social services required for the optimum growth and wellbeing;
Families are to be supported through social and healthcare services in caring for the adolescent members of the family;
The Government of India should reiterate its commitment to provide all the necessary health and social services to all the adolescents within its territory and jurisdiction. This should be performed with all necessary requirements such as a competent health system including health infrastructure, workforce, logistics and the supplies which should be accessible, acceptable and affordable to all Indian families.
Guiding Principles
Every adolescent has the fundamental right to health and wellbeing.
The physical, mental, social and spiritual wellbeing of adolescents need to be addressed in totality.
For health and wellbeing no adolescents should be discriminated on the grounds of religion, race, caste, sex, place of birth, class, language, disability, social, economic or any other status.
Family and family environment needs to be taken in to consideration for addressing health problems of the adolescents as the health problems during this stage is very typical [11].
The health services for the adolescent girls should be acceptable, accessible and affordable to the family group.
Possible Implications for Families
Adolescence is the period of rapid sexual and psychological transformations and physical growth which strongly impinge upon the family groups.
Many erratic habits and behaviour adopted during adolescence such as risk taking behaviour, substance abuse, eating habits and conflict resolution can have lifelong impact [11].
The stage of adolescence is definitely the last chance to correct the growth lag and malnutrition.
Adolescent girls constitute a socially disadvantageous class in Indian society, especially in rural areas.
Many of the adolescents, especially the girls, are sexually active however lack of information and skill for self-protection such as low level of information on family planning and usage of contraception [11].
Adolescent girls have simple but wide pervading crucial reproductive health needs that include menstrual hygiene, contraception (including emergency contraception), safety from sexually transmitted diseases and HIV. However in Indian communities, especially in rural areas, communication gap exists with parents and other adults members of the family on these issues.
Furthermore sexuality during adolescent age leads to teenage pregnancy, unsafe abortion, sexually transmitted diseases including HIV/AIDS and social problems. The risk of adverse outcomes is higher in case of adolescent pregnancy [12].
Moreover lack of “connectedness” with parents and other adult members of the families prevent dissemination of health messages and crucial skills leading to adoption of risky behaviour, substance abuse, early sexual debut and sexually transmitted diseases.
Key Priorities
Sexual and reproductive health: The sexual and reproductive health is the most vital and important component in adolescent phase of life. The behavioural pattern established during this phase determines the current health status and the risk of developing chronic ailments in later part of their life [13]. The state should stand committed to ensure the provision of acceptable, affordable and accessible adolescent health services.
The state should take the responsibility to provide health services related to;
Nutritional support to control malnutrition and anemia during this stage.
Information, education and communication services related to menstrual hygiene and use of sanitary napkins.
Peer counseling services for normal physiological changes occurring during this phase which does not require any medical intervention however poses a great concern among the adolescents. These conditions include breast change, breast asymmetry, one sided or both sided breast hypertrophy, non-cancerous breast masses and non-pathological mastalgia etc.
Services related to menstrual dysfunctions such as abnormal length of menstruation, amenorrhea, abnormal vaginal bleeding and menstrual cramps etc.
Services related to counseling and security to some of the social-medical pathologies such as hyper sexuality, adolescent pregnancies, sexual abuse and rape etc., [11].
These are the most commonly occurring problems among the adolescent girls around the world [14,15] and the Indian adolescents are no exception hence the state should give special attention for these adolescent problems.
Nutrition problems: State should provide services to a range of nutritional disorders that include under nutrition, micronutrient deficiency, overweight and obesity. During these days obesity has become an important public health issue among the adolescents [16,17]. This is important as data from large scale survey conducted by the National Institute of Nutrition from 2001 to 2006 revealed an increasing trend of malnutrition among the adolescents which is around half of the population [18,19]. On the other hand obesity and overweight which are other forms of malnutrition are also in increasing trend in India as per the WHO report [20]. This is supported by other studies that India is facing the dual burden of under nutrition and over nutrition [21,22]. Hence the state should take necessary steps to address this dual burden of nutritional problem among the adolescent population.
Substance abuse: Substance abuse is quite common among the urban adolescents that include tobacco, alcohol and other substances, even the injectable. At this juncture of modernity adolescents are highly influenced by adult role models and advertisements regarding these substances and develop a curiosity of trying these substances. The habit of substance abuse and smoking that develops during adolescence is most likely to continue during adulthood stage as well [23-25]. Thus the state should take the responsibility to create awareness and services that can help the adolescents stay away from such harmful practices.
Mental health: It has been estimated that at least 20% of the adolescents are most likely to develop one or the other forms of mental illnesses that include depression, mood disturbances, substance abuse, suicidal behaviours, eating disorders and others [18]. In addition there are other psychological problems such as emotional disturbances, depression, low self-esteem and anxiety, inadequate or excessive secondary sexual development, acne etc. Hence the state should take the responsibility to address such problems in a more appropriate manner as mental illness during this phase of life is a more sensitive issue.
Road traffic accidents: According to National Crime Records Bureau (NCRB) of 2011, 31.3% of road traffic accidents were among youth of 15-29 years of age [26]. Similarly as per the transport research wing of Ministry of Road Transport and Highways (MORTH) out of total road casualties 30.3% were in the age group of 15-24 years [27]. Given this situation the state should take necessary steps to prevent road traffic accidents such as compulsory use of helmets and seat belts, celebration of road safety week etc.
Intentional violence: Interpersonal violence among youth ranging from minor acts of bullying to severe forms of homicide contribute greatly to the burden of premature death, injury and disability; it has not just affected the adolescents but also their families, friends and communities. An average of 565 adolescents and young adults between the ages of 10 and 29 years die each day as a result of interpersonal violence across the world [28].
Non communicable diseases: Non communicable diseases may not be very prominent among the adolescents however their risky behaviour during this stage leads to the development of many non-communicable diseases during adulthood. Consumption of alcohol is linked to more than 60 different health problems and a variety of social issues ranging from domestic violence to diabetes [25]. Furthermore conditions like depression and obesity are closely linked to a number of Non Communicable Diseases (NCDs) and depression in particular linked with suicides. The Health Behaviour Study in Bangalore, India covering nearly 10,000 individuals aged 18 to 45 year from urban, rural, slum and transitional areas reported that 30% had more than five behaviours existing in the same individual [29]. Hence the state should take necessary steps to put a check on these risky health behaviours among the adolescents.
Adolescent labour: In India adolescent labour is an important matter of concern. It has been observed that adolescents are highly exploited in the construction sites, agriculture fields, and small shops and for peddling of drugs and substances. There are many hazardous industries that employ adolescents which compromise their health and hygiene, sexual health and grooming. The adolescents especially from poor and minority groups are paid much less than their adult counterparts. The female adolescents are doubly marginalized in terms of wage and work conditions. In addition they are highly vulnerable for work place violence. Many a time due to legal sanctions the adolescent workers are not the figures in the list of workers which jeopardize their protection from various social security schemes. The law enforcement agencies and welfare agencies in India do not rehabilitate these workers with proper schooling or skill development for up-gradation. The exploitation of adolescent workers leads to lifelong under development in the absence of a strict regulation by the government. Overall physical and mental abuses coupled with meager salary compel them to live with poverty and helplessness. Researchers suggest that there is an urgent need to improve the health among adolescents for reducing the burden of the disease [30]. Indian law allows the under 14 to work in non- hazardous family owned business. However such laws are misused for the benefit of industrialists by tweaking the law. The act also allows children, between 14-18 years of age, to work in hazardous conditions [31]. This is a serious concern for the overall development of adolescents.
Coordinating and Monitoring Agencies
As health in India is a state matter hence the most important strengths and at the same time challenges of coordination and monitoring in health sector is the distribution of responsibility and accountability between the Center and the States. Health being a State subject, the Central government has the accountability to provide central funding – which is about 36% of all public health expenditure and over 50% in some states [32]. Further more disease control and family planning activities are in the concurrent list which could be defined widely. Albeit some states, for instance Tamilnadu, have taken the ownership to become domain leaders and marched ahead in setting the example for others, the central government has the responsibility to rectify uneven development and provide more resources where vulnerability is pronounced. Thus the way forward is to provide equity sensitive resource allocation, strengthening institutional mechanisms for consultative decision-making and coordinated implementation, better management of fiduciary risks, and ensuring capacity building and technical assistance to States.
All the rural and urban elected local bodies would be enabled to provide leadership and participate in the functioning of district and sub-district level institutions. The important ones include Rogi Kalyan Samitis (RKS) and the Village Health Sanitation and Nutrition Committee (VHSNC). Particularly they would be in charge of, and could be financed for implementing a number of preventive and promotive health actions for the adolescents that are to be implemented at the community level.
Research and Documentation
The implementation of adolescent health policy should be supported by a comprehensive and reliable knowledge base on all aspects of the health status and conditions of adolescents. The establishment of such a base would be enabled through adolescent health focused research and documentation, both quantitative and qualitative. A continuous process of indicator-based adolescent health impact assessment and evaluation should be developed. The assessment and evaluation should be carried out on the health status of the adolescents in the country, which should inform policies and programmes for the adolescents at national level.
It is surprising to note that research in the realm of adolescent health is relatively poor in India. Most of the major findings regarding the adolescent health problems come from the national level surveys such as National Family Health Survey (NFHS) [11]. In addition few studies on several [3-9] areas of adolescent health have been carried out in different Indian communities which can be referred while rethinking policy initiatives. A multi country WHO study reports that early and unplanned adolescent pregnancies can result in adverse pregnancy outcomes such as eclampsia, low birth weight, early neonatal death and congenital malformations [33]. A study done in Chennai among the school children revealed that mass media has an adverse impact on food habits which leads to intake of more junk foods and snacks; adolescents preferred to buy food products based on TV commercials and avoided outdoor activities [34]. The suicidal tendency among adolescents is four times more among females than that of the males as reported by one of the studies in Goa [35]. Studies on road traffic accidents reveal that more than one third of the adolescents are at risky behaviour and disobey traffic rules leading to road traffic accidents and deaths as reported by one of the studies in Delhi [36]. Substance abuse is also increasing in different parts of India. A study in Chennai reveals that parental substance abuse increases the chance of adolescent substance abuse [37].
It is clear that India is lagging behind in Adolescent health research and the problem is indeed huge. Thus it becomes imperative in the part of all the stake holders and the Government as well to carry out appropriate research in the realm of adolescent health.
Conclusion
At present there is no specific adolescent health policy in India. Given the magnitude of adolescent population and the variety of problems faced by the adolescent population in India it becomes imperative to bring in to action such a policy which would specifically address the health issues and needs of adolescent population in the country. In addition the following points are significant in order to implement such a policy at national level and can help in evaluating the policy at different level of the health system and community.
Professional and technical competence regarding the program management and implementation need to be developed at national level and at each level of the health system and community.
A satisfactory level of attitude and aptitude is required among the pertinent stakeholders to implement such a policy at national level. Similar level of aptitude and attitude is also required at each level of health system and the community.
The workforce development and capacity building for all aspects of programming, managing, working and caring for the health of adolescents at all levels should be ensured through appropriate selection and well planned capacity development initiatives.
All duty bearers working with adolescents for their health care should be sensitized and oriented on health issues and held accountable for their acts of omission and commission.
#Source-Census India, 2011[
1].
[1]. Registrar General I. Census of India. 2011: provisional population totals-India data sheet. Office of the Registrar General Census Commissioner, India. Indian Census Bureau 2011 [Google Scholar]
[2]. National Health Mission. Ministry of Health and Family WelfareLast accessed on 04/04/2016New DelhiGovernment of Indiahttp://nrhm.gov.in/nrhm-components/rmnch-a/adolescent-health-rksk/rksk-background.html [Google Scholar]
[3]. Singh PK, Rai RK, Alagarajan M, Singh L, Bhutta ZA, Determinants of maternity care services utilization among married adolescents in Rural IndiaPLoS ONE 2012 7(2):e31666 [Google Scholar]
[4]. Reynolds HW, Wong EL, Tucker H, Adolescents use of maternal and child health services in developing countriesInternational Family Planning Perspectives 2006 32(1):6-16. [Google Scholar]
[5]. World Health Organisation. MPS Notes 2008 Geneva, SwitzerlandAdolescent Pregnancy [Google Scholar]
[6]. Sunitha S, Gururaj G, Health behaviours & problems among young people in India: Cause for concern & call for actionThe Indian Journal of Medical Research 2014 140(2):185-208. [Google Scholar]
[7]. Wasnik V, Rao BS, Rao D, A study of the health status of early adolescent girls residing in social welfare hostels in Vizianagaram district of Andhra Pradesh State, IndiaInternational Journal of Collabourative Research on Internal Medicine and Public Health 2012 4(1):83 [Google Scholar]
[8]. Rao VG, Aggrawal MC, Yadav R, Das SK, Sahare LK, Bondley MK, Intestinal parasitic infections, anaemia and undernutrition among tribal adolescents of Madhya PradeshIndian J Community Med 2003 28(1):26-29. [Google Scholar]
[9]. Choudhary S, Mishra CP, Shukla KP, Nutritional status of adolescent girls in rural area of VaranasiIndian J Prev Soc Med 2003 34(1):53-61. [Google Scholar]
[10]. Rashtriya Kishor Swathya Karyakram. Strategy Handbook, National Health MissionLast accessed on 04/04/2016New DelhiMinistry of Health and Family Welfare, Government of Indiahttp://nrhm.gov.in/images/pdf/programmes/rksk-strategy-handbook.pdf [Google Scholar]
[11]. Sivagurunathan C, Umadevi R, Rama R, Gopalakrishnan S, Adolescent health: present status and its related programmes in IndiaAre we in the right direction?Journal of Clinical and Diagnostic Research: JCDR 2015 9(3):LE01-LE06. [Google Scholar]
[12]. National Family Health Survey (NFHS-3) 2005– 06: India: Volume I. International Institute for Population Sciences (IIPS) and Macro International 2007 SeptemberLast accessed on 3rd Jan 2017MumbaiIIPSAvailable from:http://www.rchiips.org/nfhs/NFHS-3%20Data/VOL-1/India_volume_I_corrected_17oct08.pdf [Google Scholar]
[13]. Adolescent Health Services: Missing OpportunitiesLast accessed on 04/04/2016Available from:http://books.nap.edu/openbook.php?record_id=12063&page=1 [Google Scholar]
[14]. Knishkowy B, Schein M, Kiderman A, Velber A, Edman R, Yaphe J, Preventive adolescent health care in family practice: a program summaryThe Scientific World Journal 2006 6(1):619-27. [Google Scholar]
[15]. Richter MS, Mfolo V, The perception of South African adolescents regarding primary health care servicesThe Scientific World Journal 2006 6:737-44. [Google Scholar]
[16]. Katz-Wise SL, Blood EA, Milliren CE, Calzo JP, Richmond TK, Gooding HC, Sexual orientation disparities in BMI among US adolescents and young adults in three race/ethnicity groupsJournal of Obesity 2014 (1):1-8. [Google Scholar]
[17]. Schneider EM, Wilson DK, Kitzman-Ulrich H, George SM, Alia KA, The associations of parenting factors with adolescent body mass index in an underserved populationJournal of Obesity 2013 (1):1-7. [Google Scholar]
[18]. Hyderabad: National Institute of NutritionNational Nutrition Monitoring Bureau. Diet & nutritional status of rural population. 158. NNMB Technical Report. No.21 2002 Last accessed on 03/04/2016Available from:http://www.nnmbindia.org/NNMBREPORT2001-web.pdf [Google Scholar]
[19]. Hyderabad: National Institute of NutritionNational Nutrition Monitoring Bureau. Diet & nutritional status of population and prevalence of hypertension among adults in rural areas; p166. NNMB Technical Report No: 24 2006 Last accessed on J04/04/2016Available from:http://www.nnmbindia.org/NNMBReport06Nov20.pdf [Google Scholar]
[20]. World Health OrganizationYoung people: health risks and solutions. Fact sheet. no. 345 2011 Last accessed on 04/04/2016http://www.who.int/mediacentre/factsheets/fs345/en/index.html [Google Scholar]
[21]. Jeemon P, Prabhakaran D, Mohan V, Thankappan KR, Joshi PP, Ahmed F, SSIP Investigators. Double burden of underweight and overweight among children (10-19 years of age) of employees working in Indian industrial unitsNatl Med J India 2009 22(4):172-76. [Google Scholar]
[22]. Srihari G, Eilander A, Muthayya S, Kurpad AV, Seshadri S, Nutritional status of affluent Indian school children: what and how much do we know?Indian Pediatr 2007 44(3):204-13. [Google Scholar]
[23]. O’Hegarty MM, Pederson LL, Asman KJ, Malarcher AM, Mirza SA, Are adolescent cigarette smokers who use smokeless tobacco more likely to continue smoking in the future than cigarette-only smokers: Results from waves I and II of the adolescent health surveyISRN Public Health 2012 1:1-6. [Google Scholar]
[24]. Dowdell EB, Posner MA, Hutchinson MK, Cigarette smoking and alcohol use among adolescents and young adults with asthmaNursing Research and Practice 2011 1:1-7. [Google Scholar]
[25]. Liang W, Chikritzhs T, Alcohol consumption during adolescence and risk of diabetes in young adulthoodBioMed Research International 2014 1:1-6. [Google Scholar]
[26]. New Delhi: National Crime Records Bureau, Ministry of Home Affairs 2012Accidental deaths & suicides in India 2011 Last accessed on 07/04/2016:317Available from:http://ncrb.nic.in/CD-ADSI2011/ADSI-2011%20REPORT.pdf [Google Scholar]
[27]. New Delhi: Transport Research Wing, Ministry of Road Transport and Highways, Government of India 2012Road accidents in India 2011 Last accessed on 07/04/2016:67Available from:http://morth.nic.in/showfile.asp?lid=835 [Google Scholar]
[28]. World Health Organization; Youth violence and alcohol fact sheetLast accessed on 07/04/2016Available from:http://www.who.int/violence_injury_prevention/violence/world_report/factsheets/ft_youth.pdf [Google Scholar]
[29]. Gururaj G, Isaac MK, Girish N, Subbakrishna DK, Bangalore: National Institute of Mental Health & Neuro Sciences; 2004. Final report of the pilot study establishing health behaviours surveillance in respect of mental health. Report No.: WR/IND HSD 001/G – SE/02/413814:69 [Google Scholar]
[30]. Mokdad AH, Forouzanfar MH, Daoud F, Mokdad AA, El Bcheraoui C, Moradi-Lakeh M, Global burden of diseases, injuries, and risk factors for young people's health during 1990– 2013: a systematic analysis for the Global Burden of Disease Study 2013The Lancet 2016 387(10036):2383-401. [Google Scholar]
[31]. First post. Child Labour Act: Govt allows under-14 children to work in non-hazardous family enterprises May, 13 2015 Last accessed on 01/02/201717(48):41ISThttp://www.firstpost.com/india/child-labour-act-govt-allows-under-14-children-to-work-in-non-hazardous-family-enterprises-2242120.html [Google Scholar]
[32]. Govt of India. National Health Policy draft 2015. Ministry of Health and Family WelfareLast accessed on 10/12/2016http://www.nhp.gov.in/sites/default/files/pdf/draft_national_health_policy_.2015.pdf [Google Scholar]
[33]. Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multi-country studyBJOG 2014 121(s1):40-48. [Google Scholar]
[34]. Priyadarshini R, Jasmine S, Valarmathi S, Kalpana S, Parameswari S, Impact of media on the physical health of urban school children of age group 11-17 yrs in Chennai - A cross sectional studyIOSR Journal of Humanities and Social Science 2013 9(5):30-35. [Google Scholar]
[35]. Pillai A, Andrews T, Patel V, Violence, psychological distress and the risk of suicidal behaviour in young people in IndiaInt J Epidemiol 2009 38(2):459-69. [Google Scholar]
[36]. Sharma R, Grover V, Chaturvedi S, Health-risk behaviours related to road safety among adolescent studentsIndian J Med Sci 2007 61(12):656-62. [Google Scholar]
[37]. Anitha RM, Sathiyasekaran BWC, Mental Health symptoms and substance use among urban school going adolescentsJ. Indian Assoc Child Adolesc Ment Health 2013 9(4):102-35. [Google Scholar]