Post Stroke Psychosis Following Lesions in Basal Ganglion
Shruti Srivastava1, Mukul P Agarwal2, Ankur Gautam3
1 Professor, Department of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
2 Professor, Department of Medicine, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
3 Post Graduate Student, Department of Medicine, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shruti Srivastava, Professor, Department of Psychiatry, University College of Medical Sciences and Guru Teg Bahadur Hospital, Dilshad Garden, Delhi-110095, Delhi, India.
E-mail: srivastava_shruti@hotmail.com
Stroke is the second most common cause of death and fourth leading cause of disability worldwide. Post stroke behavioural manifestations are often not recognized, undiagnosed and hence remain untreated. They may even suffer from misdiagnosis of functional disorders before coming at conclusion of organic pathology. Early diagnosis and prompt treatment helps in lowering the overall morbidity related to stroke and improves quality of life of these patients with rare manifestations. Here, we report two cases of elderly female patients presenting with delusions and hallucinations subsequent to stroke, with lesions in basal ganglia detected on neuro-imaging.
Basal ganglia infarct, Delusions, Organic psychosis
Case Report-1
A 72-year-old female, house wife, living with her son and her daughter-in-law, presented with a history of sudden onset right sided hemiparesis one month prior to presentation. She was treated and later discharged from the medicine department. Later she presented in the Department of Psychiatry GTB Hospital with complaints of fear that somebody wanted to kill her. She was afraid of going outside alone or even with someone. She was not able to concentrate on her daily routine work and had decreased involvement in social activities. She would report seeing images which were not perceived by other people. There was no history of altered sensorium, fever, suicidal tendency or recurrent thoughts of death, emotional liability, obsession and compulsion, palpitations, impending doom, flight of ideas, grandiosity or drug abuse. There was no significant past history of any similar episode or of hypertension, diabetes, old stroke, coronary artery disease. History was given by the patient and information was corroborated with primary caregiver.
On examination she was conscious and oriented. Insight and judgement were impaired. Speech was slurred and there was increased psychomotor activity. She had delusion of persecution and visual hallucinations. Her vitals (blood pressure, pulse, temperature and respiratory rate) were normal. General physical examination was normal. In central nervous system examination power was 3/5 in right extremity without sensory and bowel/bladder involvement. Rest of the CNS examination was normal. Chest, cardiovascular and abdomen examination were also normal. Hindi mental status examination was found to be 28.
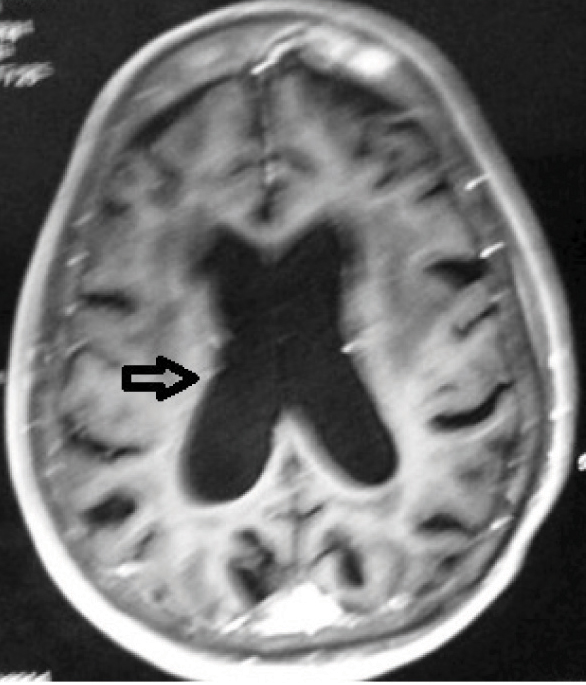
A provisional clinical diagnosis of organic psychosis (ICD- F06) was made. Magnetic Resonance Image (MRI) brain showed lacunar infarct in bilateral basal ganglia, internal capsule and thalamus. Ischemic lacunaes were also noted in bilateral basal ganglia, internal capsule, thalamus and pons. Ventricular system was found to be dilated out of proportion to the atrophy [Table/Fig-1]. She was started on atypical antipsychotic olanzapine 5 mg per day and with psycho-education. Her family was advised to keep her under close observation and support her to overcome the problems she had. On her follow up at two months, improvement of her symptoms was noticed. She was completely free of symptoms after four months of starting treatment.
MRI Brain showing ventricular system dilated out of proportion due to atrophy.
Case Report-2
A 75-year-old female patient with history of stroke was admitted in the Psychiatry ward. Stroke was followed by development of abnormal behaviour like doubting her neighbours without any reason, lack of initiative in doing any work, decreased social interaction and not doing any household work. She would instead be noticed by her son to be muttering to self. When asked by her son, she would explain that there were two different voices who were discussing about the performance of her work in third person. She also explained that at times she could hear a person giving her instructions not to do any work. There was no family history suggestive of psychiatric illness and/or a precipitating stress prior to the development of symptoms.
On mental state examination, she was well clad and kempt, maintained average personal hygiene, had inappropriate affect, second and third person auditory hallucinations, impaired judgment and absent insight with intact higher mental function.
Physical examination revealed high blood pressure recordings. Medicine referral was done to detect the risk factors of stroke. Complete haemogram, fasting and postprandial blood sugar, fasting state, lipid profile, kidney function test, thyroid function, liver function tests were carried out. Dyslipidemia and Hypertension were diagnosed in serial referrals done by medicine consultant. No focal neurological signs or step wise deterioration in the clinical parameters were noted.
Non-Contrast Computed Tomography scan (NCCT) brain was suggestive of lacunar infarct in right lentiform nucleus and clinical diagnosis of organic psychosis (ICD- F06) with hypertension and dyslipidemia was made. Hindi mental status examination score was 26. Clinical Global Impression scale (CGI) [1] was administered by qualified psychiatrist on the day of admission and at weekly intervals thereafter. She was markedly ill at the time of admission and was mildly ill at the time of discharge three weeks later. She was prescribed aripiprazole 5 mg /day which was increased to 10 mg/day after one week and her symptoms got relieved gradually. Amlodepine 5 mg/day and salt restricted, low fat diet, diet on which her blood pressure stabilized. She was also prescribed ecosprin 150 mg/day, atorvastatin 40 mg/day and clonazepam 0.5 mg/day for sleep disturbances.
Discussion
Stroke has been defined by World Health Organization (WHO) criteria as rapidly developing signs of focal (or global) disturbance of cerebral function, leading to death or lasting longer than 24 hours, with no apparent cause other than vascular. This definition includes spontaneous subarachnoid haemorrhage but excludes subdural and extradural haematomas and transient ischemic attacks. Classically it is divided into ischemic and haemorrhagic stroke [2]. Stroke is a global health problem. It is the second most common cause of death and fourth leading cause of disability worldwide [3]. Approximately 20 million people each year will suffer from stroke and of these 5 million will not survive [4]. In developed countries, stroke is the leading cause of disability. Stroke is also a predisposing factor for epilepsy, falls and depression in developed countries [5] and a leading cause of functional impairment, with 20% of survivors requiring institutional care after three months and 15%-30% being permanently disabled [6]. The primary causes of the increased global burden of stroke are related to the increase in stroke risk factors, particularly hypertension, as well as the under detection and under treatment of these risk factors in many developing countries [7-9]. Stroke has substantial impact on the psychological and physical wellbeing of patients [10-13]. Development of clinical signs and symptoms depend on the site of involvement in the central nervous system. Right hemisphere lesions that have connections with limbic system were found to be more strongly associated with mania due to stroke. On the other hand, left frontal or basal ganglia was found to be linked with major depressive disorder [14].
Psychiatric disorders following stroke have been described, most common among them is depression. Other clinical manifestations occurring after stroke like mania, generalized anxiety disorder, emotional lability (psuedobulbar affect) and catastrophic reaction in the form of frustration have been reported. Vulnerability factors like family history of depression, poor social support, social isolation have been shown to increase the risk of onset of psychiatric disorders post stroke [15,16]. In comparison to other clinical manifestations of depression, psychotic symptoms in the form of delusions, hallucinations, agitated behaviour subsequent to stroke are rarely reported. To the best of the knowledge of authors, evidence for patients presenting with post stroke psychosis is based only on case reports [17,18].
In our case after acute infarct in left caudate lobe, basal ganglion and thalamus was followed by psychotic symptoms like delusions, hallucinations and altered psychomotor activity, supporting the diagnosis of organic psychosis that was relieved after antipsychotic treatment. No family history suggestive of psychosis was noted in both the above mentioned cases. However, another previous case report on post stroke psychosis provided genetic evidence for psychosis in a middle aged man with brain lesions at bilateral lentiform nucleus and corona radiate [18]. A recent study reported that three to six months following stroke, half of the patients, including one third with normal or two third with mild cognitive impairment presented with one or more neuropsychiatric manifestations. The most common neuropsychiatric manifestation reported in this study was in the form of mood disturbances followed by behavioural problems, psychosis or euphoria [19].
Conclusion
Current evidence for post stroke psychosis is based on anecdotal case reports. Elderly patient presenting with psychiatric manifestation needs to be actively evaluated for all the known organicity risk factors for stroke such as diabetes, hypertension, dyslipidemia, smoking, ischemic heart disease etc. Appropriate consultation liaison services should be utilised for timely diagnosis and prompt management of a stroke patient presenting with psychiatric symptoms.
[1]. Busner J, Targum SD, The clinical global impression scale. applying a research tool inclinical practice. the clinical global impression scalePsychiatry (Edgmont) 2007 4(7):28-37. [Google Scholar]
[2]. WHO MONICA Project, Principal InvestigatorsThe World Health Organization MONICA Project (Monitoring trends and determinants in cardiovascular disease): a major international collaborationJ Clin Epidemiol 1988 41:104-14. [Google Scholar]
[3]. Strong K, Mathers C, Bonita R, Preventing stroke: saving lives around the worldLancet Neurol 2007 6:182-87. [Google Scholar]
[4]. Dalal P, Bhattacharjee M, Vairale J, Bhat P, UN millennium development goals: can we halt the stroke epidemic in India?Ann Indian Acad Neurol 2007 10:130-36. [Google Scholar]
[5]. Fisher M, Norrving B. The International Agenda for Stroke. 1st Global Conference on healthy lifestyles and non communicable diseases control. Moscow, Apr 28-29, 2011 [Google Scholar]
[6]. Steinwachs DM, Collins-Nakai RL, Cohn LH, Garson A Jr, Wolk MJ, The future of cardiology: utilization and costs of careJ Am Coll Cardiol 2000 35(5Suppl B):91B-98B. [Google Scholar]
[7]. World Health Organization. The global burden of disease: 2004 update. Available at: http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. Accessed January 15, 2015 [Google Scholar]
[8]. Radensky PW, Archer JW, Dournaux SF, O’Brien CF, The estimated cost of managing focal spasticity: a physician practice patterns surveyNeuro Rehabil Neural Repair 2001 15:57-68. [Google Scholar]
[9]. Feigin VL, Lawes CM, Bennett DA, Barker-Collo SL, Parag V, Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic reviewLancet Neurol 2009 8(4):355-69. [Google Scholar]
[10]. de Hann RJ, Limburg M, van der Meulen JHP, Jacobs HM, Aaronson NK, Quality of life after stroke: impact of stroke type and lesion locationStroke 1995 26:402-08. [Google Scholar]
[11]. King RB, Quality of life after strokeStroke 1996 27:1467-72. [Google Scholar]
[12]. Hop JW, Rinkel JE, Algra A, van Gijn J, Quality of life in patients and partners after aneurysmal subarachnoid hemorrhageStroke 1998 29:798-804. [Google Scholar]
[13]. Robinson RG, Neuropsychiatric consequences of strokeAnnu Rev Med 1997 48:217-29. [Google Scholar]
[14]. Robinson RG, Jorge R, Neuropsychiatric aspects of cerebrovascular disease. In: Sadock BJ, Sadock VA, Ruiz P editorsKaplan & Sadock’s Comprehensive textbook Of Psychiatry 2009 9th edPhiladelphiaWolters Kluwer:426 [Google Scholar]
[15]. Schubert DS, Taylor C, Lee S, Physical consequences of depression in the stroke patientGen Hosp Psychiatry 1992 14:69-76. [Google Scholar]
[16]. Parikh RM, Robinson RG, Lipsey JR, The impact of post stroke depression on recovery in activities of daily living over a 2-year follow-up. Arch Neurol 1990 47:785-89. [Google Scholar]
[17]. Bielaski M, Bondurant H, Psychosis following a stroke to the cerebellum and midbrain: a case reportCerebellum Ataxias 2015 2:17 [Google Scholar]
[18]. Abdulla KH, Saini SM, Sharip S, Rahman AH, Psychosis post corona radiate and lentiform nucleus infartionBMJ Case Rep 2015 2015:piibcr2014208954 [Google Scholar]
[19]. Wong A, Lau AY, Yang J, Wang Z, Liu W, Lam BY, Neuropsychiatric symptom clusters in stroke and transient ischemic attack by cognitive status and stroke subtype: frequency and relationships with vascular lesions, brain atrophy and amyloidPLoS One 2016 11(9):e0162846 [Google Scholar]