Enteric Cholestatic Hepatitis with Ascites: A Rare Entity
Samarth Virmani1, Rama Bhat2, Raghavendra Rao3, Savio Dsouza4, Nitin Bhat5
1 Undergraduate Student, Department of Medicine, Kasturba Medical College, (Manipal University), Manipal, Karnataka, India.
2 Professor, Department of Medicine, Kasturba Medical College, (Manipal University), Manipal, Karnataka, India.
3 Assistant Professor, Department of Medicine, Kasturba Medical College, (Manipal University), Manipal, Karnataka, India.
4 Senior Resident, Department of Medicine, Kasturba Medical College, (Manipal University), Manipal, Karnataka, India.
5 Assistant Professor, Department of Medicine, Kasturba Medical College, (Manipal University), Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra Rao, Assistant Professor, Department of Medicine, Kasturba Medical College, Manipal-576104, Manipal, Karnataka, India.
E-mail: ragsmanipal1983@gmail.com
Typhoid fever is a very common illness in developing countries. Patients most often present with a history of fever, vomiting, anorexia, abdominal pain, etc. Rarely there is hepatic involvement due to the disease process. This is a case report of a 26-year-old male who had presented with fever, jaundice and ascites. The widal titres were found to be within normal limits (1:80) however the patient was found to have Salmonella typhi on ascitic fluid culture. The patient was treated with the appropriate antibiotics and was later discharged.
Hepatitis, Peritoneal fluid, Salmonella
Case Report
A 26-year-old male presented to the Emergency Department with complaints of high grade fever of 10 days duration and yellowish discoloration of skin and sclera along with abdominal distension of 4 days duration. There was no associated history of haematemesis, malaena, altered sensorium, pale coloured stools or pruritis. There was no history of drug ingestion or drug abuse, recent blood transfusions, alcohol intake, etc. On examination, his pulse rate was 100 beats/min, blood pressure was 140/90 mmHg, respiratory rate was 18 breaths/min, oxygen saturation was 100% on room air and oral temperature was recorded to be 1010F. On general physical examination, he was found to have icterus and pedal oedema. On examination of the abdomen, there was no tenderness, guarding or rigidity. He was found to have ascites and test for shifting dullness was positive. The liver and spleen were not palpable. All other systems were found to be normal.
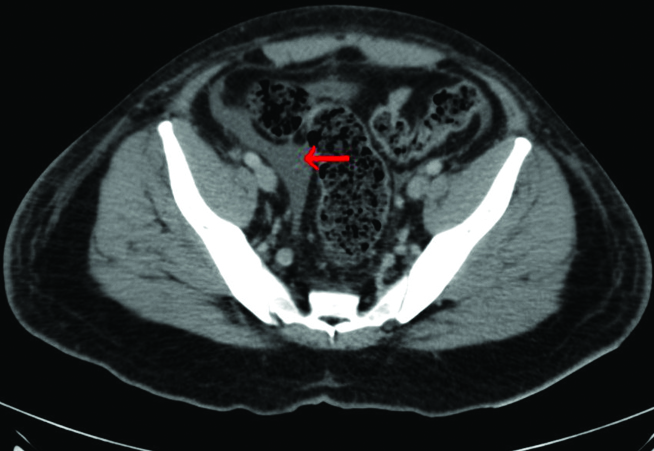
He was investigated for the same. His complete blood picture was normal apart from elevated erythrocyte sedimentation rate (ESR=30 mm). His renal function tests were normal and serum sodium levels were low (Na=129mEq/l). Liver function tests were deranged as the total bilirubin and direct bilirubin were 13.6 mg/dl (normal=0.3-1.9 mg/dl) and 11.4 mg/dl (normal=0-0.3 mg/dl) respectively. The aspartate transaminase and alanine transaminase levels were 78 U/L and 108 U/L (normal= 0-40 U/L) respectively with alkaline phosphatase level of 212 IU/L (normal=44-147 IU/L) and serum albumin of 3.1g/dl. The patient was empirically started on injectable ceftriaxone and metronidazole in view of provisional diagnosis of acute cholecystitis. The blood and urine cultures were sterile and the patient’s serology reports for Hepatitis A, Hepatitis B, Hepatitis C, Malaria, HIV and leptospirosis were found to be negative. Widal titres were 1:80 for O and H antigens. An abdominal ultrasound was done which showed hepato-splenomegaly and mild ascites. CECT scan of abdomen and pelvis revealed the same findings as on ultrasound with few enlarged mesenteric lymph nodes [Table/Fig-1].
CECT abdomen horizontal view showing minimal ascites (red arrow).
A diagnostic ultrasound guided ascitic tap was done which showed protein– 2.8 g/dl, albumin-1.5 g/dl, Serum Ascites Albumin Gradient (SAAG)- 1.6 g/dl, glucose- 110 mg/dl (corresponding random blood glucose– 124 mg/dl), total count- 920 cells/mm3 with neutrophil- 89% and lymphocytes- 11% and the culture of peritoneal fluid was found to be positive for Salmonella typhi, sensitive to ceftriaxone and resistant to ciprofloxacin. Liver biopsy was not done in this patient since he did not consent for the procedure. The patient was continued on injectable ceftriaxone and metronidazole was discontinued. The condition of the patient improved clinically along with improvement of liver function tests. The patient was then discharged after 12 days of hospitalisation.
Discussion
Typhoid fever is a very common infectious disease which is more common in tropical countries. Annually, approximately 21 million illnesses and 216,000 deaths are reported worldwide [1].
The clinical features of typhoid fever are usually non-specific, such as sustained fever, malaise, headache, abdominal pain, anorexia, or vomiting. The lymphoid tissue of the gastrointestinal tract is commonly the pathological site involved in Salmonella infection. Rarely, haematogenous dissemination of the organism or its endotoxin may occur resulting in systemic involvement that has the potential of involving major organs such as the liver, brain, gall-bladder, kidney, lung and heart [2].
The incidence of typhoid hepatitis was approximately 11% as per a study [3]. The factors responsible for the differing severity of hepatic injury in typhoid fever are unknown. It could possibly be due to interplay of the micro-organism factors and the immunity of an individual [4]. It is postulated that the pathophysiological mechanism by which hepatic dysfunction is produced by Salmonella could be either due to direct invasion of microorganisms or by endotoxemia with immune-mediated liver damage [5].
Hepatic involvement may also result in jaundice. The occurrence of jaundice in patients with typhoid fever is roughly 4.8%-17.6% [6]. Biliary canaliculi occlusion by swollen hepatocytes leads to impairment in excretion of bilirubin. This promotes rupture of bile canaliculi which leads to direct reflux of bile into the hepatic sinusoids, resulting in increase in levels of conjugated bilirubin [7].
It is important to recognize Salmonella hepatitis as it can have a similar presentation to acute viral hepatitis. In few cases the extent of liver involvement in typhoid fever may result in a picture indistinguishable from viral hepatitis [8].
Ahmad A et al., studied 254 patients with typhoid fever and found that clinical manifestations of typhoid fever are usually non-specific and clinically indistinguishable from other infections such as malaria and other bacterial and viral infections [9]. In tropical countries, this can prove to be a major problem as jaundice in a patient with fever can be because of malaria, amoebic or viral hepatitis.
A significant rise in serum bilirubin without a significant increase in serum Aspartate Aminotransferase (ALT) is common in typhoid fever but unusual in viral hepatitis as seen in our patient [10]. Moreover, nonspecific prodromal illness precedes the jaundice and the fever tends to subside with the appearance of jaundice in case of viral hepatitis; whereas in typhoid, fever persists despite the appearance of jaundice [10].
Though there are many reports of peritonitis in typhoid fever due to intestinal perforation, but there are very few case reports in international literature highlighting a collection of peritoneal fluid without the evidence of a perforation. A study by Chiu CH et al., conducted on 71 children with typhoid fever reported an incidence of 4% of ascites or pleural effusion [11]. It is also rare to have Salmonellatyphi in ascitic fluid with normal serum widal titres and a negative blood culture as in our patient.
It is of significant importance to reduce mortality rates due to such invasive infections with the use of appropriate antimicrobial agents. The mainstay of therapy of invasive salmonellosis is the use of fluoroquinolones such as ciprofloxacin, however the resistance against quinolones has been steadily increasing [12,13]. Increased rates of clinical and microbiological failure are being seen due to the presence of reduced ciprofloxacin sensitivity. Thus, first line therapy is by giving alternative antimicrobials such as third generation cephalosporins and azithromycin [14]. Such a resistance was also seen in our case, which resulted in the treatment of the patient with ceftriaxone.
Conclusion
A patient with negative viral or bacterial markers for hepatitis may rarely have Salmonella typhi induced hepatitis. It is of utmost importance to get a culture of ascitic fluid despite widal titres or blood culture being negative, in order to prevent missing an important diagnosis.
[1]. Crump JA, Luby SP, Mintz ED, The global burden of typhoid feverBull World Health Organ 2004 82:346-53. [Google Scholar]
[2]. Pramoolsinsap C, Viranuvatti V, Salmonella hepatitisJ Gastroenterol Hepatol 1998 13:745-50. [Google Scholar]
[3]. Durrani AB, Typhoid hepatitisJ Pak Med Assoc 1995 45:317 [Google Scholar]
[4]. Shetty AK, Mital SR, Bahrainwala AH, Khubchandani RP, Kumta NB, Typhoid hepatitis in childrenJ Trop Pediatr 1999 45:287-90. [Google Scholar]
[5]. Khosla SN, Typhoid hepatitisPostgrad Med J 1990 66:923-25. [Google Scholar]
[6]. Kamath PS, Jalihal A, Chakraborty A, Differentiation of typhoid fever from fulminant hepatic failure in patients presenting with jaundice and encephalopathyMayo Clin Proc 2000 75:462-66. [Google Scholar]
[7]. Kaplan LM, Isselbacher KJ, Jaundice: In Braunwald E, Fauchi AS, Kasper DL, editorsHarrisons Principles of internal Medicine 2001 15th edNew YorkMcGrawHillbook Company:249-57. [Google Scholar]
[8]. Mishra D, Chaturvedi D, Mantan M, Typhoid fever and viral hepatitisIndian J Pediatr 2008 75:509-10. [Google Scholar]
[9]. Ahmed A, Ahmed B, Jaundice in typhoid patients: Differentiation from other common causes of fever and jaundice in the tropicsAnn Afr Med 2010 9:135-40. [Google Scholar]
[10]. Nazmul-Ahsan HA, Jalil-Chowdhury MA, Azharr MA, Rafiqeuddin AK, Pitfalls in the diagnosis of jaundiced patient in the tropicsTrop Doc 1995 25:191 [Google Scholar]
[11]. Chiu CH, Tsai JR, Ou JT, Lin TY, Typhoid fever in children: A fourteen year experienceActa Pediatr Taiwan 2000 41:28-32. [Google Scholar]
[12]. Crump JA, Kretsinger K, Gay K, Hoekstra RM, Vugia DJ, Hurd S, Clinical response and outcome of infection with Salmonella enterica serotype Typhi with decreased susceptibility to fluoroquinolones: a United States foodnet multi-center retrospective cohort studyAntimicrob Agents Chemother 2008 52:1278-84. [Google Scholar]
[13]. Wain J, Hoa NT, Chinh NT, Vinh H, Everett MJ, Diep TS, Quinolone-resistant Salmonella Typhi in Viet Nam: molecular basis of resistance and clinical response to treatmentClin Infect Dis 1997 25:1404-10. [Google Scholar]
[14]. Clark TW, Daneshvar C, Pareek M, Perera N, Stephenson I, Enteric fever in a UK regional infectious diseases unit: a 10 year retrospective reviewJ Infect 2010 60:91-98. [Google Scholar]