An Uncommon Case of Cervical Thymopharyngeal Duct Cyst
Xenophon Sinopidis1, Kleopatra Paparizou2, Maria Athanasopoulou3, Antonios Panagidis4, George Georgiou5
1 Assistant Professor, Department of Paediatric Surgery, University of Patras, Patras, Achaia, Greece.
2 Consultant, Department of Pathology, St Andrews Hospital, Patras, Achaia, Greece.
3 Resident, Department of Paediatric Surgery, Karamandaneion Children’s Hospital, Patras, Achaia, Greece.
4 Consultant, Department of Paediatric Surgery, Karamandaneion Children’s Hospital, Patras, Achaia, Greece.
5 Head, Department of Paediatric Surgery, Karamandaneion Children’s Hospital, Patras, Achaia, Greece.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Xenophon Sinopidis, University Hospital of Patras, Patras-26504, Achaia, Greece.
E-mail: xsinopid@upatras.gr
Thymopharyngeal duct cyst is one of the most uncommon benign cervical lesions encountered in the paediatric population. Due to its rarity, it almost always escapes a correct preoperative diagnosis and is usually misdiagnosed as a branchial cyst or lymphangioma. Furthermore, although located at the neck it may present with retrosternal or mediastinal extension.
In this case report here we present a case of a young boy with a right cervical mass, diagnosis of thymopharyngeal duct cyst was confirmed during histopathological examination of the excised specimen. Furthermore, preoperative ultrasonography and MRI did not detect the thin cord and the lower part of the lesion, which rendered operative treatment more demanding. Apropos to these findings, we reflect on the crucial points of awareness that affect the diagnostic and surgical process of this lesion.
Cervical cyst, Children, Paediatric, Thymic cyst
Case Report
A 10-year-old boy presented with a lump on the right cervical region which was observed during the latest trimester of his life, with a progressive increase of size. The patient had a history of cystic fibrosis, a reason for which he visited periodically the Paediatric Respiratory Department, where the cervical swelling was noted at first. On clinical examination a non tender, non inflamed soft mass was revealed at the right side of the neck, anteriorly to the right sternocleidomastoid muscle. The lesion was not affected by swallowing or breathing.
Ultrasonography and MRI showed a lesion of multilocular cystic pattern of a size of 6 x 2 x 2 cm. The lesion was located medially to the right sternocleidomastoid muscle, close to the carotid artery bifurcation and the internal jugular vein, on which it exerted mild pressure [Table/Fig-1]. The radiological morphology and the location of the malformation set a differential diagnosis between a congenital branchial cyst and a lymphangioma. Fine Needle Aspiration Cytology (FNAC) was not performed as the decision was to proceed to radical excision of the mass.
Sagittal view of contrast-enhanced MRI showing the cystic lesion at the right side of the neck.

Surgery under general anaesthesia followed and a right cervical transverse incision was performed over the lesion. The cystic lesion was found anteriorly to the sternocleidomastoid muscle, and was dissected from the internal jugular vein, the carotid artery, and the vagus nerve [Table/Fig-2]. A diving segment of the malformation, which was omitted by the preoperative imaging assay, continued towards the sternal notch, parallel to the route of the sternocleidomastoid muscle. To achieve an effective access to this lower portion, a second lower incision at the base of the neck was performed. Through the second incision, the lesion was excised completely. Its inferior edge ended at the opening of the thoracic cavity. The total length of the excised surgical specimen was 24 cm [Table/Fig-3].
Operative view or the cystic malformation lying on the carotid artery. (left to right)

The excised specimen. The cyst is emptied from its fluid content.

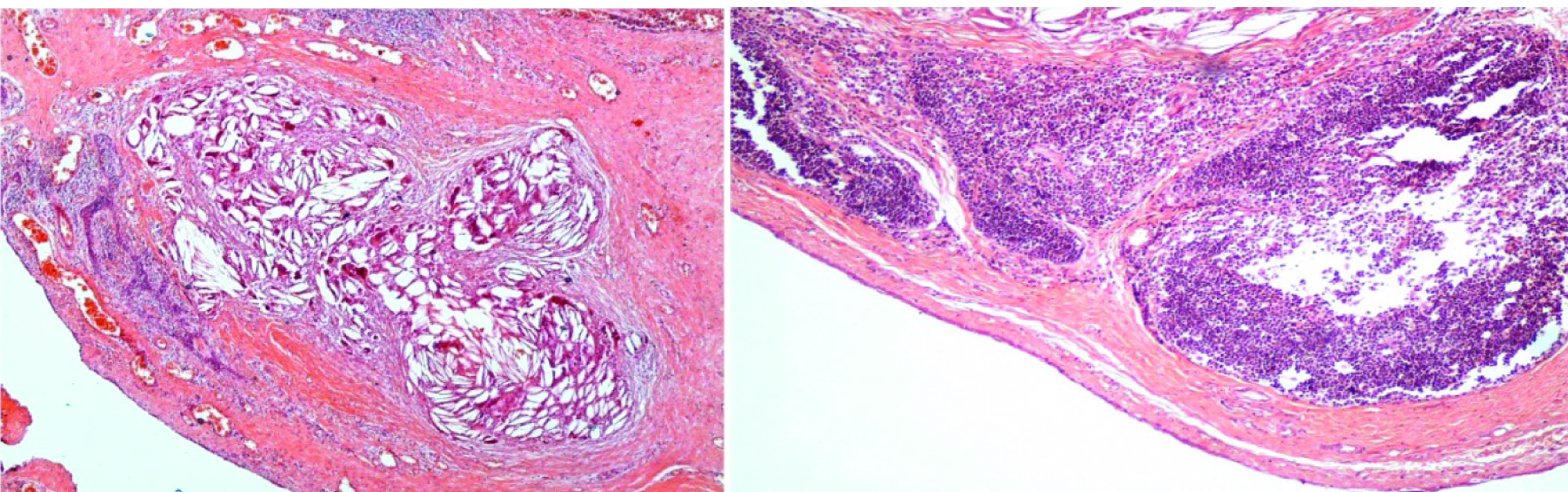
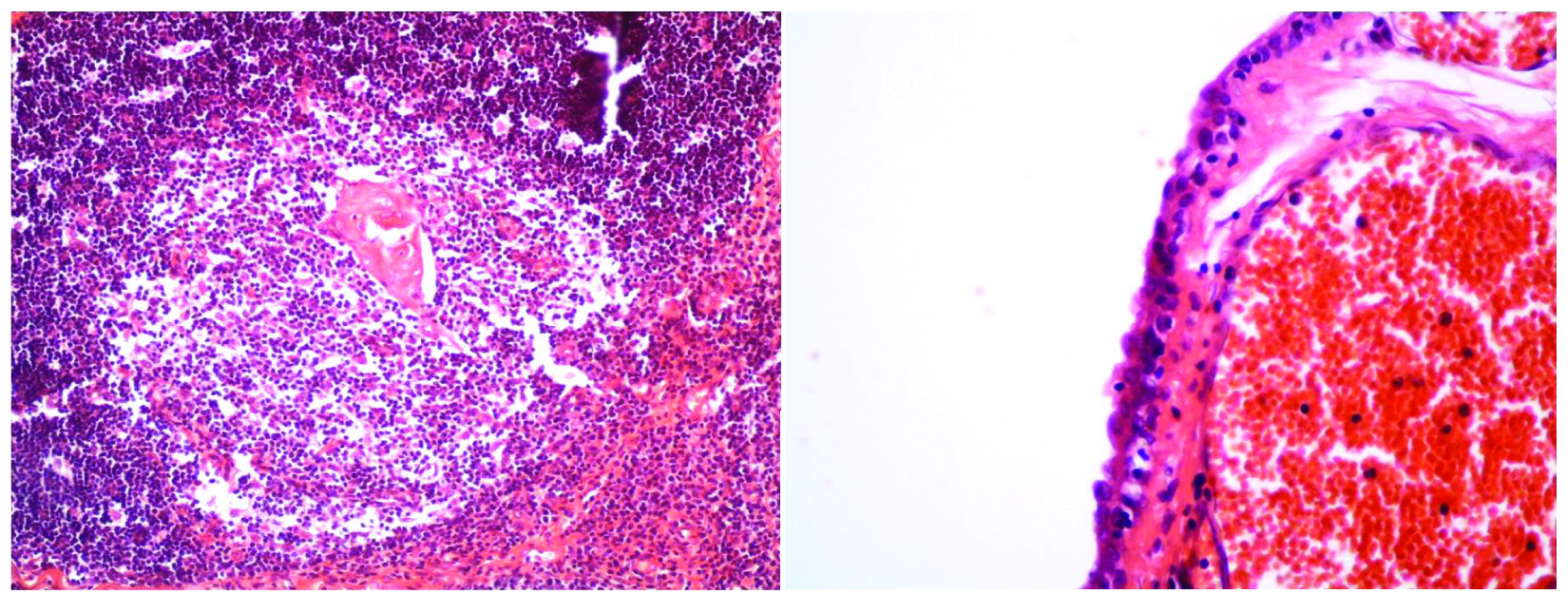
Macroscopically, it consisted of thymus tissue with maximum diameter of 5 cm which was adjoined through an elastic tract with a cyst measuring 4 cm at its maximum diameter. The cyst was unilocular, had fibrous, soft and thin wall and contained watery-serous fluid. Histological examination of the specimen showed the presence of Hassall’s corpuscles, cholesterol granulomas formation, and lymphocytic infiltration. The epithelium of the cyst was mainly cuboidal and partially squamous. No immature thymic tissue was detected. The diagnosis after histological analysis was that of congenital thymopharyngeal cyst [Table/Fig-4a,b,c,d,e].
Cystic wall; cuboidal and partially squamous epithelium. The wall is thickened by blood vessels and lymphocytic inflammatory infiltrate (haematoxylin and eosin stain; original magnification, x4). (left to right)
(b) Cholesterol cleft granulomas beneath the intraluminal wall; consistent mostly of newly formed blood vessels (fibrovascular proliferation) (haematoxylin and eosin stain; original magnification, x 4); (c) The cystic wall contains scattered nests of thymic tissue including small lymphocytes (mature lymphoid tissue) and epithelial cells. (Hematoxylin and eosin stain; original magnification, x 20). (left to right)
(d) A thymic (Hassall’s) corpuscle (haematoxylin and eosin stain; original magnification, x 20); (e) Cuboidal epithelium lining the cystic wall (haematoxylin and eosin stain; original magnification, x 40). (left to right)
Discussion
Thymus is a primary organ of the lymphoid system in childhood, originating from the elongated ventral part of the third or more infrequently fourth pair of pharyngeal pouches which form initially the thymopharyngeal tracts [1]. Epithelial proliferation, lumen obliteration and separation from the pharynx are followed by fusion in the median plane of the upper mediastinum, to form the final organ in the ninth gestational week [1,2]. Failure of the obliteration procedure and preservation of the thymopharyngeal duct, or degeneration of Hassall’s corpuscles within remnants of ectopic thymic tissue, are the main mechanisms of formation of cervical cystic remnants of thymic origin [1-3]. The gland involutes progressively after puberty [1].
Congenital cervical cystic malformations in children can be detected from infancy to late adolescence [1,4,5]. Thymic origin lesions present with a frequency of 1% of the cystic cervical lesions [6,7]. In a 20-year-study on 331 patients under the age of 18 years presenting with cystic masses, only one case was diagnosed as thymic cyst (frequency 0.30%) [8]. During a period of 16 years in three major institutes only nine cases of thymic cysts were reported [1]. Until 1978 fewer than seven cases were reported in literature, a number which seemed to rise to 150 cases in 2004 [1,3,9]. Komura M et al., estimated this number up to more than 80 cases [10].
Clinical presentation of cervical thymic lesions is variable. The most common pattern (80-90%) is that of a benign painless soft and non tender lateral cervical mass which enlarges progressively, with normal overlying skin [1,2,11]. In almost all cases it is unilateral. There is prevalence of the left side of the neck (60-70%), most commonly affecting children at the onset of puberty, with a male predominance of 3:1 [1,3,4]. In exceptional cases it may mimic cervical adenopathy [1]. In 6-10% of patients, pain, dyspnea, dysphagia, vocal cord paralysis, stridor, or dyspnea may present [4,5,9,10]. In 50% of cases the inferior part of the lesion continues as fibrotic cord and descending behind the manubrium into the thoracic cavity and is not clinically palpable or recognizable by imaging [2,9].
Ultrasonography, CT and MRI show the cystic nature of the lesion, yet the diagnosis posed is that of branchial cyst, lymphangioma, and less often dermoid and epidermoid cyst, thyroglossal cyst, or cystic teratoma [7,10]. CT gives important information to distinguish thymic cysts from other congenital anomalies such as lymphangiomas and branchial cleft cysts based on specific anatomic location and appearance. CT also provides information regarding proximity to vital structures that optimizes operative planning. A contrast study shows a homogeneous hypodense mass with minimal rim enhancement when imaging thymic cysts [12,13]. External laryngocele has also been reported as preoperative diagnosis in a child, as the lesion increased in size with Valsalva manoeuvre [14]. Abnormal calcium metabolism may also be associated if there is a functional parathyroid component in a thymic cyst [11]. De Caluwe O et al., summarized the main differences among the uncommon thymic cysts, and the most common cystic hygromas and branchial cleft cysts in terms of incidence, age group, localization, and mediastinal extension [9]. Radical excision of thymic cysts is the treatment of choice [2,9,11]. Caution is necessary because of the proximity with the major cervical vessels. In the cases where the malformation is long and extends towards the sternum, as happened in this case, a second stepladder incision in a lower level is demanded [6]. Recurrence rate after surgery is approximately 2% in cases incompletely resected [15].
Conclusion
Thymopharyngeal cyst presents both diagnostic and surgical complexity. From the diagnostic aspect, as it is rare and frequently regarded as branchial cyst or lymphangioma, it is often the pathologist who must demonstrate a high index of suspicion to implement the correct diagnosis. From the surgical point of view, the surgeon may often confront a previously undiagnosed diving cord segment behind the manubrium into the thoracic cavity, fact that turns surgery to a more demanding level of difficulty.
[1]. Cigliano B, Baltogiannis N, De Marco M, Faviou E, Antoniou D, De Luca U, Cervical thymic cystsPediatr Surg Int 2007 23:1219-25. [Google Scholar]
[2]. Kaufman MR, Smith A, Rothschild MA, Som P, Thymopharyngeal duct cyst. An unusual variant of cervical thymic anomaliesArch Otolaryngol Head Neck Surg 2001 127:1357-60. [Google Scholar]
[3]. Khariwala SS, Nicollas R, Triglia JM, Garabedian EN, Marianowski R, Van Den Abbeele T, Cervical preservations of thymic anomalies in childrenInt J Pediatr Otorhinolaryngol 2001 69:909-14. [Google Scholar]
[4]. Saggese D, Ceroni-Compadretti G, Cartaroni C, Cervical ectopic thymus: a case report and review of the literatureInt J Pediatr Otorhinolaryngol 2002 66:77-80. [Google Scholar]
[5]. Hsu BS, Heatly DG, Wilhelm M, Large cervicothoracic thymic cyst causing prominent airway deviation in a 3-day-old neonateWMJ 2011 110:185-87. [Google Scholar]
[6]. Shenoy C, Kamath MP, Hedge MC, Rao Aroor R, Maller W, Cervical thymic cyst: a rare differential diagnosis in lateral neck swellingCase Rep Otolaryngol 2013 2013:350502 [Google Scholar]
[7]. Bothale KA, Mahore SD, Karmarkar P, Dongre T, Images: Ectopic thymic cyst: A case reportIndian J Pathol Microbiol 2015 58:118-19. [Google Scholar]
[8]. Hsieh YY, Hsueh S, Hsueh C, Lin JN, Luo CC, Lai JY, Pathological analysis of congenital cervical cysts in children: 20 years of experience at Chang Gung memorial hospitalChang Gung Med J 2003 26:107-13. [Google Scholar]
[9]. De Caluwe D, Ahmed M, Puri P, Cervical thymic cystsPediatr Surg Int 2002 18:477-79. [Google Scholar]
[10]. Komura M, Kanamori Y, Sugiyama M, Fukushima N, Iwanaka T, A pediatric case of life-threatening airway obstruction caused by a cervicomediastinal thymic cystPediatr Radiol 2010 40:1569-71. [Google Scholar]
[11]. Gaddikeri S, Vattoth S, Gaddikeri RS, Stuart R, Harrison K, Young D, Congenital cystic neck masses: embryology and imaging appearances with clinicopathological correlationCurr Probl Diagn Radiol 2014 43:55-67. [Google Scholar]
[12]. Kuperan AB, Quraishi HA, Shah AJ, Mirani N, Thymopharyngeal duct cyst: a case presentation and literature reviewLaryngoscope 2010 120(Suppl 4):S226 [Google Scholar]
[13]. Choi YW, McAdams HP, Jeon SC, Hong EK, Kim Y-H, Im J-G, Idiopathic multilocular thymic cyst: CT features with clinical and histopathological correlationAJR 2001 177:881-85. [Google Scholar]
[14]. Ozturk K, Elsurer C, Bulut S, Duran M, Ugras S, Cervical thymic cyst mimicking laryngoceleCase Rep Otolaryngol 2013 2013:839406 [Google Scholar]
[15]. Wagner CW, Vinocur CD, Weintraub WH, Golladay ES, Respiratory complications in cervical thymic cystsJ Pediatr Surg 1988 23:657-60. [Google Scholar]