Case Report
A 43-year-old male patient presented to Department of Radiodiagnosis with the two month history of swelling in right inguinal region and scrotum. On local examination, the swellings were firm and tender. On digital rectal examination, prostate was mildly enlarged.
He underwent an ultrasound examination which revealed metastatic enlarged lymph nodes along the bilateral iliac vessels, bilateral inguinal region and retroperitoneum largest of size 7 x 3.6 x 6.5 cm in right side of pelvis. Bilateral testes were bulky, heterogeneous and showed multiple hypoechoic lesions within, showing raised vascularity on colour doppler. Urinary bladder was normal. Prostate was mildly enlarged measuring 3.8 x 3.5 x 3.5 cm with approx volume of 25 cc. FNAC from the right inguinal lymph node revealed metastatic deposits of the epithelial malignancy.
Further, Computed Tomography (CT) abdomen was done. On plain CT, prostate was heterogeneous and globular with irregular margins measuring 4 x 4.3 x 4.2 cm in Antero-Posterior (AP), transverse and Cranio-Caudal (CC) dimensions respectively with approx. volume of 36 cc.
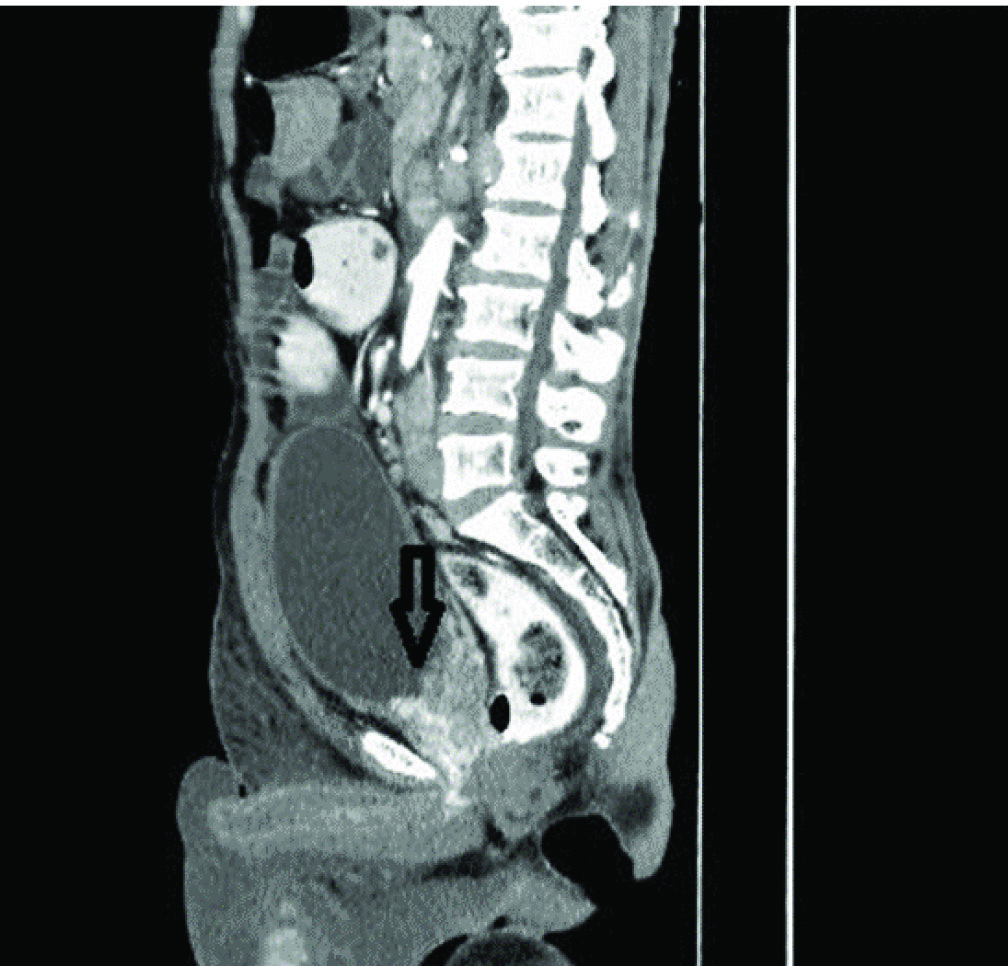
Antero-superiorly, the fat plane between the prostate and bladder base was lost, suggestive of invasion. On either side, prostate was invading bilateral seminal vesicles with no obvious fat plane in between. Posteriorly, the fat plane between prostate and distal rectum was also lost suggestive of likely invasion. On CECT study, Prostate showed significant heterogeneous enhancement [Table/Fig-1].
CECT abdomen (sagittal) showing globular, heterogeneously enhancing prostate with irregular margins. Infiltration of the urinary bladder base (arrow) is also seen.
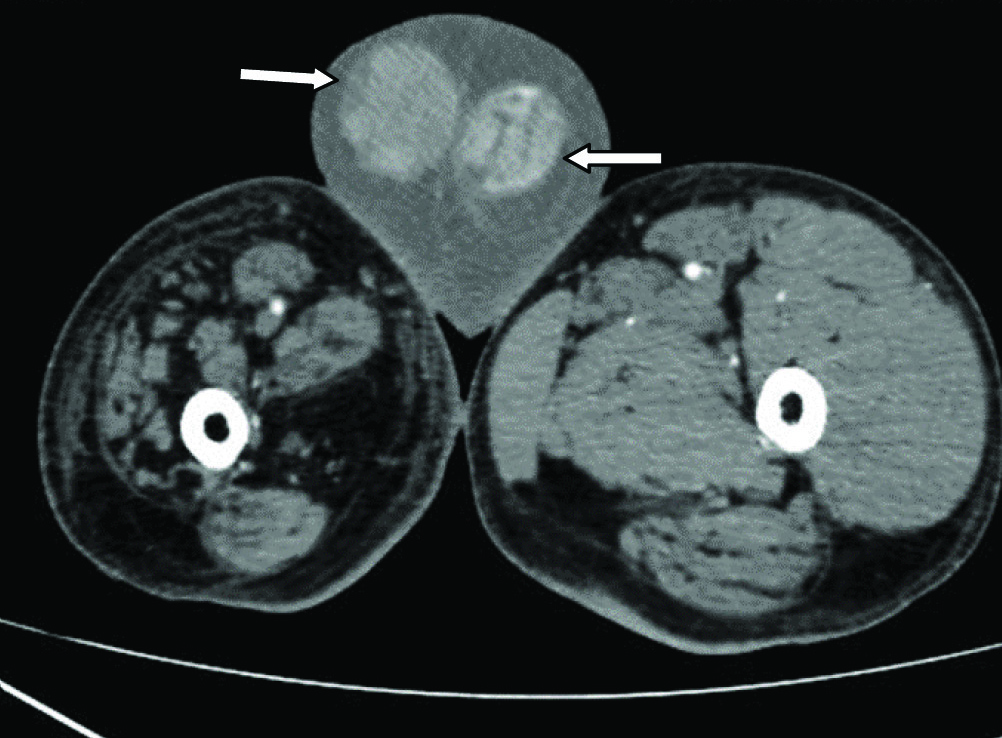
Also, bilateral testes were bulky and heterogeneous. Right testis measured 4.9 x 4.5 x 6.8 cm and left testis measured 5.4 x 4.3 x 8 cm in AP, transverse and CC dimensions respectively. On post contrast study, bilateral testes showed significant heterogeneous enhancement with few non enhancing areas [Table/Fig-2].
CECT abdomen (axial) showing enlarged, heterogeneously enhancing bilateral testis (arrows) with bilateral hydrocele.
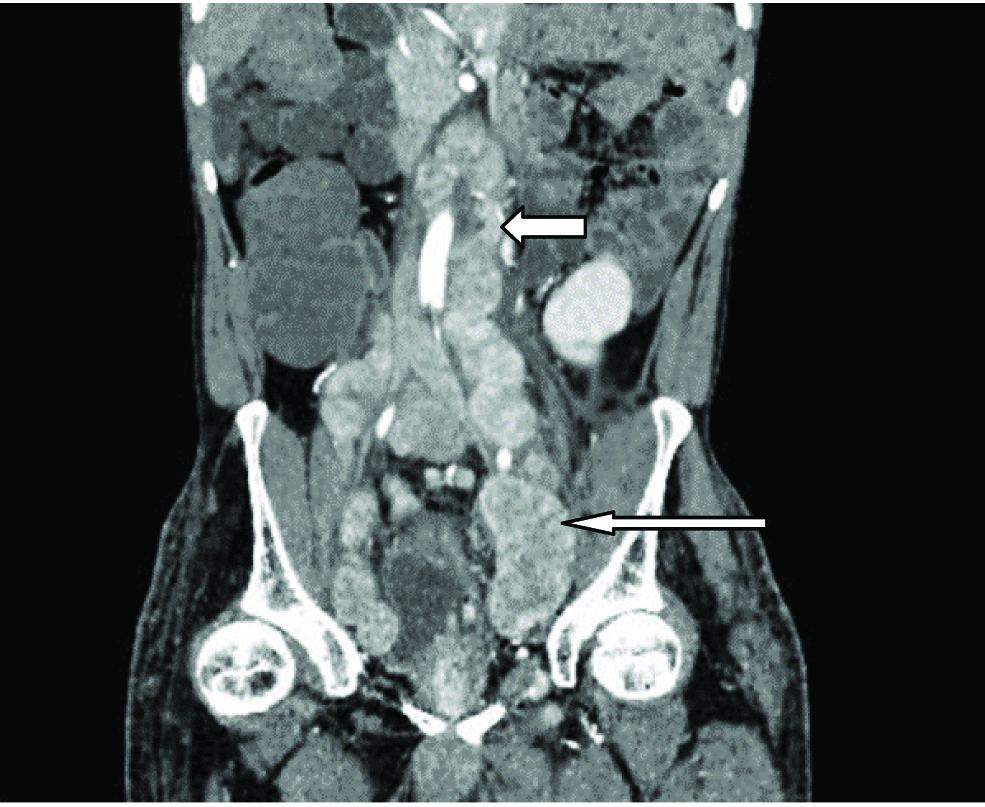
Multiple enlarged, conglomerated, heterogeneously enhancing lymph nodes were also noted in bilateral inguinal region, along the bilateral internal and external iliac vessels, bilateral obturator, pre and para aortic region, surrounding the bladder, aortocaval window, in the retroperitoneal area posterior to aorta, along the mesentry, largest of size 8 x 4 x 6 cm in AP, transverse and CC dimensions in pelvis on left side [Table/Fig-3].
CECT abdomen (coronal) showing multiple enlarged, conglomerated, heterogeneously enhancing lymph nodes along the bilateral internal vessels (long thin arrow), para aortic region (short thick arrow) and surrounding the bladder.
Thus, CECT abdomen revealed primary malignancy of prostate gland invading seminal vesicles, distal rectum and bladder base with secondary metastases in bilateral testes and metastatic conglomerated lymph nodes in bilateral inguinal region, pelvis, retroperitoneum and paraaortic region.
Serum PSA was elevated (> 100 ng/ml). Serum beta-human chorionic gonadotropin and alfa feto-protein levels were within normal limits.
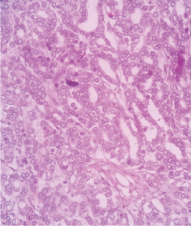
He underwent a transrectal tru-cut biopsy from prostate in the department of surgery, which revealed adenocarcinoma of prostate with Gleason’s score of 4 + 4 = 8 [Table/Fig-4]. A tru-cut biopsy from the right inguinal lymph node was also taken, which on histopathology showed deposits of adenocarcinoma.
(4) Histology of the prostate biopsy showing closely packed glands with little intervening stroma. Nuclei of glands are round to oval hyperchromatic with scanty cytoplasm. Mild to moderate anisonucleosis and pleomorphism, suggestive of adenocarcinoma of prostate (Gleason’s score 4+4=8). Haematoxylin and eosin, ×10 magnification.

The final diagnosis of primary PCa with metastatic deposits in bilateral testes and metastatic lymph nodes in bilateral inguinal region, pelvis, retroperitoneum, paraaortic was made.
Later, bilateral orchiectomy was done. Histopathological analysis revealed solid sheets of tumour cells around and in between the seminiferous tubules with round nuclei with prominent nucleoli and scanty cytoplasm suggestive of metastatic deposits of adenocarcinoma in bilateral testes [Table/Fig-5].
Histopathology of right testis shows sheets of tumour cells with round nuclei with prominent nucleoli and scanty cytoplasm, suggestive of metastatic deposits of PCa. Haematoxylin and eosin, ×10 magnification.
Thus the diagnosis of bilateral testicular metastases from the primary PCa was confirmed which initially manifested as testicular carcinoma in a relatively young patient.
Currently, the patient is on chemotherapy i.e. anti-androgen drug calutide 50 mg once a day for two years and interval follow up of serum PSA level once in two months. The PSA level was decreased to 8 ng/dl after two months of chemotherapy.
Discussion
The approximate incidence of metastases to the testis is 2.5% as seen in various autopsy series. With the exception of the infiltration of leukaemia and lymphoma, secondary neoplasms of the testis are rare, with an incidence of 0.02–2.5% [1]. A 4% of patients with prostate cancer show secondary metastases to the testis, most of these are detected incidentally after orchiectomy or at autopsy [1]. Majority of the secondary metastases to the testis are from distant primary sites such as prostate, gastrointestinal system and lungs [2]. Secondaries to the testes are most often unilateral; however, bilateral metastases are also documented but are rare [2]. Best to our knowledge, the most common metastatic sites of prostate cancer are the pelvic lymph nodes, bone, lung, liver, bladder, and brain, but rarely the testis [2].
The possible hypothesis for spread of PCa to the testis is retrograde venous extension or embolism, arterial embolism, lymphatic extension and endocanalicular spread [1,2].
Bubendorf L et al., studied a cohort of 1589 patients which showed that 35% of cases had hematogenous secondary involving bone (90%), lung (46%) and liver (25%). Only 0.5% (n=3) showed testicular metastases [3].
Lu LY et al., reported 14 cases with metastatic tumour to the testis [4]. Out of total 14, the most common primary was PCa in eight patients with six in unilateral testis and two in bilateral testes. Few cases have been reported with bilateral testicular metastases from already known primary PCa, who were on hormonal therapy and presented with symptoms of enlarged testes [5,6].
Also, few cases of bilateral testicular metastases from known primary PCa which were detected on histopathology after bilateral subcapsular orchiectomy for treatment of the PCa are reported [2,7-9].
In our case, the patient presented with symptomatic testicular metastases and was retrospectively diagnosed as primary PCa on CECT. This is a rare presentation of PCa.
Bilateral testicular Metastases in patients with PCa is a rare occurrence and therefore, its prognostic significance is unknown. Hence, the value of bilateral testicular metastases as a prognostic indicator in PCa cannot be assessed. Nevertheless, it is commonly regarded as a sign of advanced PCa [2].
Conclusion
In middle age male patient presenting with a testicular mass, a possibility of primary PCa with testicular metastases should be kept in mind even though the size of the prostate being normal.
Thus, it was the rare presentation of an occult primary PCa with bilateral testicular metastases in adult patient who presented with right testicular mass.
[1]. Kusaka A, Koie T, Yamamoto H, Hamano I, Yoneyama T, Hashimoto Y, Testicular metastases of prostate cancer: a case reportCase Reports in Oncology 2014 7(3):643-47. [Google Scholar]
[2]. Ho CR, Ng KF, Chen JF, Wu CT, Chuang CK, Pang ST, Metastases of prostate cancer in a single testis presented as a hydrocele: Report of a CaseCurr Urol 2007 1:55-56. [Google Scholar]
[3]. Bubendorf L, Schopfer A, Wagner U, Sauter G, Moch H, Willi N, Metastatic patterns of prostate cancer: an autopsy study of 1,589 patientsHum Pathol 2000 31:578-83. [Google Scholar]
[4]. Lu LY, Kuo JY, Lin AT, Chang YH, Chen KK, Pan CC, Metastatic tumors involving the testesJ Urol Roc 2000 11:12-17. [Google Scholar]
[5]. Fornage BD, Logothetis CJ, Swanson DA, Ro JY, Bilateral testicular metastases from prostate carcinoma: gray-scale and color doppler sonographic findingsJournal of Ultrasound in Medicine 1995 14(3):247-49. [Google Scholar]
[6]. Upchurch E, Khan F, Okeke A, Symptomatic bilateral testicular Metastases from carcinoma of the prostateBMJ Case Rep 2013 2013:2-4. [Google Scholar]
[7]. Kim SO, Choi YD, Jung Il S, Oh KJ, Im CM, Kang TW, Prostate cancer with solitary metastases to the bilateral testisYonsei Med J 2011 52(2):362-64. [Google Scholar]
[8]. Menon S, Gujral S, Bakshi G, Tongaonkar HB, Bilateral testicular metastases from prostatic adenocarcinoma mimicking an intertubular pattern of seminoma and expressing RhammJ Cancer Res Ther 2010 6(1):97-99. [Google Scholar]
[9]. Manikandan R, Nathaniel C, Reeve N, Brough RJ, Bilateral testicular metastases from prostatic carcinomaInt J Urol 2006 13(4):476-77. [Google Scholar]